MTP joint fusion
1. General considerations
If fragmentation is such that the joint cannot be reconstructed, the options are:
- nonoperative treatment
- arthroplasty
- primary fusion
Neither of these options is ideal.
The results may be unsatisfactory because of the fracture's intraarticular nature, and the patient may complain of pain and stiffness.
In the hallux, excisional arthroplasty is less tolerated due to instability.
Arthroplasty exists but will not be covered here.
As fusion is permanent, the decision to perform fusion should be considered for only significantly damaged articular surfaces.
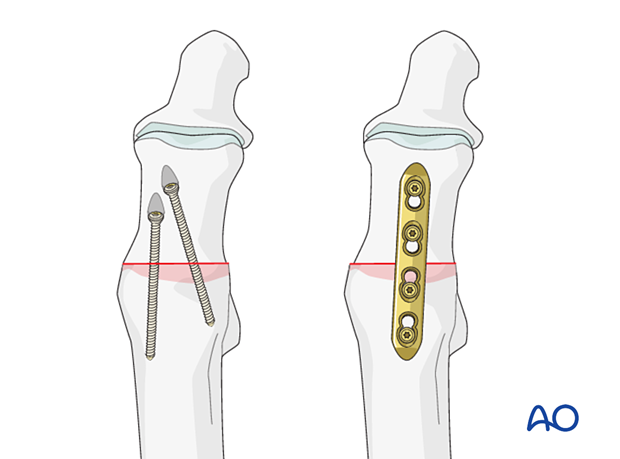
The fusion can be completed using either lag screws or a plate.
The patient should be made aware that this procedure will shorten the toe.
Toe fractures versus long bone fractures
Toe fractures are different from long bone fractures.
- The bones are very small
- Fracture gaps are small
- Fixation devices don't need to counter large forces
Thus, following the AO principles is less critical than for long bones, and often isolated screws or K-wires alone will work satisfactorily.
Restoration of length, rotation, and angulation are important for cosmesis.
The hallux is particularly critical due to its importance for walking.
Timing of surgery
The timing of surgery is influenced by the soft tissue injury and the patient's physiologic status.
Dislocation or injuries associated with the skin at risk requires immediate intervention regardless of the amount of soft tissue swelling.
If possible, swelling should be significantly decreased before surgery, which can take up to two weeks in some instances.
Open fractures should be promptly irrigated and debrided, and treated with antibiotics. Definitive fracture fixation may not be possible during this setting.
Forefoot fractures do not contribute to physiologic instability. If there is no soft tissue at risk, urgent intervention is not required.
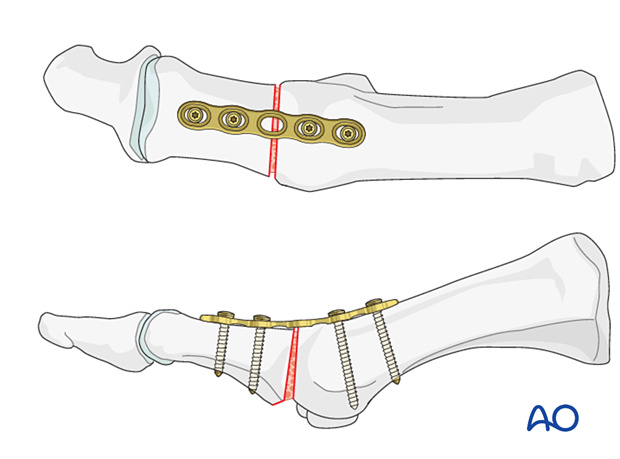
Lag screws vs plate fixation
The fixation can be ensured using either lag screws or a plate.
Typically, lag screws are used when the construct is length-stable, and compression is possible.
Plates are an acceptable alternative to lag screws but result in more prominent hardware. Plates in combination with autogenous bone graft may also be used in cases with bone loss where maintenance of length is desirable. A dorsal plate is less prominent than a medially placed plate.
2. Patient preparation and approaches
Patient preparation
This procedure is typically performed with the patient placed supine and the knee flexed 90°.

