Palmar approach to the proximal interphalangeal joint
1. Introduction
The palmar approach offers access to the flexor tendon sheath, the volar plate and the volar capsule, and the condyles and base of the adjacent phalanges.
This approach is indicated mainly for:
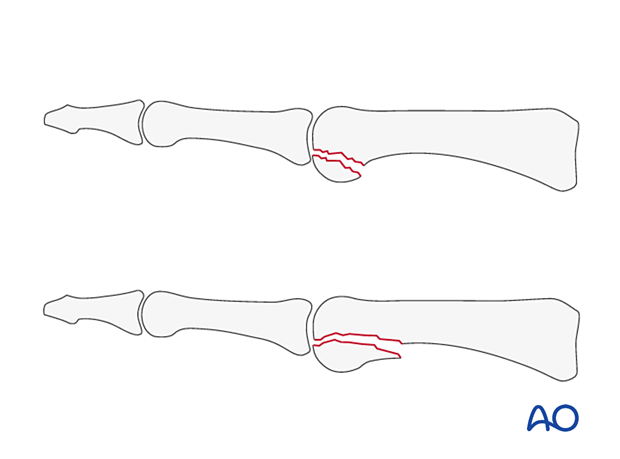
- Volar plate avulsion fractures of the base of the middle phalanx
- Fracture-dislocations of the proximal interphalangeal (PIP) joint
- Comminuted, impacted fractures of the base of the middle phalanx
- Volar coronal fractures of the distal end segment of the proximal phalanx
An exception to this rule is a dorsal central slip avulsion fracture of the base of the middle phalanx, with palmar dislocation, which cannot be approached via a palmar exposure, and the dorsal route becomes the first choice.
The palmar approach is also indicated for volar plate arthroplasty.
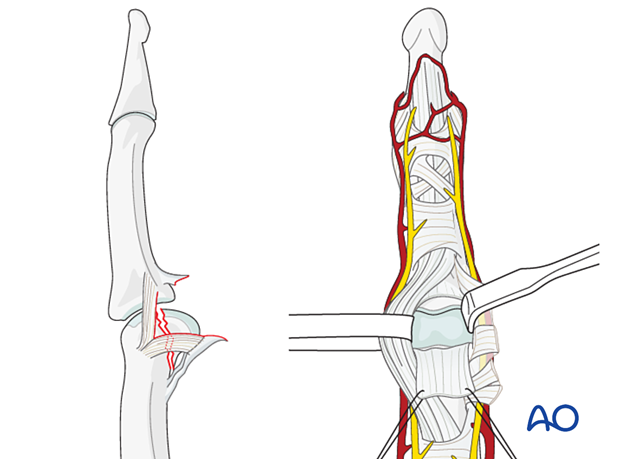
2. Surgical anatomy
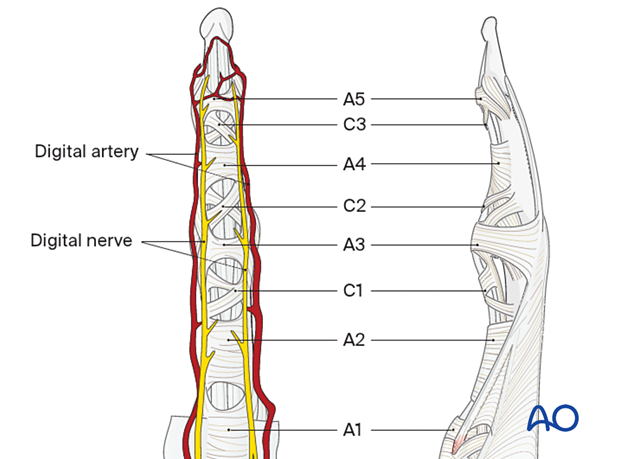
When approaching the PIP joint, preserve the digital arteries and nerve.
