Dorsal approaches to the proximal interphalangeal joint
1. Introduction
The dorsal approach to the proximal interphalangeal (PIP) joint offers access to the extensor tendon, joint capsule, collateral ligaments, the distal part of the proximal phalanx, and the base of the middle phalanx.
This approach may be extended proximally and distally as needed.
This approach is indicated for:
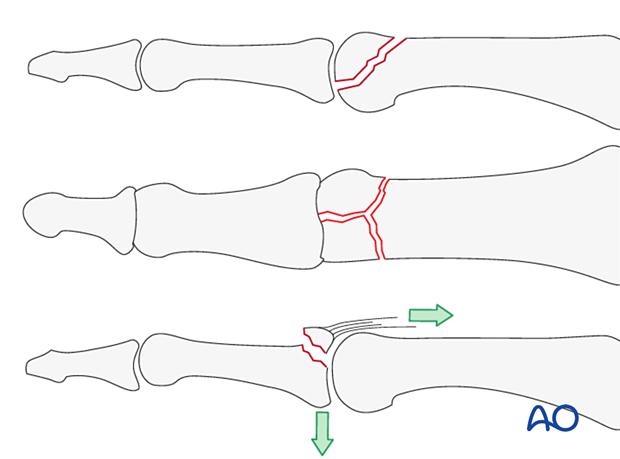
- Intraarticular fractures
- Dorsal coronal plane fractures of the condyles of the proximal phalanx
- Central slip avulsion fractures from the dorsal base of the middle phalanx
AO teaching video
Finger, proximal interphalangeal joint, dorsolateral approach
AO teaching video
Finger, proximal interphalangeal joint, midline approach
2. Surgical anatomy
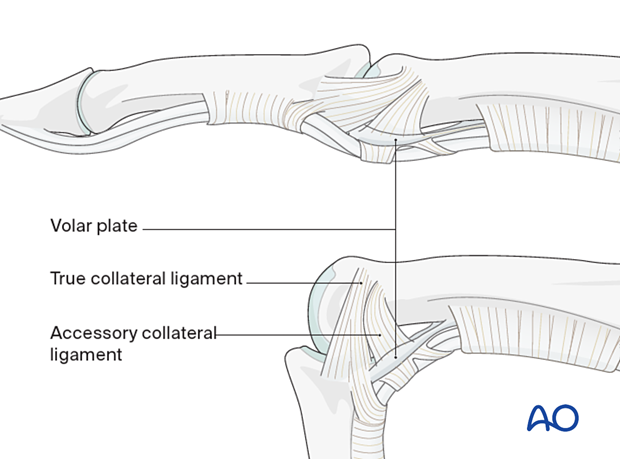
The interphalangeal joints are hinge joints. The heads of the proximal and middle phalanges each have two articular condyles that resemble a grooved trochlea and assist in preventing adduction/abduction and rotation in conjunction with the collateral ligaments.
Dynamic stability results from compressive forces, which increase during pinch and grip. Passive stability derives from the bone morphology and tension in the collateral ligaments and the volar plate. This passive stability is maximal in full extension.
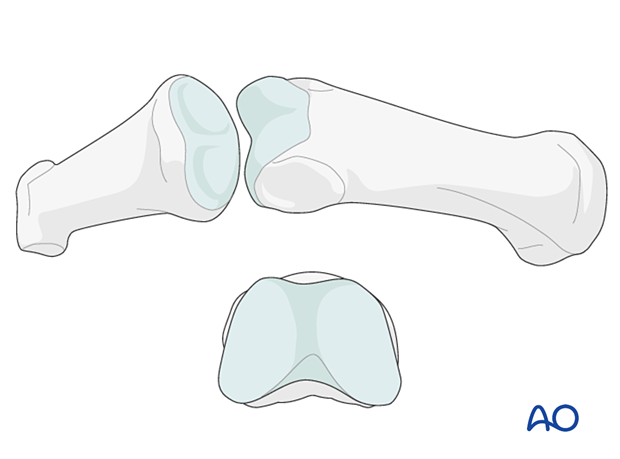
The two collateral ligaments and the volar plate are the primary structures stabilizing the interphalangeal joints and preventing displacement in the coronal plane (abduction/adduction).
The collateral ligaments also prevent side-to-side translational displacement.
