MIPO approach to the distal femur from lateral/anterolateral
1. Principles
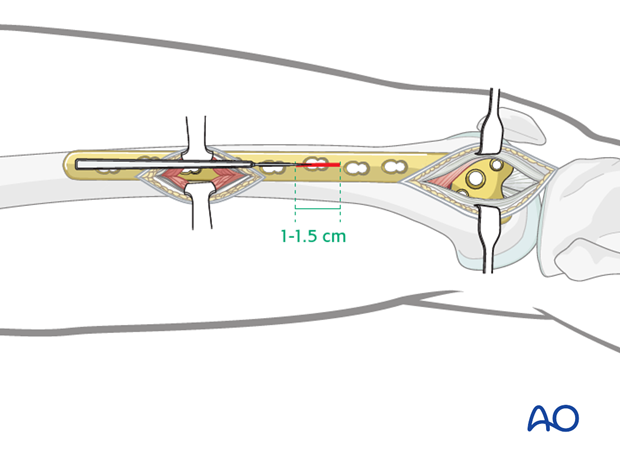
The lateral minimally invasive plate osteosynthesis (MIPO) approach combines a short version of the open lateral approach to the distal femur, a minimally invasive approach to the midshaft or, proximal femoral region, and small 1.0 – 1.5 cm wide stab incisions.
The lateral minimally invasive plate osteosynthesis (MIPO) approach combines
- A shorter version of the open lateral approach to the distal femur (with or without joint arthrotomy). Click here for the open lateral approach.
- A minimally invasive approach to the midshaft, which aids the surgeon in ensuring that the plate is in the appropriate position on the more proximal aspect of the femur
- Small 1.0 – 1.5 cm stab incisions for percutaneous screw placement
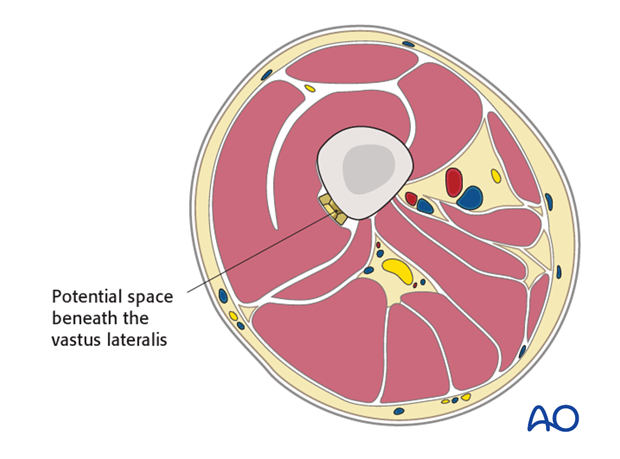
The plate is slid in a submuscular manner in a natural potential space beneath the vastus lateralis.
2. Prophylactic antibiotics
Antibiotics are administered according to local antibiotic policy and specific patient requirements. Many surgeons use gram-positive prophylactic antibiotic cover for closed fractures, adding gram-negative prophylactic cover for open fractures.