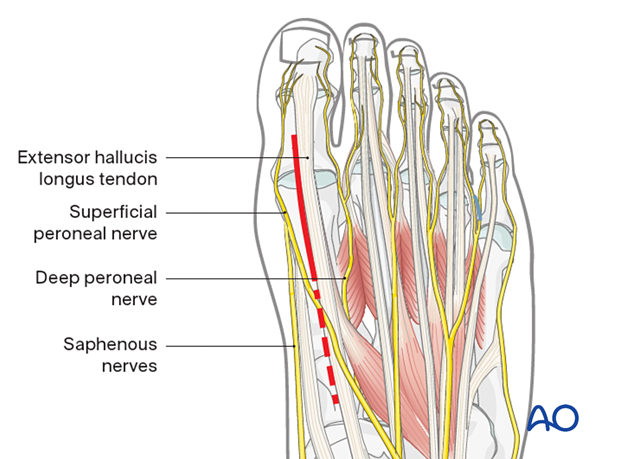
Selection of approach
Fusion may be performed through either the:
If the fusion is secured using a plate, a dorsal plate will be less prominent than a medial plate.
3. Preparation of joint for fusion
Visualization
Expose the articular surfaces.
Visualization may be improved by longitudinal manual distraction or a mini distractor; and by releasing the dorsal insertion of the EHB.
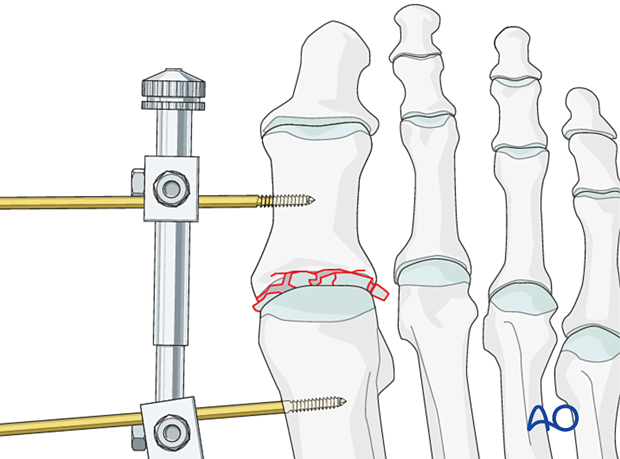
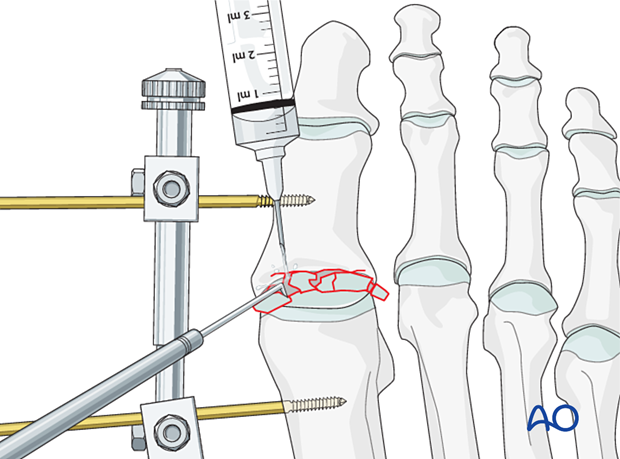
Irrigation
Irrigate the fracture site using a syringe.
Once adequate visualization has been achieved and the joint thoroughly irrigated, examine the extent of articular surface involvement to validate the preoperative plan of primary fusion versus ORIF.
If joint comminution is not extensive, it may be possible to perform ORIF.