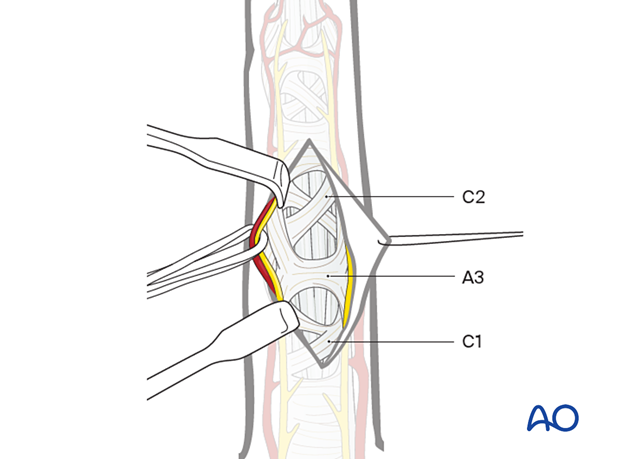
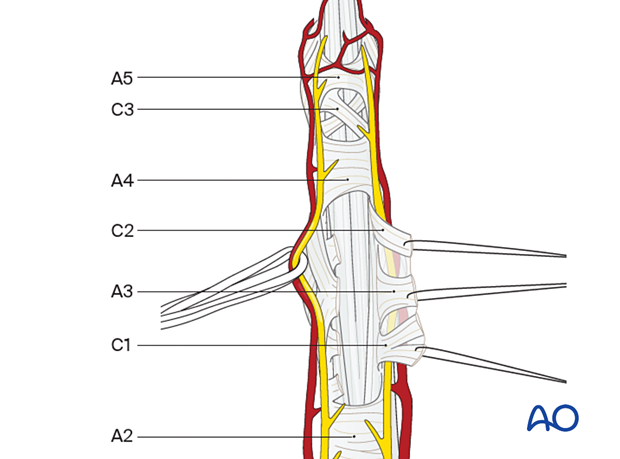
The flexor tendon pulleys are transverse (A) or cruciform (C). They are numbered sequentially from proximal to distal, as illustrated.
On the right, the pulley system is shown diagrammatically for clarity.
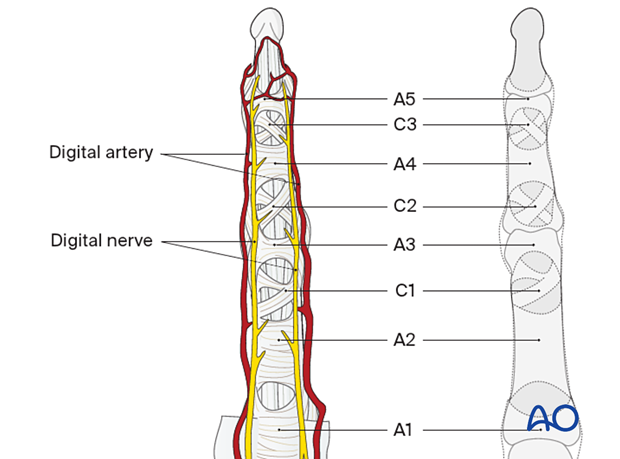
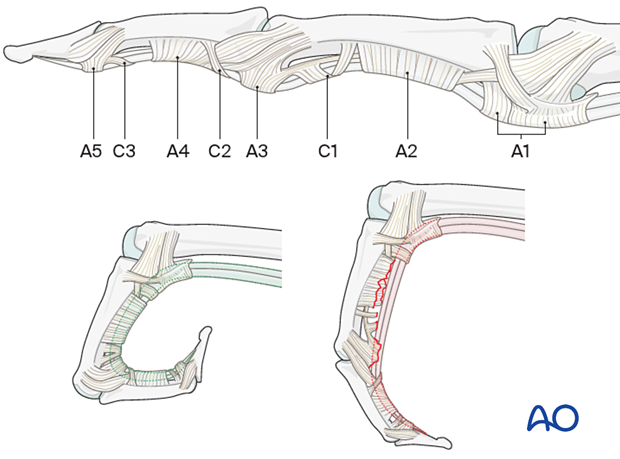
Lateral view showing the pulley system
The A2 and A4 pulleys are critical for the effective function of the flexor tendon system. They must be preserved to avoid bowstringing of the flexor tendons during flexion of the finger.