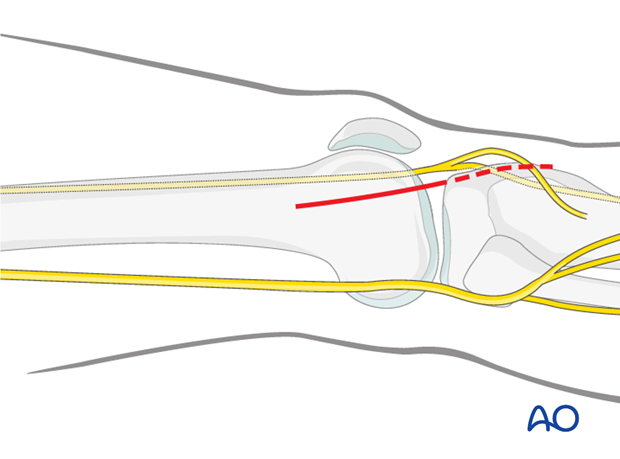
3. Distal approach
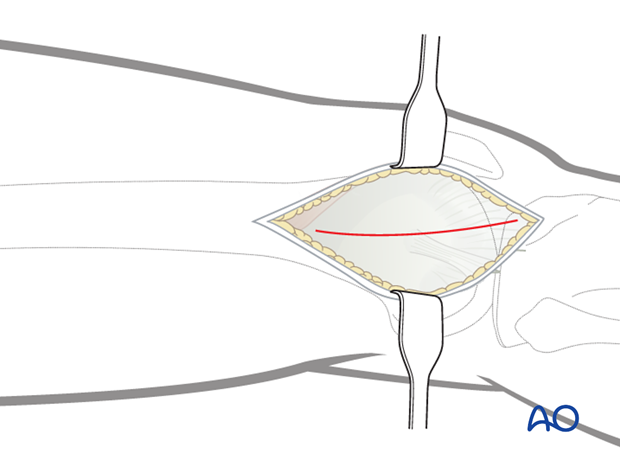
Skin incision
The skin incision for minimally invasive plate osteosynthesis of a distal femoral fracture is simply a shorter version of the open lateral approach to the distal femur.
As with the standard open lateral approach, the distal extent of the incision depends on the need for an arthrotomy. However, the proximal extent is shorter as the plate will be slid into a submuscular tunnel.
The proximal starting point for the skin incision is in the metaphyseal region of the femur.
The distal extension of the skin incision is dependent on whether or not an arthrotomy needs to be performed.
If joint exposure is needed, the incision is carried to the level of Gerdy's tubercle (dashed line).
If an arthrotomy is not necessary, the skin incision can stop approximately 1-2 cm distal to the joint line.
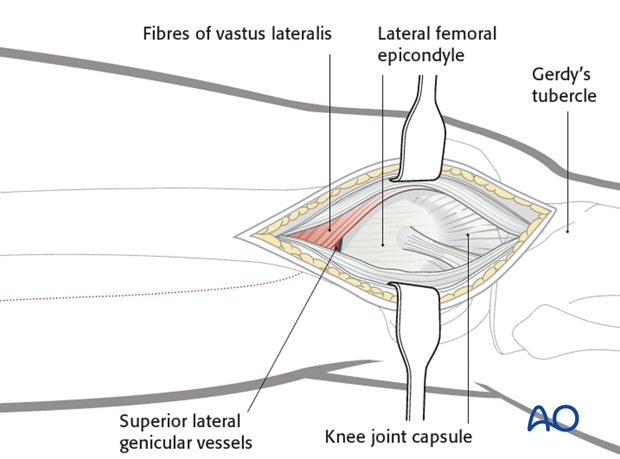
Division the iliotibial band (tract)
Divide the iliotibial band (tract) in line with the skin incision. Distally, the fibers slope anteriorly towards the Gerdy's tubercle. The incision through the iliotibial band should follow the fiber orientation.
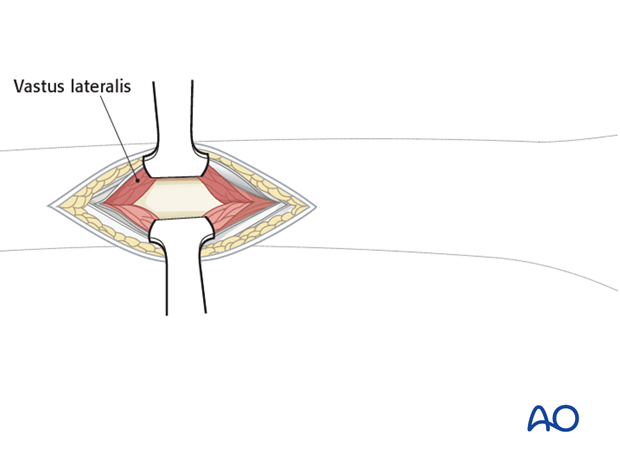
Vastus lateralis
Key point: Unlike the standard lateral approach to the distal femur, in the MIPO approach the vastus lateralis is left generally undisturbed. The muscle fibers of the vastus lateralis are minimal in the distal 8-10 cm of the femur. Therefore, if a joint arthrotomy is not performed the lateral aspect of the distal femur for minimally invasive osteosynthesis is exposed once the surgeon has divided the iliotibial band.
