Lag-screw fixation
1. General considerations
Fracture-dislocations of the distal end segment involve a volar or dorsal coronal fragment. These rare injuries should be treated with open reduction with arthrotomy and lag-screw fixation.
There is a high risk of joint stiffness.
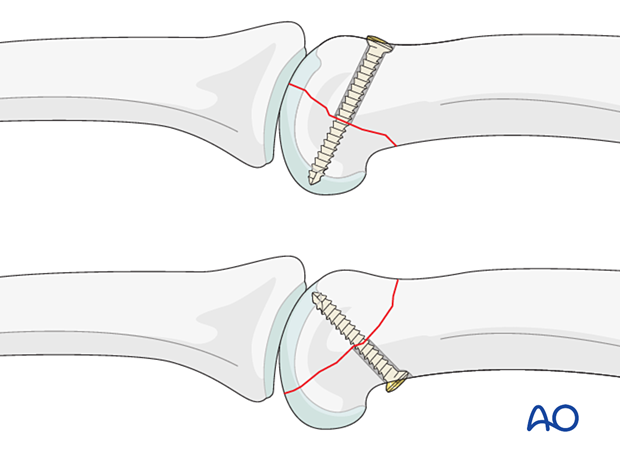
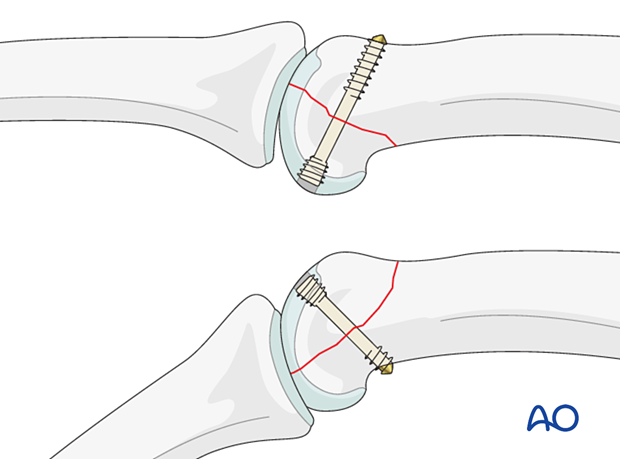
Headless compression screws are inserted through the articular surface.
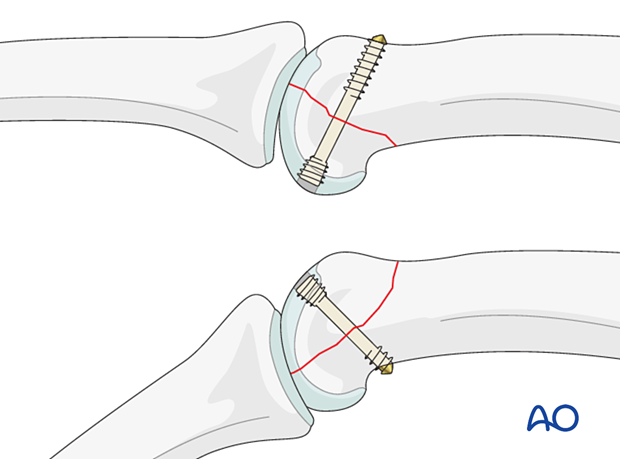
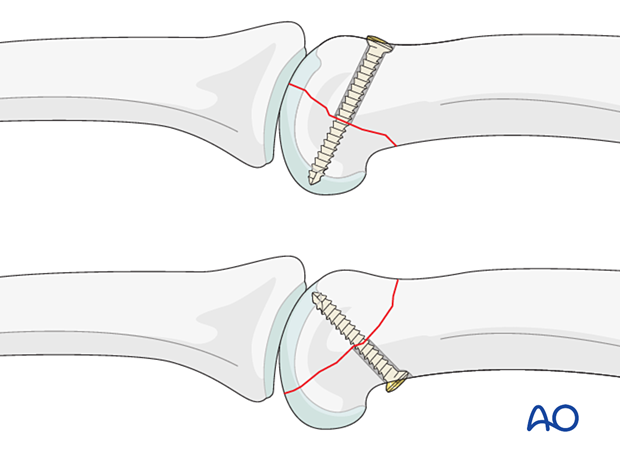
Alternative: cortical lag screw
If headless compression screws are not available, a cortical lag screw may be inserted through the opposite cortex into the subchondral bone.