The accessory collateral ligaments slacken in flexion, while the true collateral ligament is further tensioned in flexion due to the greater palmar width of the condyles.
When using a lateral approach, avoiding injury to these structures is mandatory.
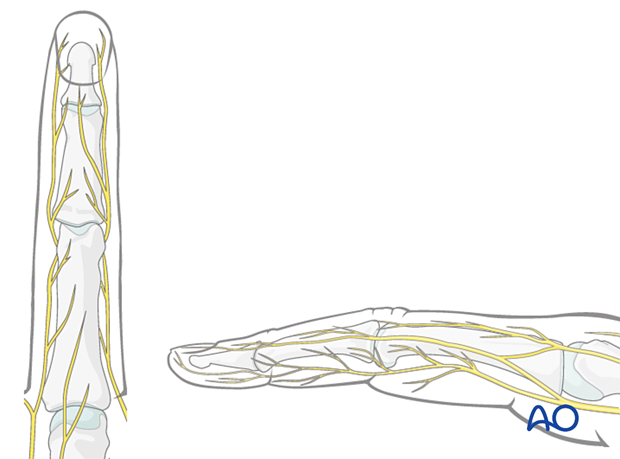
Nerve identification
In the thin subcutaneous tissue, identify and protect the dorsal sensory branches of the radial and ulnar nerves.
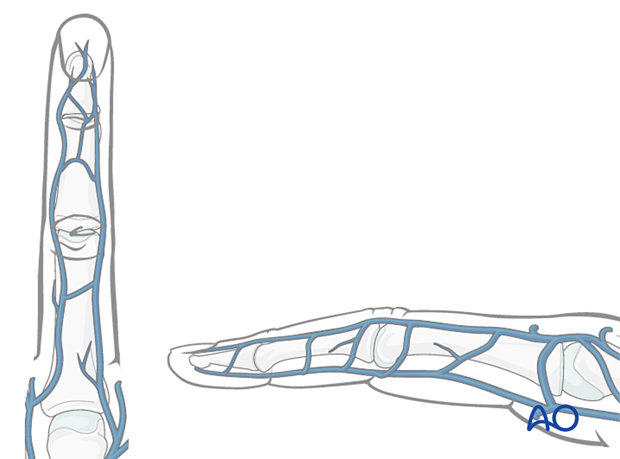
Vein identification
The dorsal venous system of the fingers has longitudinal and transverse branches. Be careful to preserve the longitudinal branches. For better exposure, the transverse branches may be ligated or cauterized, but preserve as many dorsal veins as possible to avoid congestion and swelling, with consequent fibrosis and stiffness.
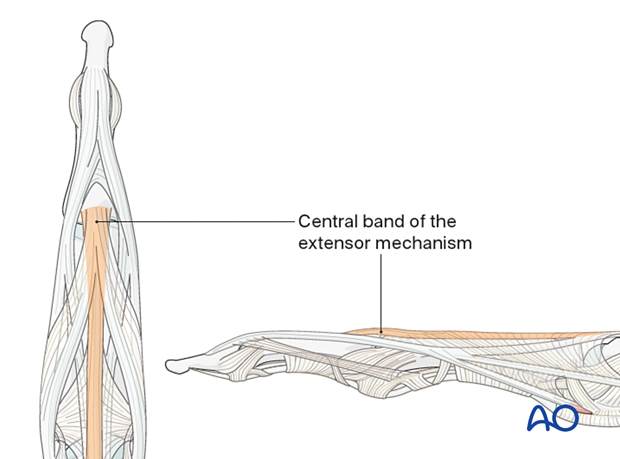
Preservation of soft-tissue structures
Preserve the insertion of the central band of the extensor mechanism to the dorsal aspect of the middle phalangeal base. If this is detached and not repaired, a boutonniere deformity may occur.
