Lateral parapatellar approach to the distal femur
1. Introduction
The lateral parapatellar approach provides a good view of the articular surface of the distal femur. With a longitudinal division of the quadriceps tendon and extensor mechanism, the patella can be dislocated medially.
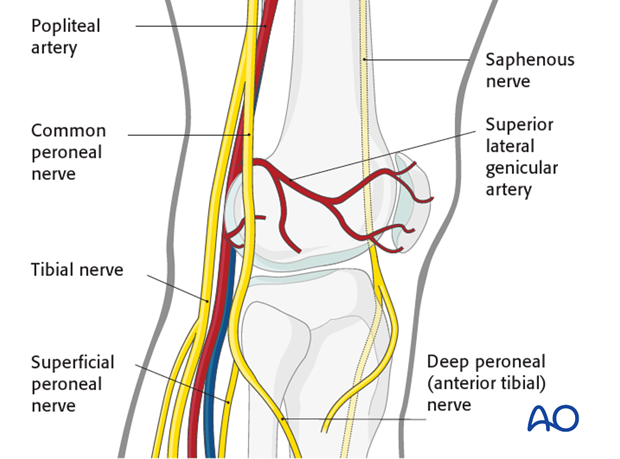
Neurovascular considerations
StructuresIn general, there are no neurovascular structures at risk. The common peroneal nerve is safe posterior and distal to the approach.
There is only the lateral superior genicular artery to avoid or ligate.
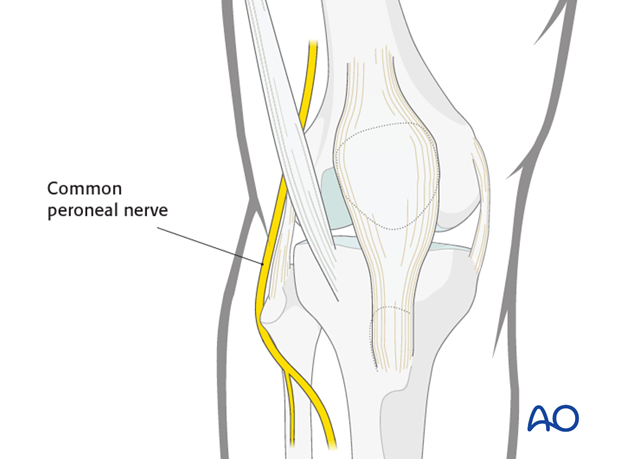
The surgical approach exploits only the extensor mechanism. No significant neurovascular risks are present.
Extensions of the lateral parapatellar approach
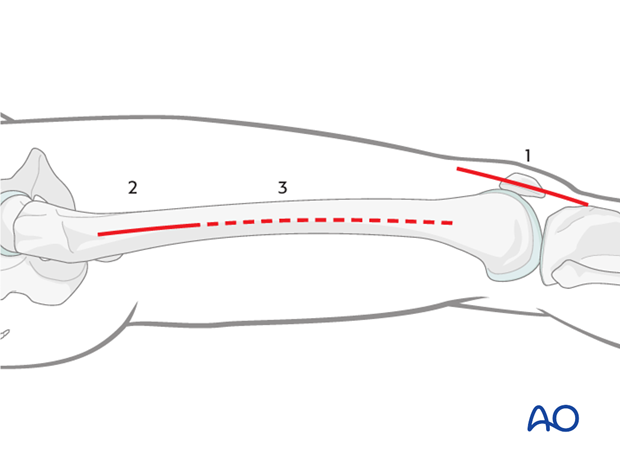
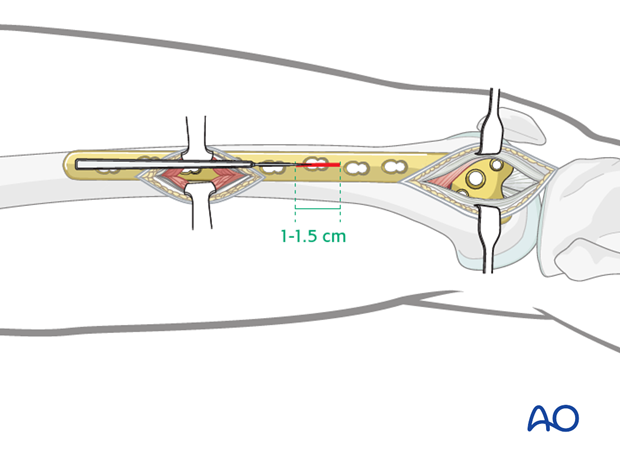
For most intra articular distal femoral fractures, the lateral parapatellar approach (1) includes:
- A minimally invasive approach to the midshaft, or proximal, femoral region (2), which aids the surgeon in ensuring that the plate is in the appropriate position on the proximal, lateral aspect of the femur
- Small 1.0–1.5 cm stab incisions for percutaneous screw insertion (3)
The lateral parapatellar approach may also be used in isolation (only using incision 1) for lateral sagittal or coronal fractures, in which a plate is not inserted by sliding into a submuscular tunnel.