Branches of the superior lateral genicular artery/vein will need to be cauterized.
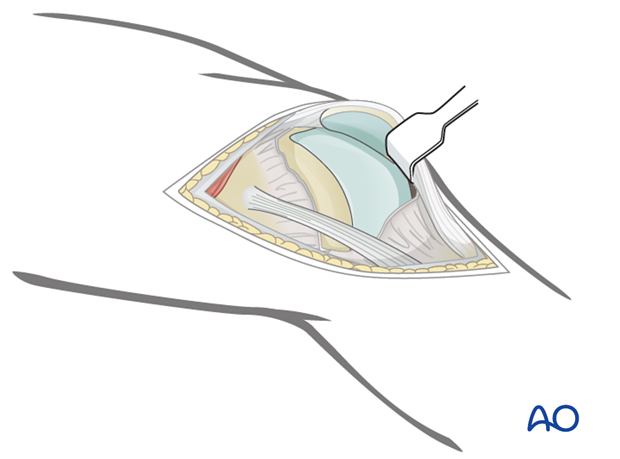
Visualization of the articular surface
Joint capsule arthrotomyFor cases in which the articular surface needs to be visualized, perform a joint capsule arthrotomy.
This requires distal extension of the wound by approximately 3-4 cm.
Distally, incise the joint capsule over the anterior third of the lateral femoral condyle. You can carry this joint arthrotomy distally as far as the anterior portion of the lateral meniscus.
To facilitate exposure of the articular surface, use a blunt angled retractor. Take care to avoid excessive tension on the patellar tendon, especially in osteoporotic individuals.
Closure
Close any joint capsule arthrotomy and the iliotibial band with absorbable sutures. Close the skin and the subcutaneous tissues in a routine manner.
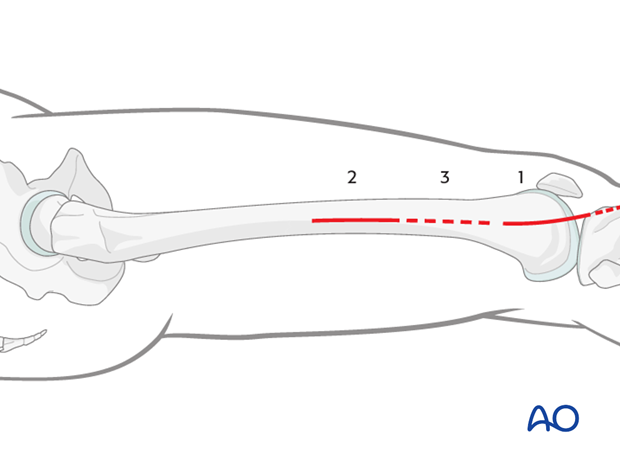
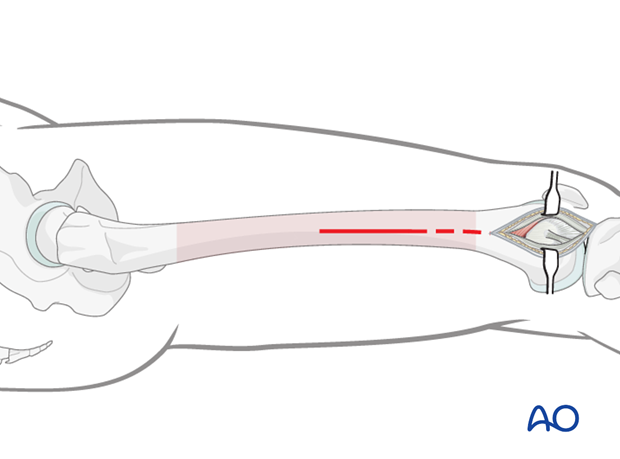
4. Minimally invasive approach to the midshaft or proximal femoral region
Skin incision
Make a short incision along an imaginary line (dashed line) between the lateral femoral epicondyle and the greater trochanter.