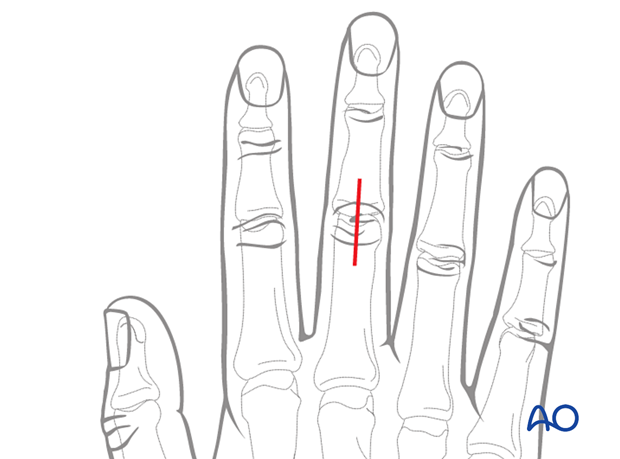
3. Skin incision
Several skin incision options are available. Each comes with benefits and disadvantages.
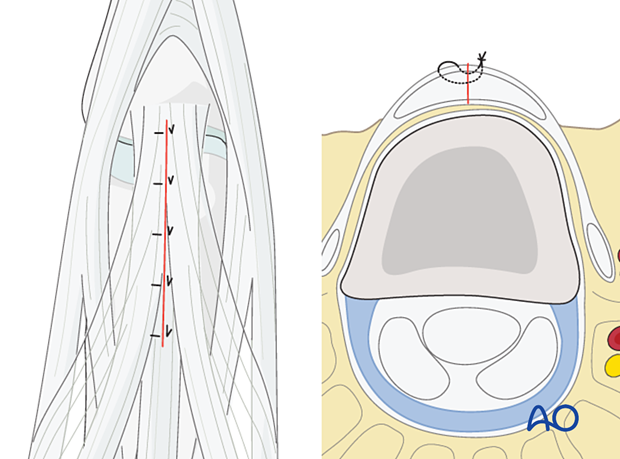
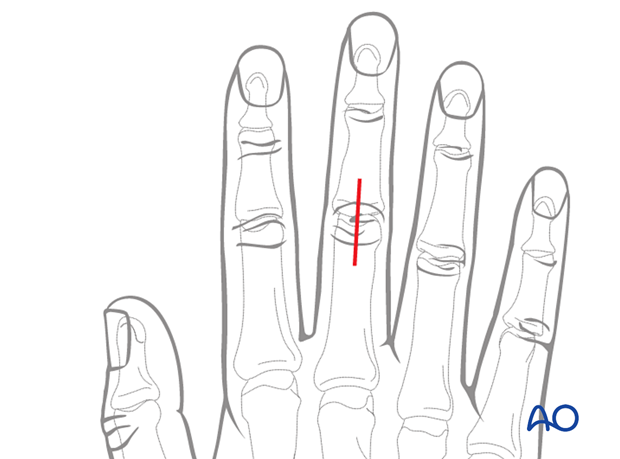
Straight dorsal incision
Perform a straight midline dorsal incision over the PIP joint.
With this incision, vascularity and venous drainage are well preserved. Early postoperative motion will prevent scarring between the skin, tendon, and bone.
The disadvantage of this incision is that any skin and tendon scarring will be in the same line.
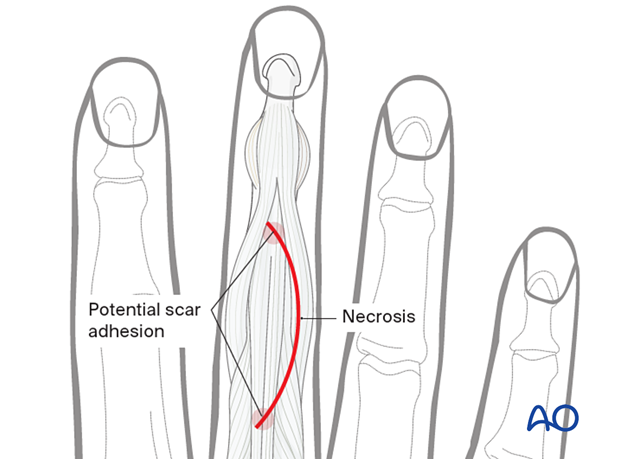
Curved skin incision
Perform a curved skin incision over the PIP joint. The convexity of the incision is planned so that the scar does not involve the radial border of the index or the ulnar border of the little finger. The fracture morphology and implant placement must be given priority when planning the incision.
The advantage of the curved incision is that the skin and tendon scarring are not in line.
The disadvantage is reduced vascularity at the apex of the curve, with a risk of necrosis and delayed skin healing.
