ORIF - Anterior lag screws for large fragments
1. Principles
Hoffa fractures involve important load-bearing areas of the knee joint surface, and the principles of anatomical reduction and absolute stability of fixation apply.
Generally, these fractures are reduced and fixed from posterior with leg screws and a buttress plate. However, occasional circumstance would only allow for anterior fixation alone. This fixation is not stable and is generally not advised.
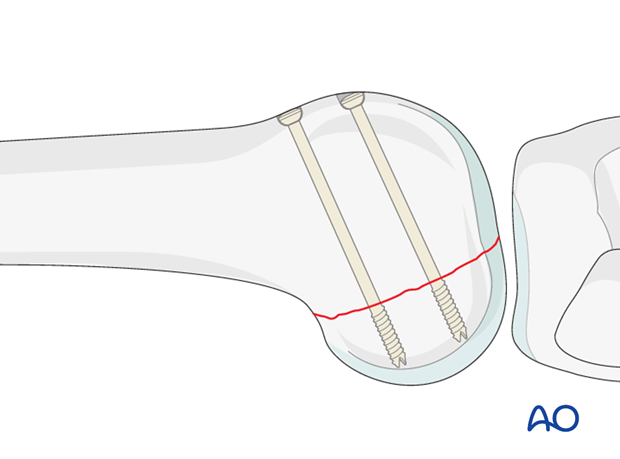
Fixation from anterior can be achieved indirectly with 3.5 mm or 4.5 mm screw systems. It is advantageous to use cannulated screw systems.
In small fragments direct fixation through a posterior approach is required.
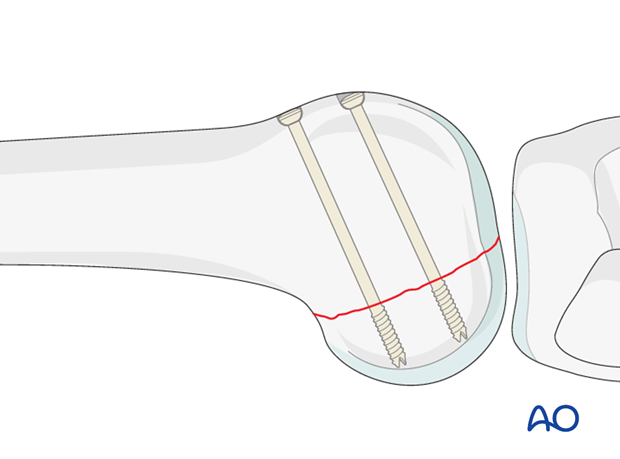
At least two screws should be used, in order to prevent fragment rotation and to achieve satisfactory compression.
No implant can violate the articular surface.
Similar principles apply if both condyles are fractured.
2. Preparation and approach
Positioning
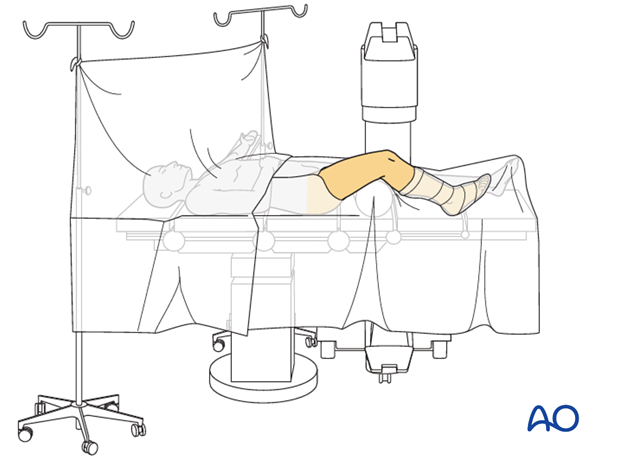
This procedure may be performed with the patient in one of the following positions:
- Supine position knee flexed 30°
- Supine position knee flexed 90°
- Lateral decubitus (particularly in obese patients)
Approach
For this procedure the following approaches may be used:
- MIO approach from lateral/anterolateral
- Medial parapatellar approach
- Lateral parapatellar approach
- Medial approach
These difficult fractures can be approached for reduction and fixation from the anterior aspect. If the posterior condylar fragments are large, the fracture lines will usually be accessible by the parapatellar approach.