This has the disadvantage that reduction and fixation may need different approaches.
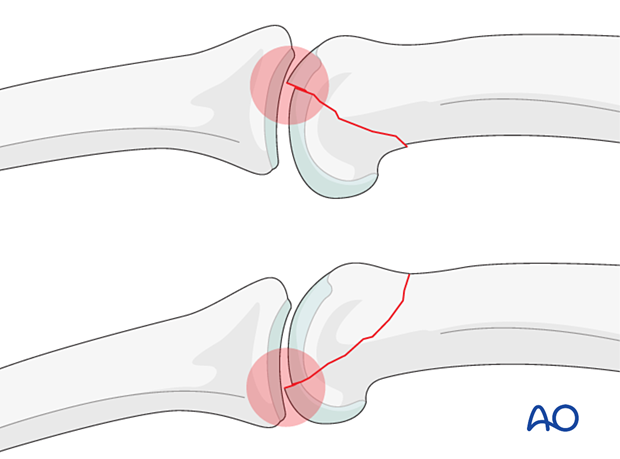
Anatomical reduction mandatory
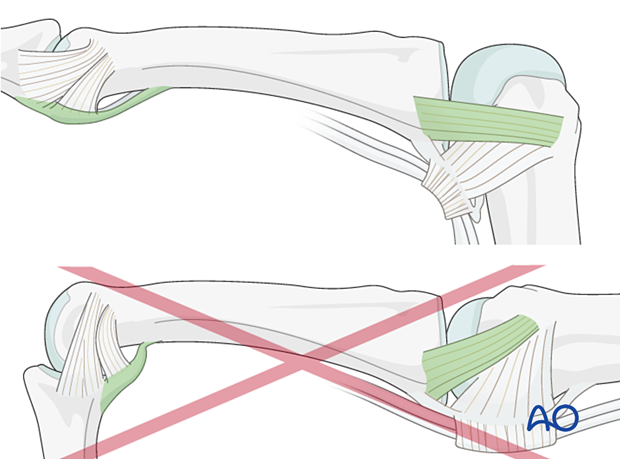
Articular fractures must be reduced anatomically. Otherwise, the articular cartilage may be damaged, leading to painful degenerative joint disease and digital deformity.
This illustration shows how displacement may lead to abrasion and shearing of the articular cartilage and to instability.
Associated ligament injuries
In dislocation of the proximal interphalangeal (PIP) joint, ligaments are often ruptured. These soft-tissue injuries usually heal without reconstruction. However, collateral ligament and volar plate ruptures may need repair (anchor sutures or bone tunnels) if the joint remains unstable after reduction and fixation.
2. Patient preparation
Place the patient supine with the arm on a radiolucent hand table.

3. Approaches
For this procedure, the following approaches may be used, depending on the fracture morphology:
4. Reduction
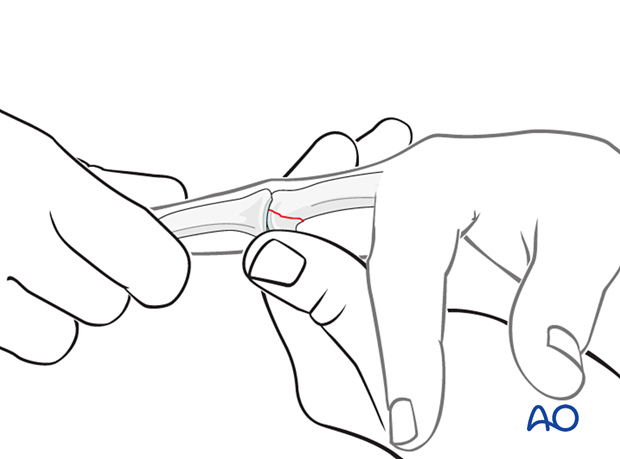
Closed reduction of the dislocation
Dorsal fracture-dislocationApply traction to the finger with the PIP joint in partial flexion and exert dorsal pressure on the displaced condyle to reduce the dislocation.