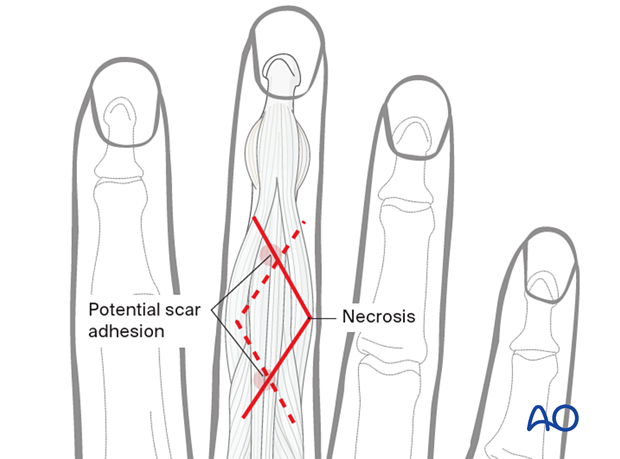
Zigzag skin incision
A zigzag incision may be used. This approach allows for:
- Full exposure of the joint and the shaft
- Paratendon or through tendon approach
Depending on the fracture pattern, the incision may be designed with an ulnar or radial apex.
The skin on the ulnar side of the 5th finger and the radial side of the 2nd finger should be preserved to protect sensitivity.
4. Skin retraction
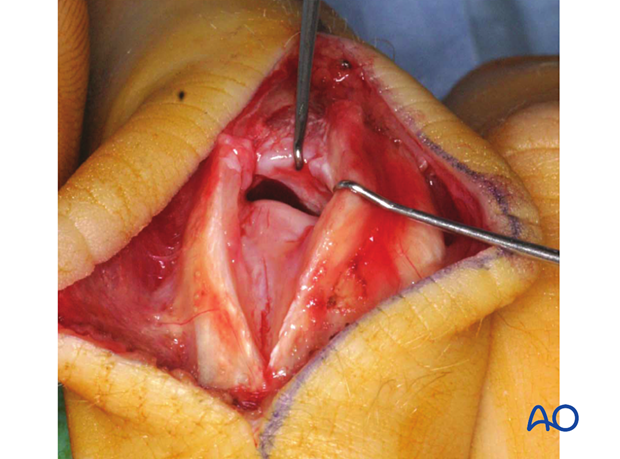
Retract and elevate the skin and the subcutaneous tissue as a single layer. The extensor apparatus is fully exposed and intact.
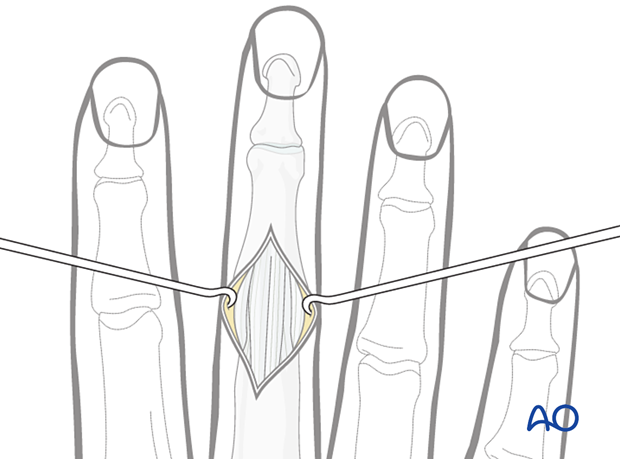
5. Tendinous approach
To approach the PIP joint for fractures of the proximal phalanx, a dorsal incision may be used in the middle of the extensor mechanism.
Retraction of the slips exposes the dorsal capsule of the PIP joint.
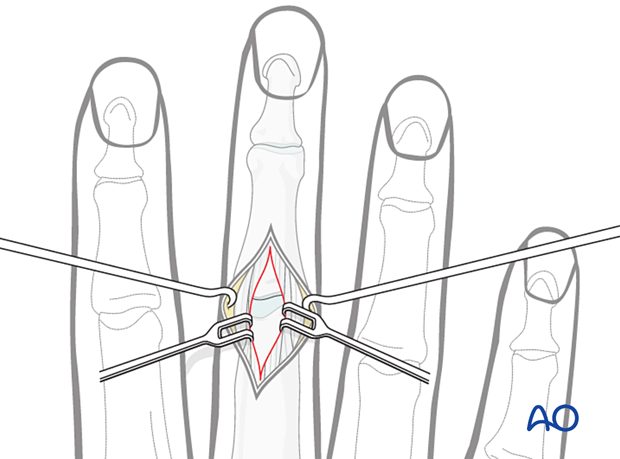
Alternatively, a paratendon approach through the lateral band may be used, especially to reduce and fix unicondylar fractures.