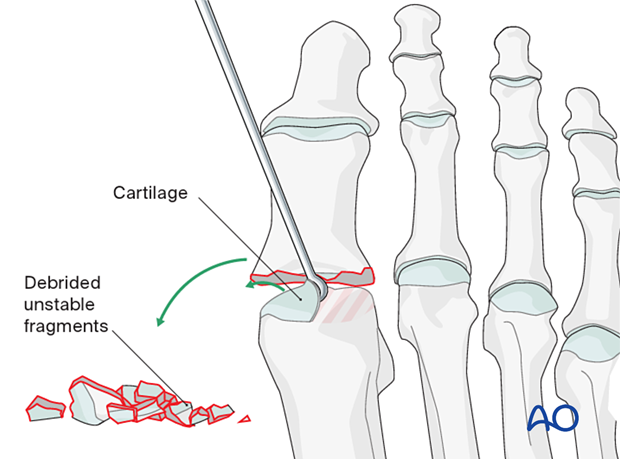
Preparation of the joint for fusion
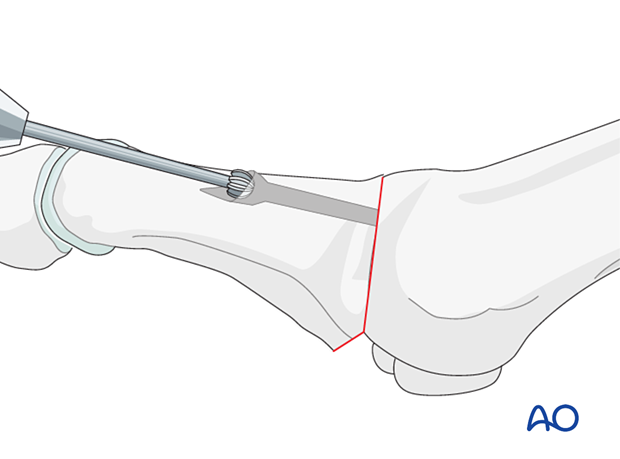
Displaced fracture fragments are debrided and mobilized with a dental pick or Freer elevator.
Remove the cartilage from the adjacent bone using a curette.
Disrupt the subchondral bone using a high-speed burr to promote bone growth.
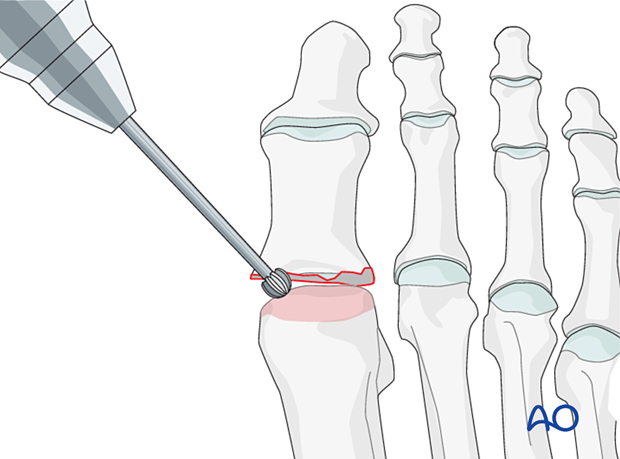
The bone may need further debridement to ensure a large contact surface.
The amount of debridement performed should be minimized to preserve length but still ensure an appropriate contact surface for fusion.
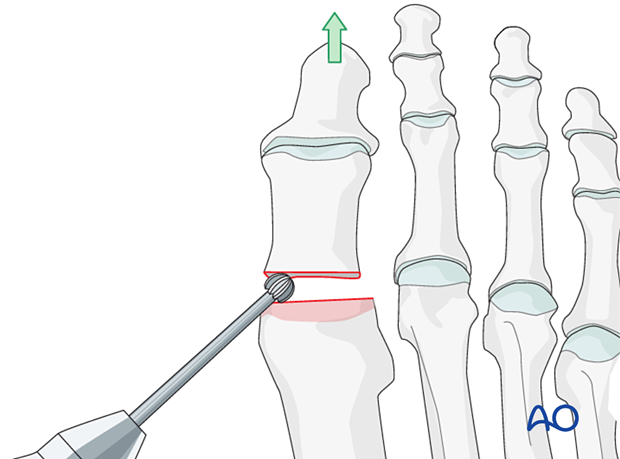
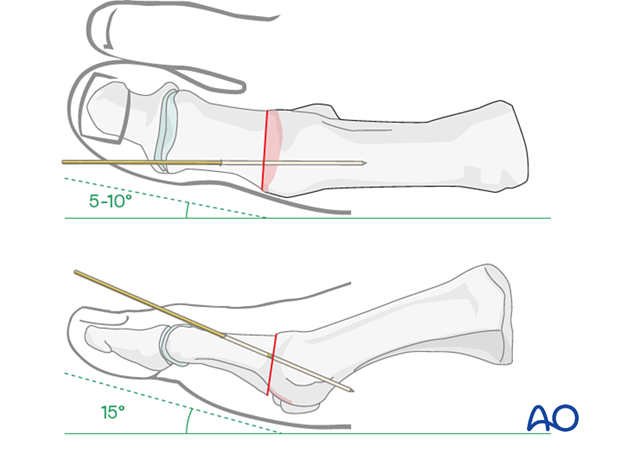
The positioning of the hallux
Position the hallux in 15° of dorsiflexion relative to the floor's plane and 5–10° of valgus relative to the first metatarsal.