For shallower fragments the standard lateral/anterolateral approach is necessary to gain more posterior access: alternatively, a posterior approach should be considered.
For the medial side, a straight medial approach can be used, taking care to avoid injury to the infrapatellar branch of the saphenous nerve.
3. Reduction
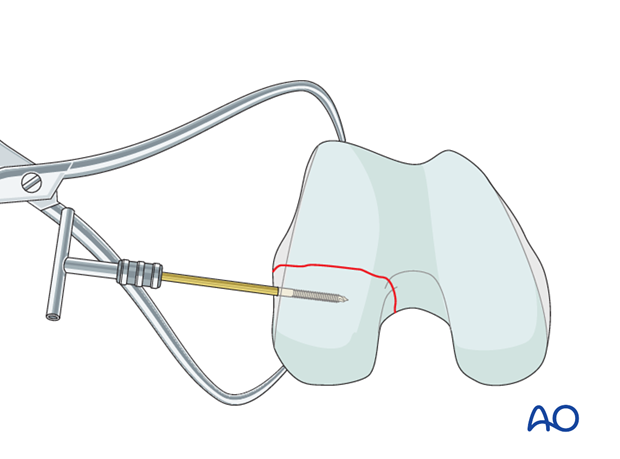
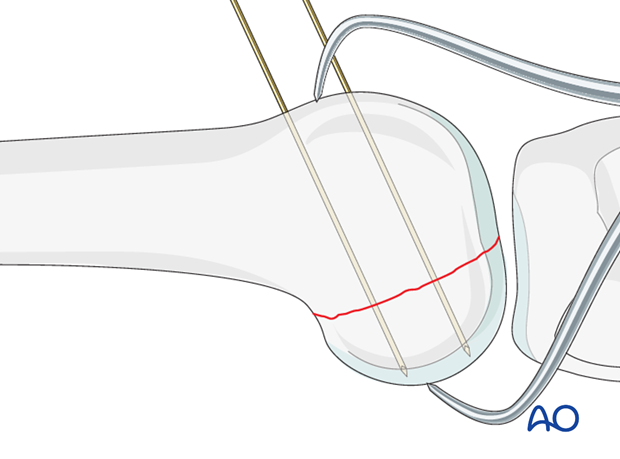
Achieve reduction using periosteal elevators and a large pointed reduction forceps. The joystick technique, in which a small Schanz screw is inserted from the extraarticular surface, is also useful (as illustrated).
4. Fixation
Guide-wire insertion
Insert the guide wires as perpendicularly as possible to the fracture plane.
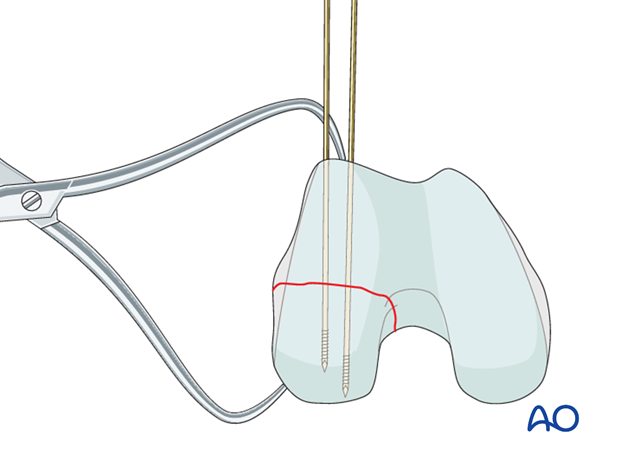
Check guide-wire placement
Check the correct guide-wire insertion under fluoroscopic image intensifier control. The condylar surface must not be perforated.
Screw insertion
The lag screws are inserted according to the standard technique for cancellous lag screws under image intensifier control.