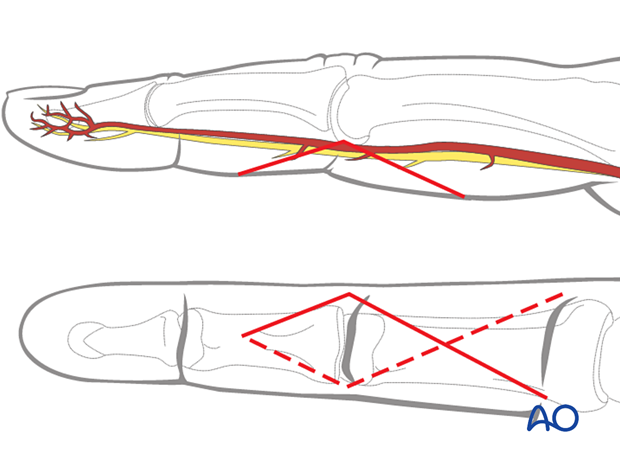
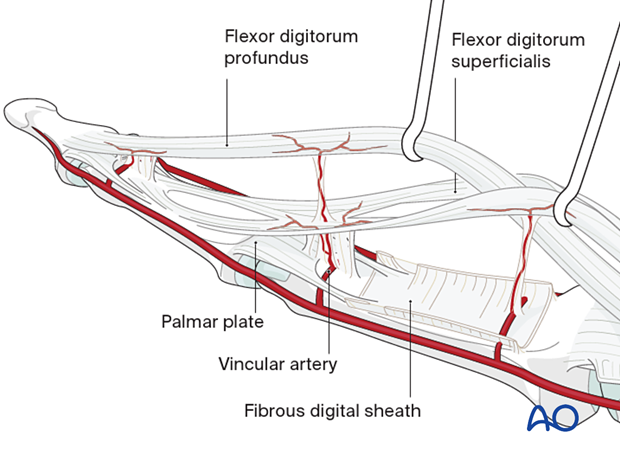
Vincular arteries
The vincular arteries are delicate but essential to the vascularity of the flexor tendons. They must be preserved whenever possible; otherwise, the vascularity of the tendon may be compromised.
3. Skin incision
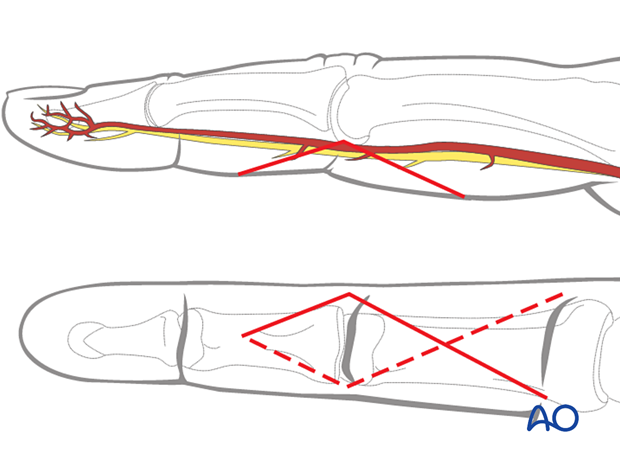
Perform a carefully planned palmar, angled skin incision (Bruner zigzag), using the flexor skin creases as a guide, as illustrated.
The apex of the angle should be at the end of the intermediate flexor crease, level with the PIP joint.
Plan the apex of the incision so that the scar does not involve the radial border of the index or the ulnar border of the little finger.
4. Elevation of the flap
Elevate the angled skin flap by blunt dissection in the thin subcutaneous tissue and retract the apex using a fine suture. Identify and gently mobilize the digital arteries and nerves.
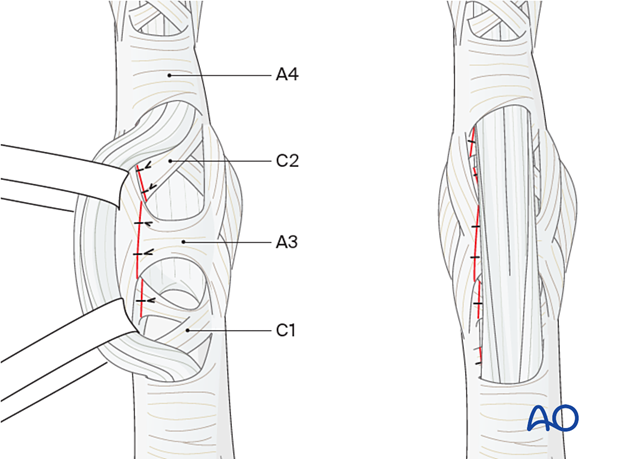
The flexor sheath with the C1, C2, and A3 pulleys is exposed.