Teaching video
This video demonstrates the lateral parapatellar approach for the reduction and fixation of the articular block as well as the insertion of an LCP plate in a minimally invasive manner. The LISS plate is used.
2. The lateral parapatellar approach
Skin incision
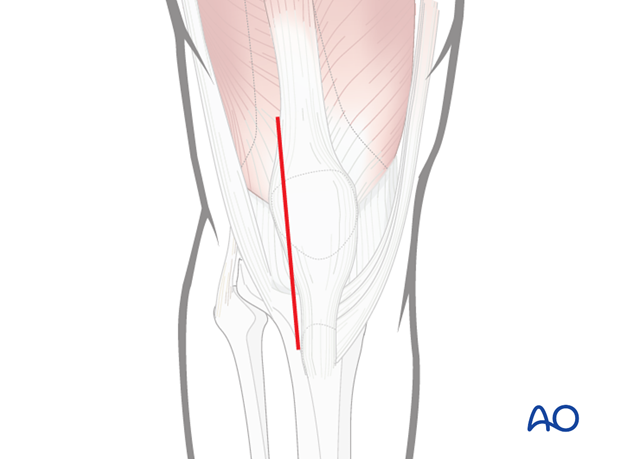
Place a rolled towel under the knee to produce 20° to 30° of knee flexion.
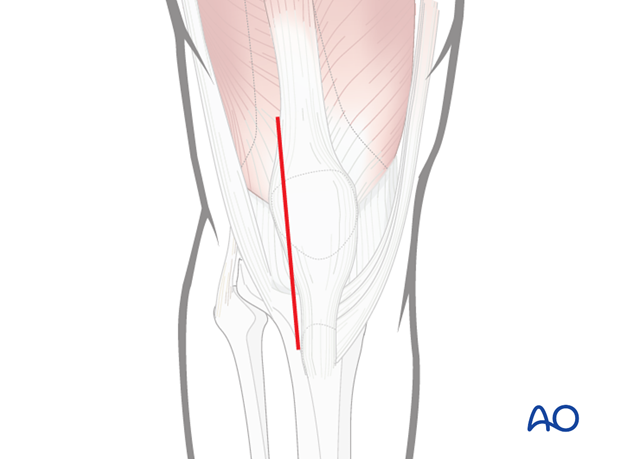
Mark the tibial tubercle and the patella. The incision can be either directly midline, or preferably, slightly lateral to midline (as shown).
A common mistake is to make the incision too short, which will later on not permit medial patellar dislocation. The incision is generally 15–18 cm in length.
Deep dissection
Deep dissection exposes the lateral aspect of the patella.
The extensor retinaculum is preserved over the front of the patella.
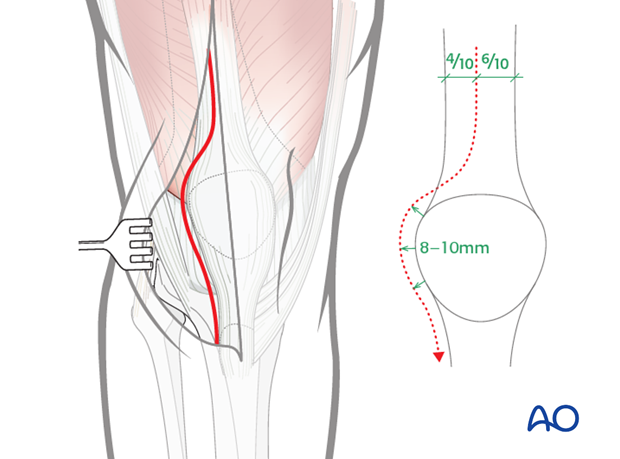
The skin incision is long enough for the surgeon to define both the medial and the lateral aspects of the quadriceps tendon.