There should be no protruding screw heads.
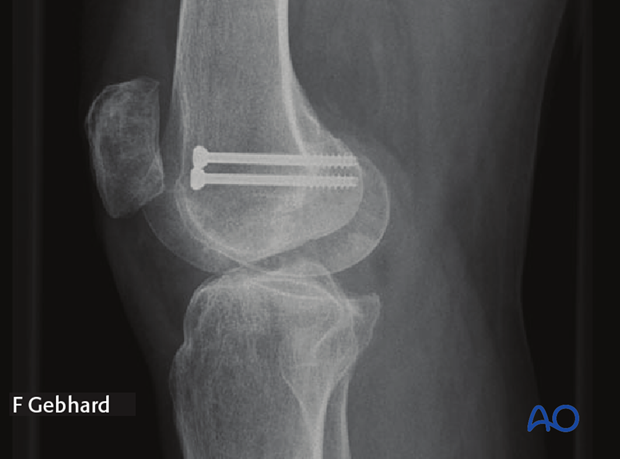
X-ray
X-ray showing the completed osteosynthesis. In this instance this fixation has worked over long term. Generally, a posterior buttress plate should also be used.
5. Aftercare
Impediments to the restoration of full knee function after distal femoral fracture are fibrosis and adhesion of injured soft tissues around the metaphyseal fracture zone, joint capsular scarring, intra-articular adhesions, and muscle weakness.
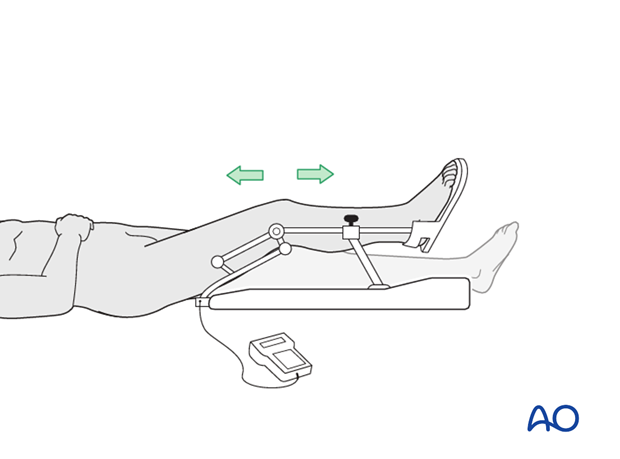
Early range of motion helps restore movement in the early postoperative phase. With stable fracture fixation, the surgeon and the physical therapy staff will design an individual program of progressive rehabilitation for each patient.
The regimens suggested here are for guidance only and not to be regarded as prescriptive.
Functional treatment
Unless there are other injuries or complications, knee mobilization may be started immediately postoperatively. Both active and passive motion of the knee and hip can be initiated immediately postoperatively. Emphasis should be placed on progressive quadriceps strengthening and straight leg raises. Static cycling without load, as well as firm passive range of motion exercises of the knee, allow the patient to regain optimal range of motion.
Weight bearing
Touch-down weight-bearing (10-15 kg) may be performed immediately with crutches, or a walker. This will be continued for 6-10 weeks postoperatively. This is mostly to protect the articular component of the injury, rather than the shaft injury. Touch-down weight-bearing progresses to full weight-bearing gradually, over a period of 2 to 3 weeks (beginning at 6–10 weeks postoperatively). Ideally, patients are fully weight-bearing, without devices (e.g., cane) by 12 weeks.
Follow-up
Wound healing should be assessed at two to three weeks postoperatively. Subsequently 6-week, 12-week, 6-month, and 12-month follow-ups are usually made. Serial x-rays allow the surgeon to assess the healing of the fracture.
Implant removal
Implant removal is not essential but should be discussed with the patient if there are implant-related symptoms after consolidated fracture healing.
Thrombo-embolic prophylaxis
Thrombo-prophylaxis should be given according to local treatment guidelines.