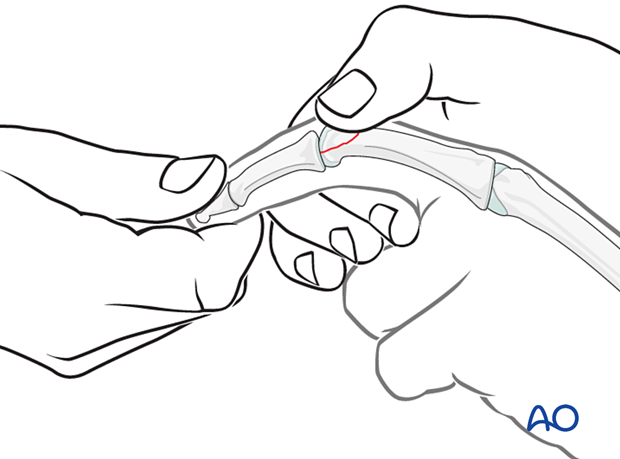
Apply traction to the finger with the PIP joint in extension and exert palmar pressure on the displaced condyle to reduce the dislocation.
Stability assessment
Confirm reduction with an image intensifier and check the joint stability by flexion and extension. This should show congruent movement compared with the adjacent joints.
If congruent reduction cannot be achieved, often due to interposed soft tissue, an open reduction is necessary.
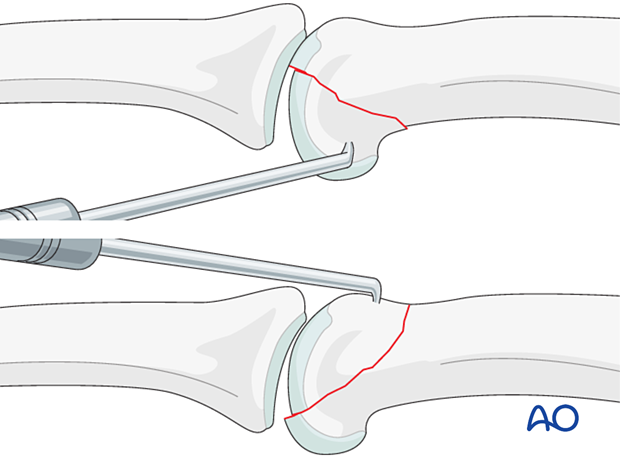
Fracture reduction
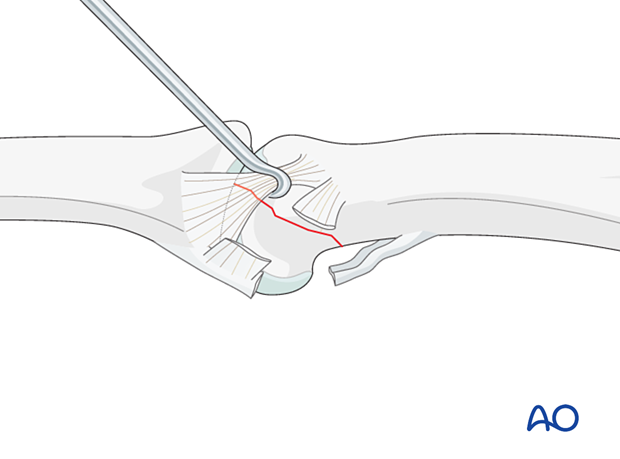
Gently reduce the fragment with a dental pick. Be careful to avoid fragmentation.
The opposite joint surface of the middle phalanx can be used as a template for reduction.
If a small articular fragment is present, it can be excised. This will not compromise the stability or flexion of the PIP joint.
If there is soft-tissue interposition, this must be removed.
Any incongruency on the palmar side is critical and can impede movement. It must be anatomically reduced and fixed.