The starting point and the length of the incision depend on the operational requirements for the minimally invasive procedure.
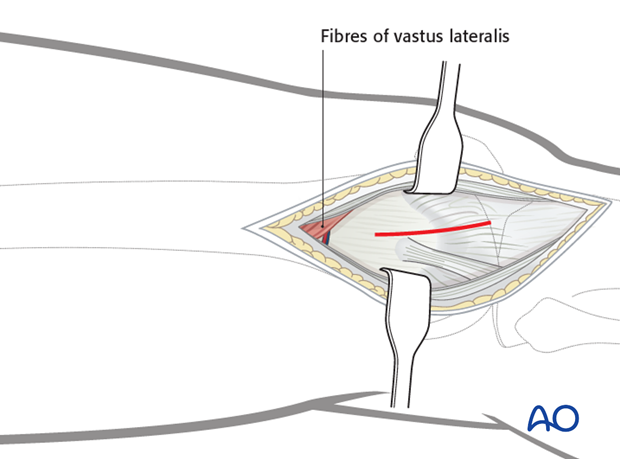
Dissection
Incise the fascia lata and expose the muscle fascia of the vastus lateralis.
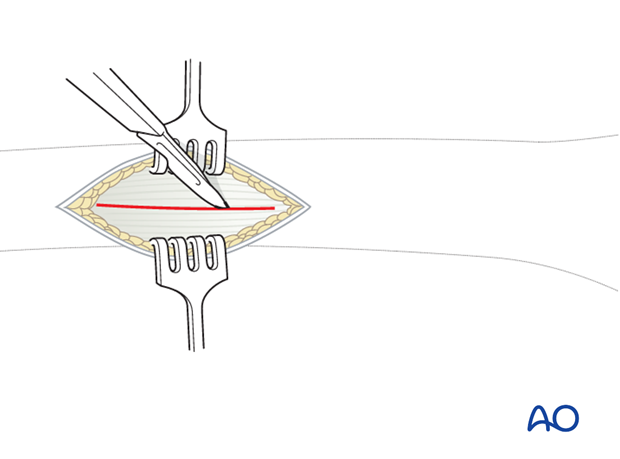
Carefully incise the muscle fascia of the vastus lateralis.
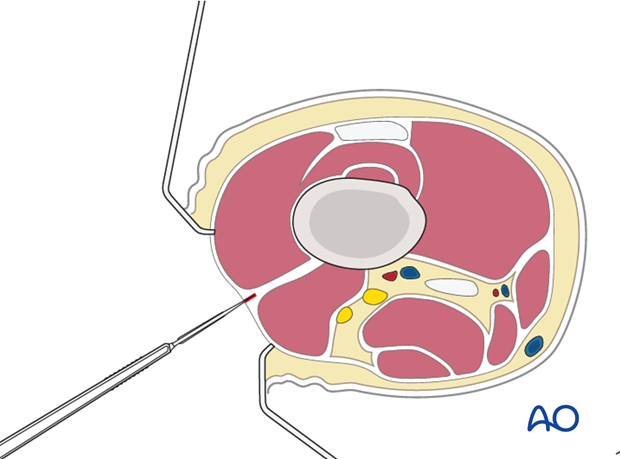
Dissect the muscle fibers apart bluntly down to the femur. Normally, with a formal approach to the lateral aspect of the femur, the entire muscle belly of the vastus lateralis is elevated anteriorly from the lateral intermuscular septum. However, with minimally invasive techniques, this is not possible. Therefore, the muscle belly is split in the line of its fibers to approach the lateral aspect of the femur.
