Medial parapatellar approach to the distal femur
1. Principles
This approach is used for medial femoral condylar fractures. In addition, it may be used in retrograde nailing of intra articular fractures.
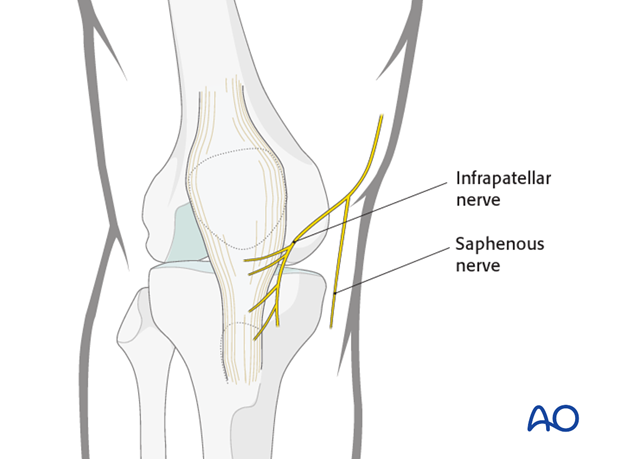
2. Neurovascular structures
The saphenous nerve runs along the medial aspect of the distal femur. The infrapatellar branches of the saphenous nerve lie on the medial and inferior aspects of the patella. Postoperatively, there will be minor sensory disturbance around and below the scar, but significant saphenous nerve damage is avoidable. Occasionally, there may be postsurgical saphenous nerve neuroma formation which is rarely a significant problem.
The long saphenous vein should be preserved.
There are no surgically important arteries on the medial side of the knee joint.
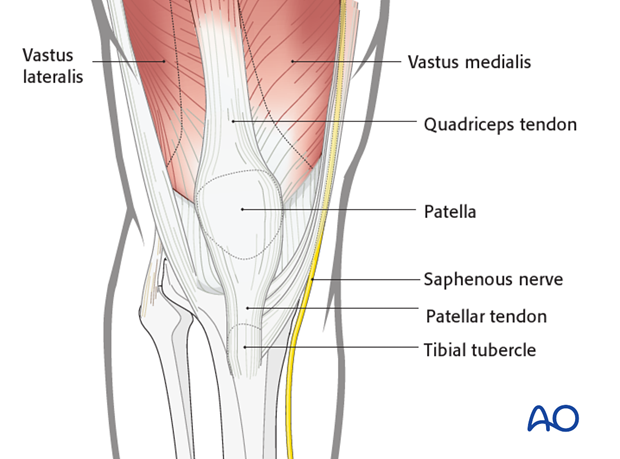
3. Landmarks
The landmarks are the patella, the patellar tendon and the tibial tubercle, which are easily palpable.
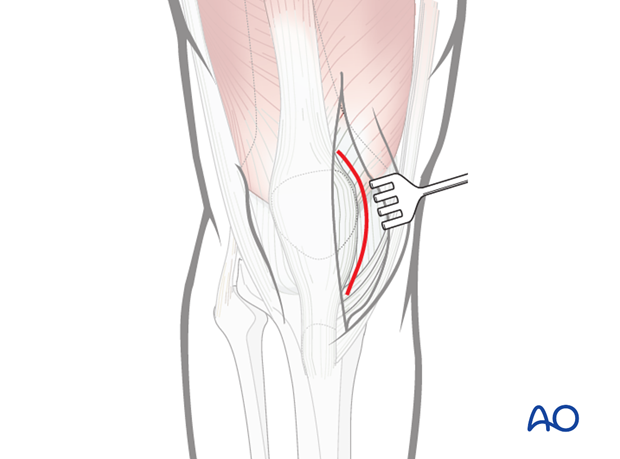
4. Skin incision
Make a longitudinal, slightly oblique, medial parapatellar incision along a line starting 5 cm above the superior pole of the patella to the tibial tubercle.
Flaps should not be raised so as to avoid damage to skin blood supply.

5. Opening of the knee joint
Incise the medial patellar retinaculum and open the joint capsule.
6. Proximal and distal extensions
Depending on the fracture configuration, the incision can be extended proximally to increase the exposure of the distal femur.
The incision can be extended more distally towards the tibial tubercle to increase the exposure of the knee joint.
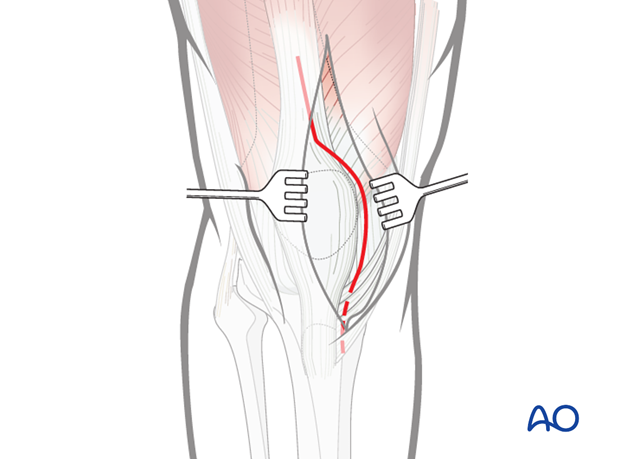
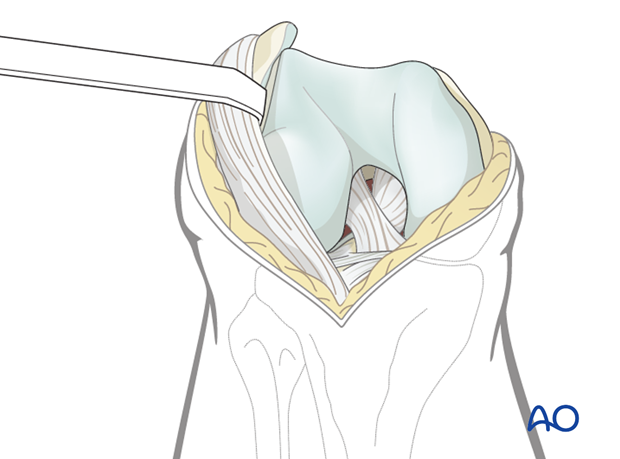
7. Reflection of the patella and extensor retinaculum
With enough extension of the incision, the patella can be dislocated laterally. Be careful to avoid avulsion of the patellar ligament from the tibial tubercle. To aid exposure of the whole distal femur the incision can be extended proximally into the quadriceps tendon.
A retractor can be used gently to hold the extensor retinaculum laterally.
Once the patella is dislocated, there will be a wide exposure of the knee to aid anatomical articular surface reconstruction.
8. Wound closure
Closure
Close the iliotibial band with absorbable sutures. Close the subcutaneous tissues and skin in a routine manner.