Make a full thickness, longitudinal incision through the lateral parapatellar retinaculum and the quadriceps tendon. It begins slightly lateral to midline (40% lateral; 60% medial) and curves to the lateral aspect of the patella. It should leave an 8–10 mm cuff of parapatellar retinaculum on the lateral aspect of the patella.
The split in the quadriceps tendon extends approximately 10 cm above the superior pole of the patella. If an adequate release is not performed, the surgeon risks patellar tendon avulsion during patellar dislocation.
Distal extension of the deep dissection
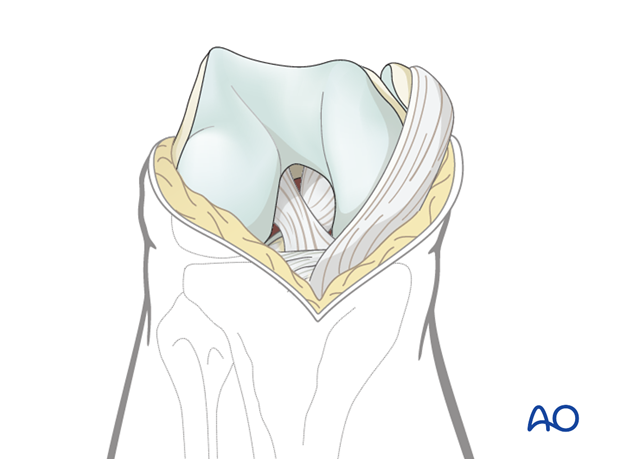
Carry the division down distally to the lateral aspect of the patellar tendon and then, by flexion of the knee and medial traction on the extensor mechanism, the patella is dislocated medially.
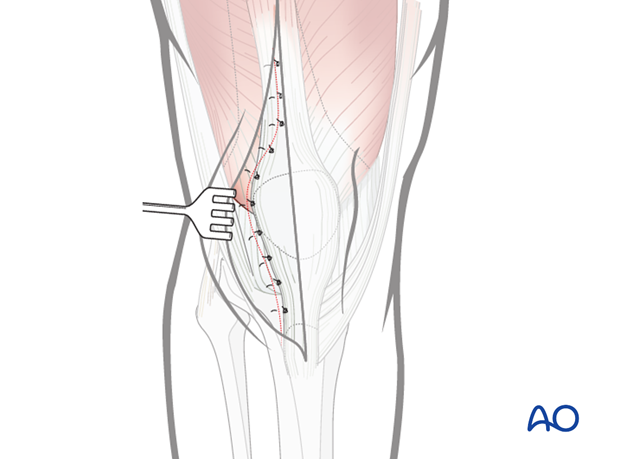
Wound closure
Close the quadriceps tendon and cuff of tissue along the lateral aspect of the patella with interrupted #2, or larger, sutures. Close the skin and subcutaneous tissue in a routine manner.
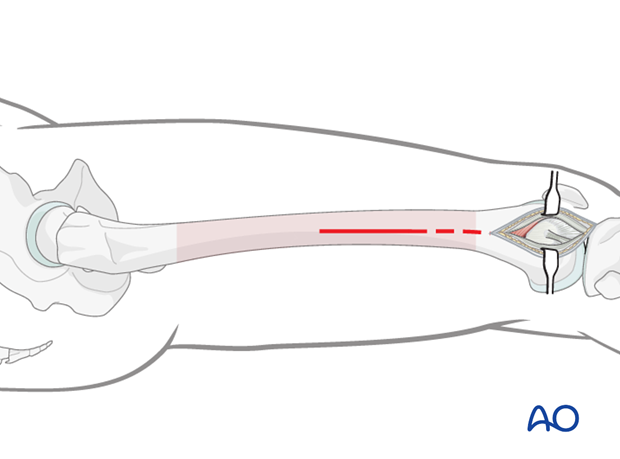
3. Minimally invasive approach to the midshaft or proximal femoral region
Skin incision
Make a short incision along an imaginary line (dashed line) between the lateral femoral epicondyle and the greater trochanter.