The tendon may be retracted to either side.
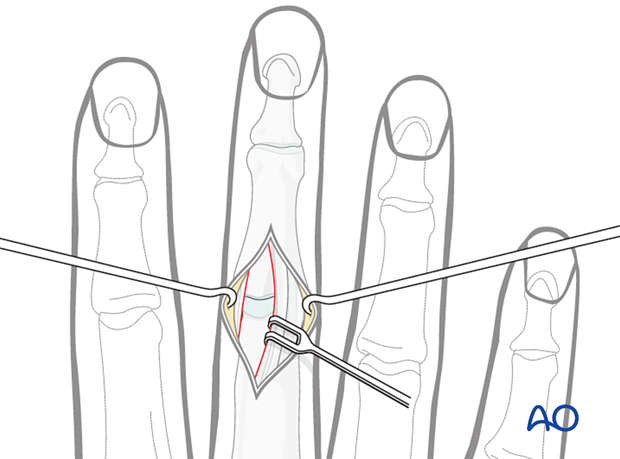
Incise gently lateral to the lateral band.
Divide the transverse retinacular ligament using a dental pick inserted between it and the collateral ligament to avoid accidentally cutting the collateral ligament.
A longitudinal capsulotomy allows the joint to be inspected.
Capsulotomy
Perform a vertical capsulotomy to expose the joint.
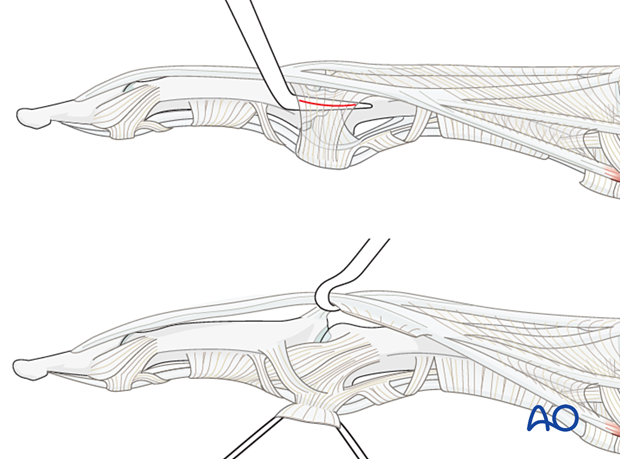
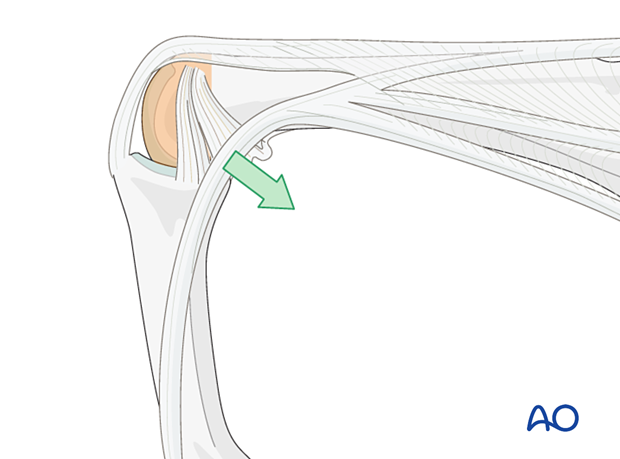
Flexion for better exposure
Flexing the PIP joint allows the lateral band to move in a palmar direction, giving better exposure to the joint.
6. Wound closure
Regardless of the chosen approach, all tendon incisions must be repaired with nonabsorbable monofilament sutures with an atraumatic needle prior to wound closure.
Cover the implant with the periosteum as far as possible; this helps minimize contact between the extensor tendons and the implant.
To avoid subluxation of the tendon after a paratendon approach, reattach the tendon.