Division of the pulleys
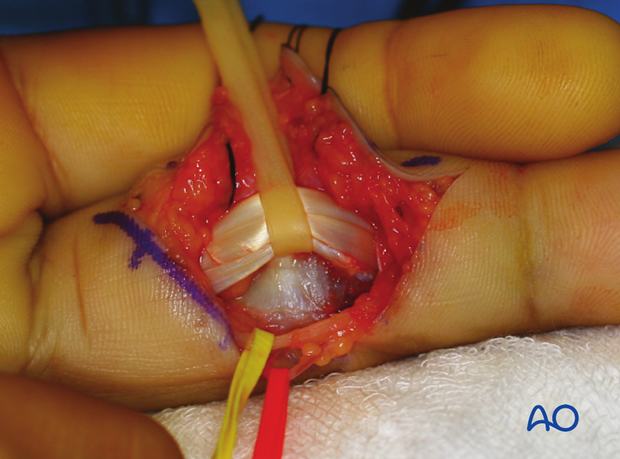
Incise the C1, A3, and C2 pulleys laterally, near their bony attachments, leaving enough (at least 2 mm) for later reattachment, and elevate them with sutures.
This clinical photo gives a good view of the flexor tendons after the pulleys have been divided.

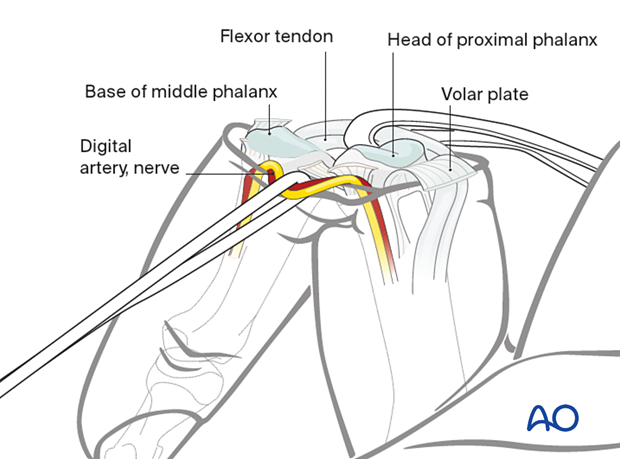
5. Exposure of the palmar capsule
Often, reduction and fixation of volar coronal fractures do not need further exposure.
For full exposure of the joint, the volar plate may be detached with a flap.
Retract the flexor tendons using a latex loop (such as a Penrose drain).
The palmar capsule is now visible.
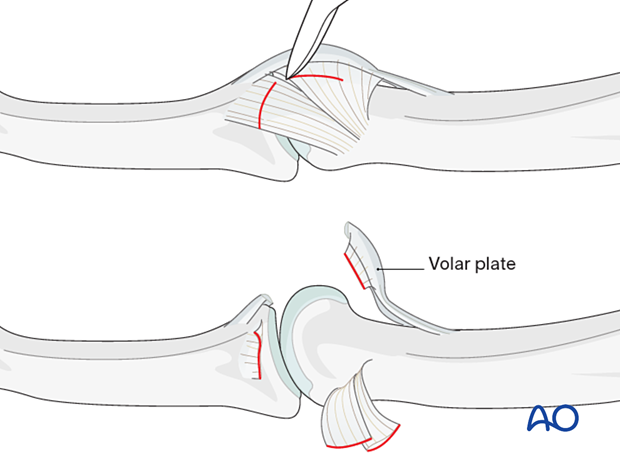
6. Exposure of the volar plate
Extension of the PIP joint now exposes the distal edge of the volar plate. The fracture fragment can be elevated with the volar plate and retracted proximally.