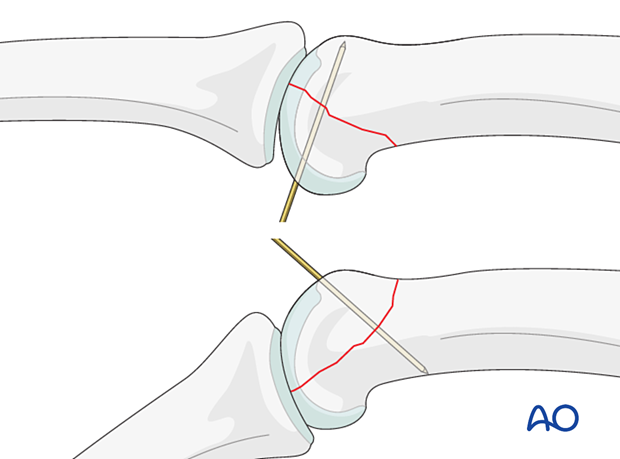
Preliminary K-wire fixation
Preliminarily stabilize the fragment with a K-wire or the guide wire for a cannulated screw.
5. Fixation
Sparing the ligaments
In dorsal fragmentsIn dorsal fragments, the collateral ligament covers part of the fracture line on the lateral aspect of the head.
Flexing the PIP joint will draw back the collateral ligament, which can be further retracted with a hook to expose the dorsal fragment.
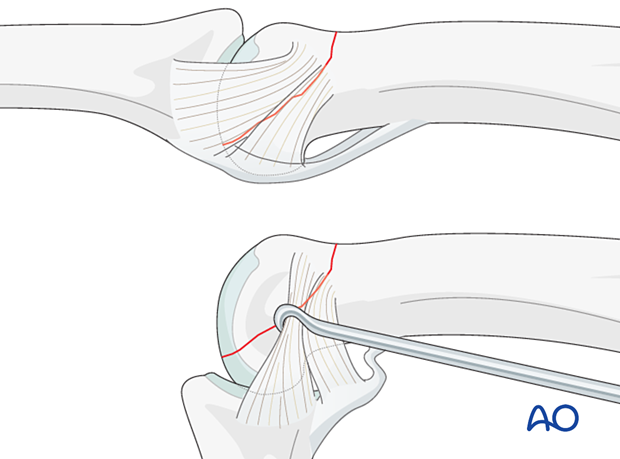
In palmar dislocations, the collateral ligament complex is torn or partially torn. In most cases, the remnant of the collateral ligament can be retracted gently to reveal the palmar condylar fracture line.
Insertion of a headless compression screw
Insert the lag screw through the articular surface into the subchondral bone of the fragment. Select the screw length so the tip does not penetrate the articular cartilage.
Carefully tighten the screw to achieve interfragmentary compression.
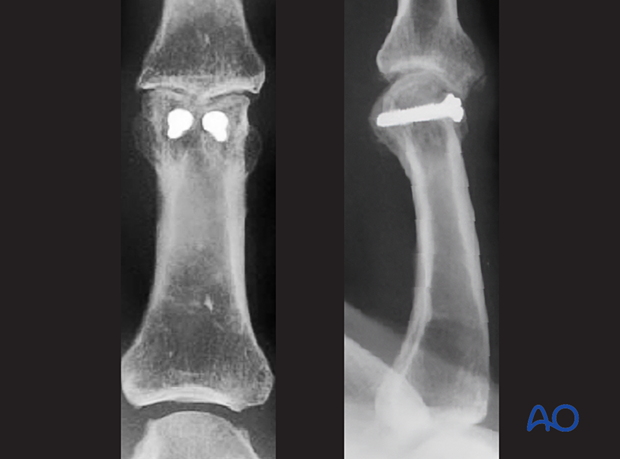
Confirm anatomical reduction and correct screw placement with an image intensifier.
Alternative: cortical lag screw
If headless compression screws are not available, a cortical lag screw may be inserted through the opposite cortex into the subchondral bone.
6. Final assessment
Confirm anatomical reduction of the articular surface and correct screw placement with an image intensifier.
7. Aftercare
Postoperative phases
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.