Temporarily fix the position using a K-wire inserted from dorsal to plantar.
Before permanent fixation, ensure that the two bone ends are intimate and use intraoperative radiographs to confirm correct alignment.
4. Fixation
Lag screw fixation
Ideally, two lag screws (2.7 mm) are inserted. Ensure that the lag screws are well spread at the arthrodesis site, which will result in a more rigid construct.
Countersink the glide hole to reduce screw prominence.
The screws should fully engage the bone proximally but should not be prominent at the metatarsal head's plantar surface, which may cause pain.
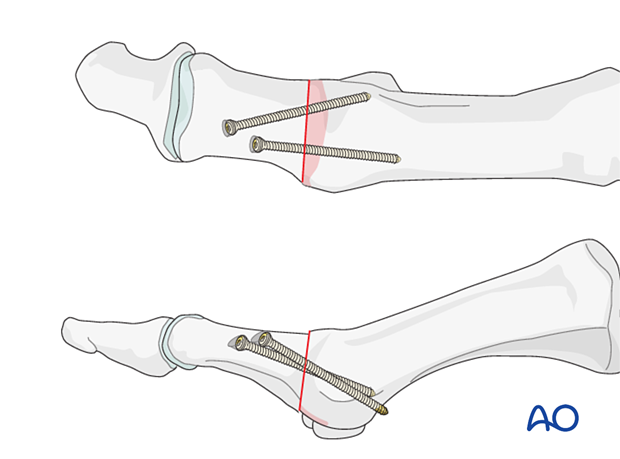
The screws may also be inserted in a crossing pattern.
The screws should not cross at the MTP interface.
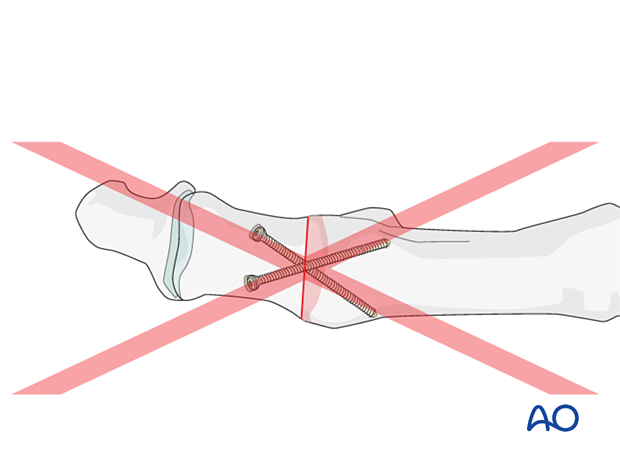
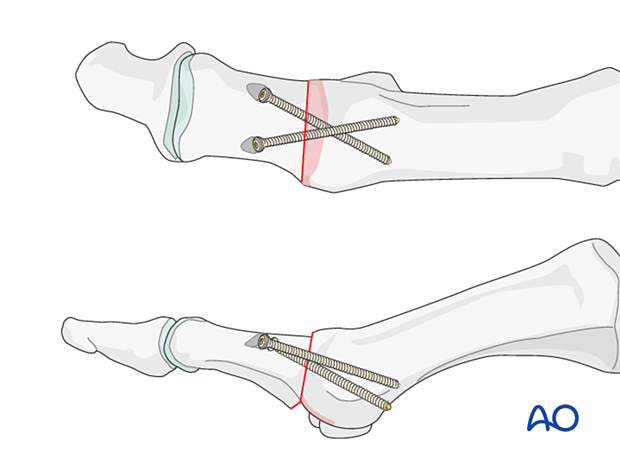
Plate fixation
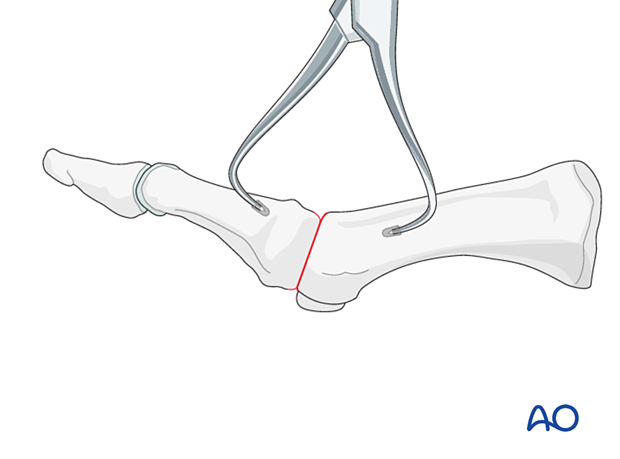
With compressionCompress the intended fusion site using a reduction clamp.