7. ‘Shotgun’ hyperextension exposure
Indications
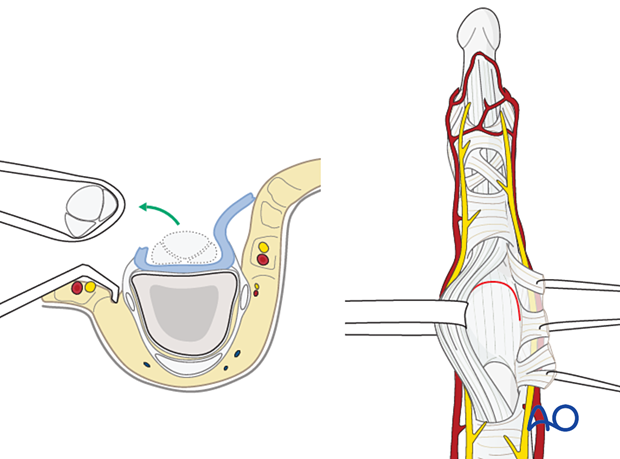
If there is comminution, or impaction of fragments, at the head of the proximal phalanx that needs to be reduced, both collateral ligaments must be divided.
This will enable full opening of the PIP joint by hyperextension, thereby exposing fully the base of the middle phalanx.

Detachment of the ligaments
The distal and palmar attachments of the collateral ligaments should be detached bilaterally and retracted dorsally.
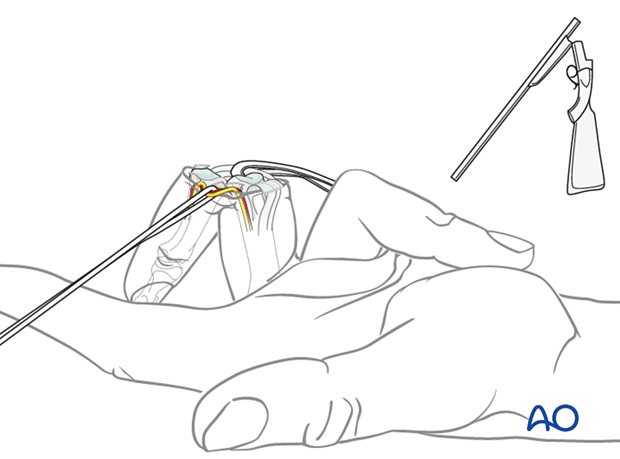
Hyperextension of the finger
After detachment of the collateral ligaments, the finger can be fully hyperextended (as in breaking open a shotgun).
This will give a complete view of the whole joint surface of the middle phalanx and both condyles of the proximal phalanx.

8. Wound closure
Regardless of the chosen approach, all tendon incisions must be repaired with nonabsorbable monofilament sutures with an atraumatic needle before wound closure.
Volar plate reattachment
Reattach the volar plate using either a pullout suture or at least two anchor sutures.
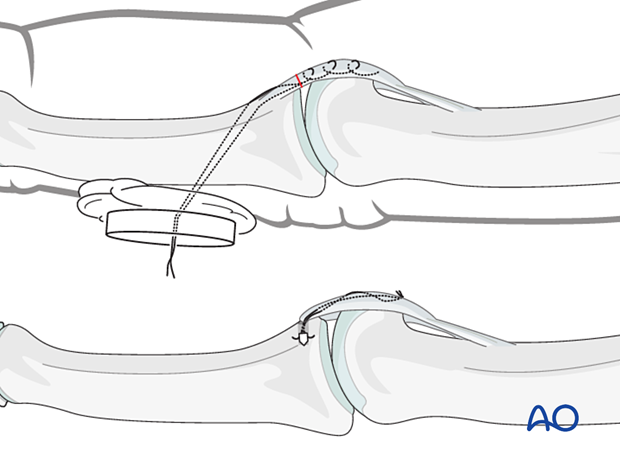
Pulley repair
It is recommended to repair the A3 pulley. If possible, also reattach the C1 and C2 pulleys.
The flap of the C1, A3, and C2 pulleys is passed beneath the flexor tendons and sutured to the opposite side, using 5.0 nonabsorbable monofilament sutures, to reinforce the volar plate.