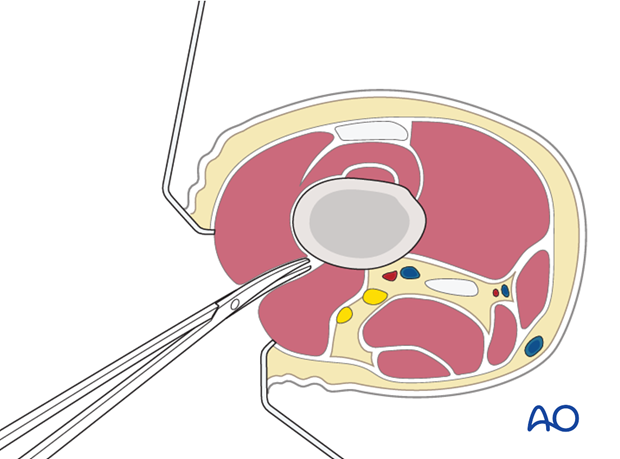
Retraction
Two Hohmann retractors are recommended - one anterior and one posterior - for a secure exposure of the femoral shaft.
Hohmann retractors ensure appropriate plate positioning on the femur. It is wise first to ensure that the most proximal screw hole of the plate is centrally located, before any other screws are inserted in the proximal plate.
Closure
Close the iliotibial band with absorbable sutures. Close the subcutaneous tissues and skin in a routine manner.
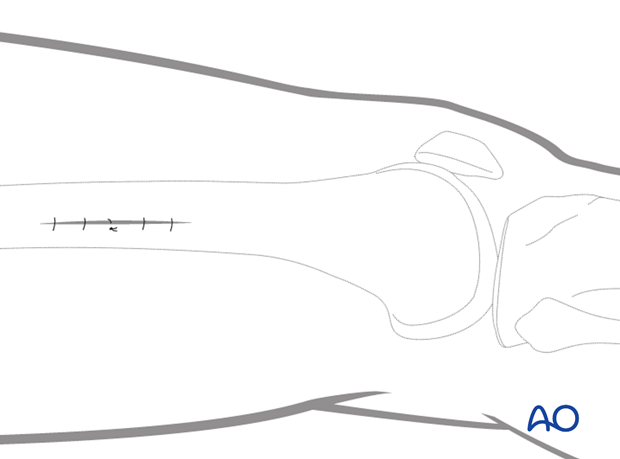
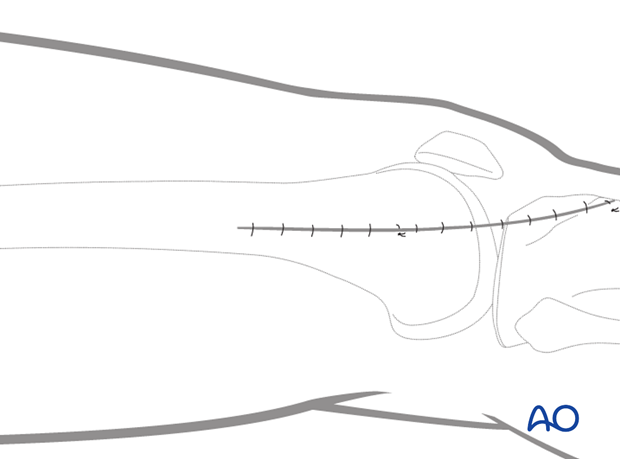
5. Stab incisions for percutaneous screw placement
Incision
Make a 1-1.5 cm wide incision in line with the screw hole of the plate. This incision is made as a single stab through the skin, subcutaneous tissue, iliotibial band, fascia of the vastus lateralis and finally through the muscle belly of the vastus lateralis. A common mistake is to make the stab incision too small. A 1–1.5 cm wide incision is sufficient for most screw insertions.
If two screws need to be placed close to each other a smaller version of the lateral approach to the femur can be used for this purpose.
Closure
Close the iliotibial band with absorbable sutures. Close the subcutaneous tissues and skin in a routine manner.