Two small 2.0 drill holes may be helpful to enable clamp application.
A four-hole 2.4 or 2.7 compression plate is contoured to fit the bone surface.
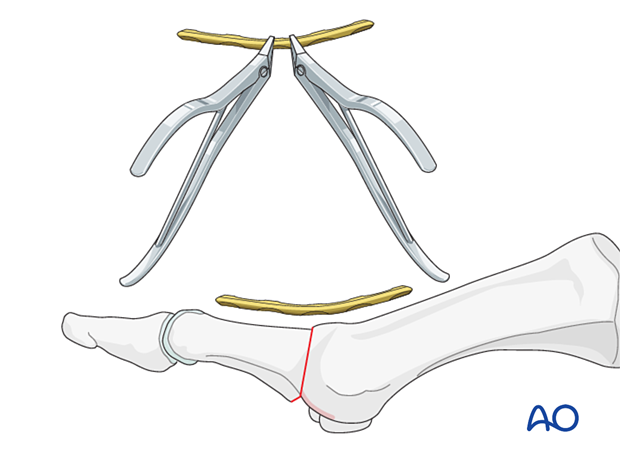
The plate is fixed using a minimum of two screws in each bone segment.
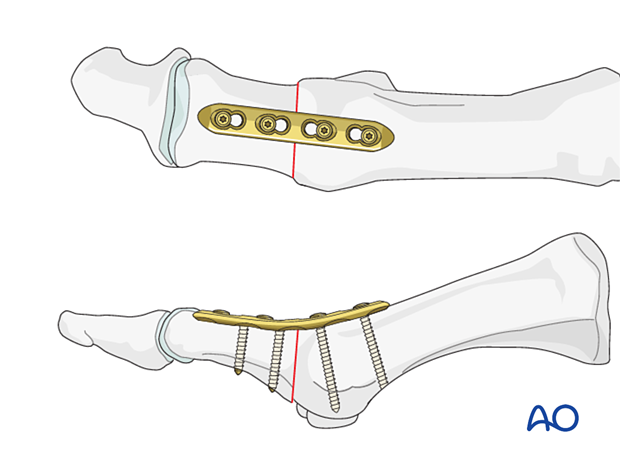
The plate is fixed using a minimum of two screws in each bone segment.
Any bony defect may be grafted.
5. Aftercare
The surgical site must be protected until the soft tissues have healed. Soft tissue healing may be slow.
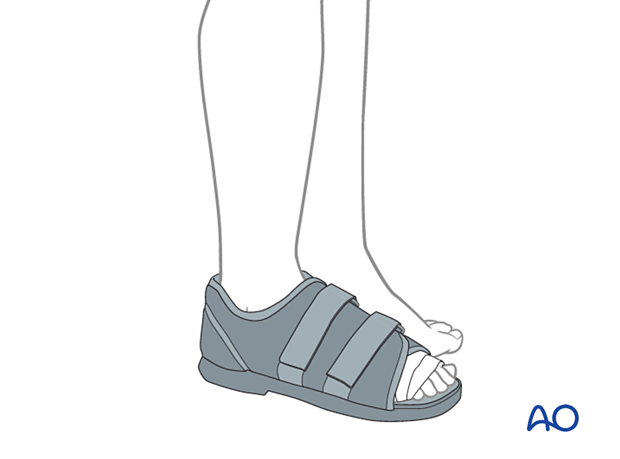
We recommend a flat, rigid sole shoe for postoperative care and subsequent ambulation after wire removal.
If such is not available, then a short leg cast would be necessary until ambulation is started.
If K-wires are present, they can be removed at six weeks.