Postoperative treatment
If there is swelling, the hand is supported with a dorsal splint for a week. This would allow for finger movement and help with pain and edema control. The arm should be actively elevated to help reduce the swelling.
The hand should be splinted in an intrinsic plus (Edinburgh) position:
- Neutral wrist position or up to 15° extension
- MCP joint in 90° flexion
- PIP joint in extension
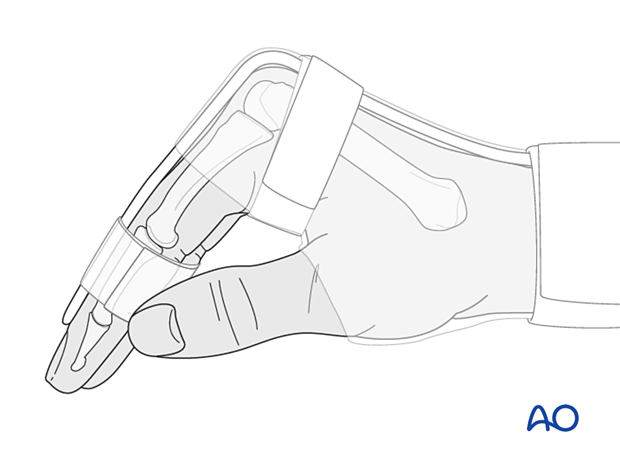
The reason for splinting the MCP joint in flexion is to maintain its collateral ligament at maximal length, avoiding scar contraction.
PIP joint extension in this position also maintains the length of the volar plate.
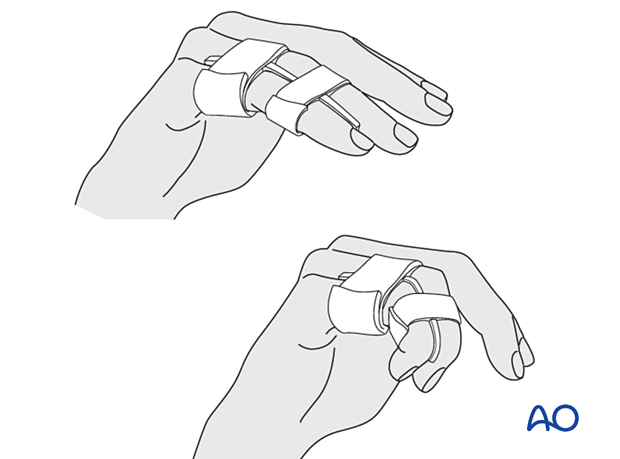
After subsided swelling, protect the digit with buddy strapping to a neighboring finger to neutralize lateral forces on the finger.
Functional exercises
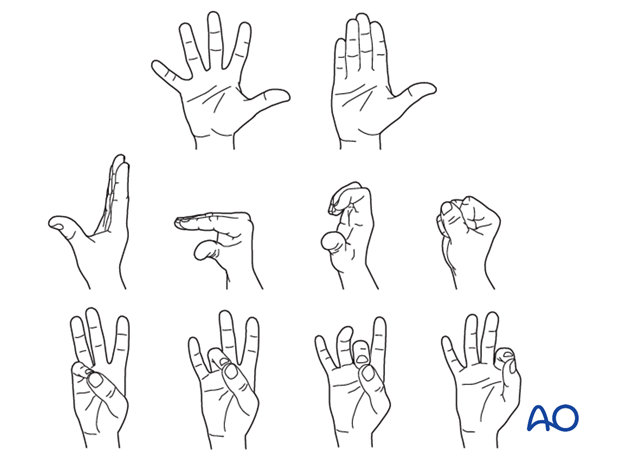
To prevent joint stiffness, the patient should be instructed to begin active motion (flexion and extension) immediately after surgery.
Follow-up
See the patient after 5 and 10 days of surgery.
Implant removal
The implants may need to be removed in cases of soft-tissue irritation.
In case of joint stiffness or tendon adhesion restricting finger movement, arthrolysis or tenolysis may become necessary. In these circumstances, the implants can be removed at the same time.