The starting point and the length of the incision depend on the operational requirements for the minimally invasive procedure.
Dissection
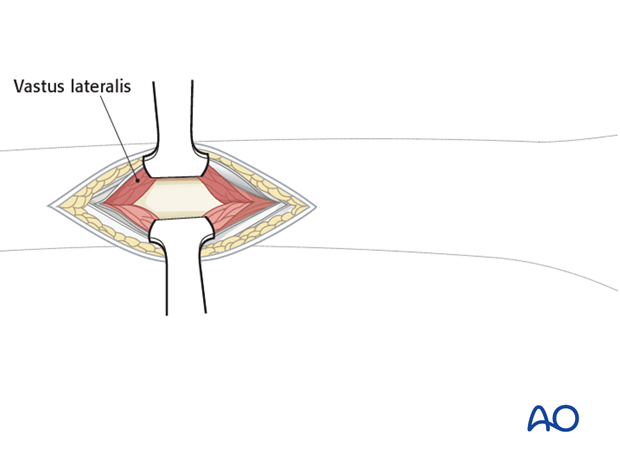
Incise the fascia lata and expose the muscle fascia of the vastus lateralis.
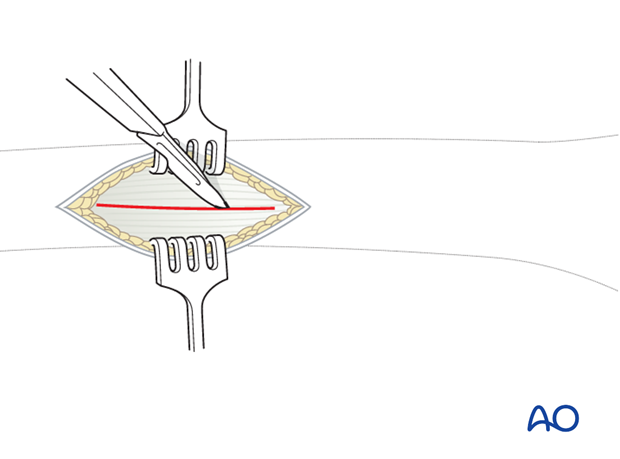
Carefully incise the muscle fascia of the vastus lateralis.
Dissect the muscle fibers apart bluntly down to the femur. Normally, with a formal approach to the lateral aspect of the femur, the entire muscle belly of the vastus lateralis is elevated anteriorly from the lateral intermuscular septum. However, with minimally invasive techniques, this is not possible. Therefore, the muscle belly is split in the line of its fibers to approach the lateral aspect of the femur.
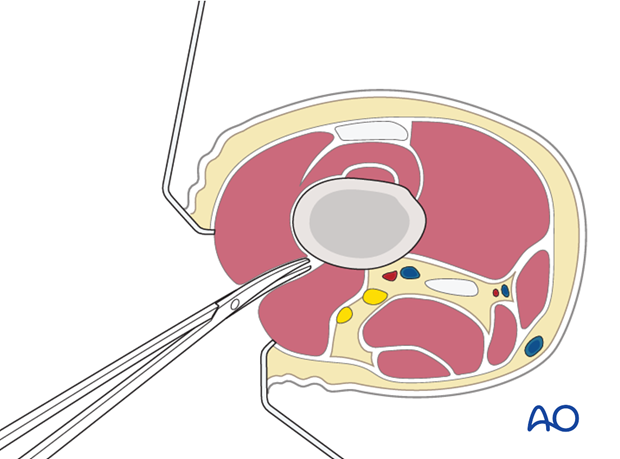
Retraction
Two Hohmann retractors are recommended - one anterior and one posterior - for a secure exposure of the femoral shaft.
Hohmann retractors ensure appropriate plate positioning on the femur. It is wise first to ensure that the most proximal screw hole of the plate is centrally located, before any other screws are inserted in the proximal plate.
Closure
Close the iliotibial band with absorbable sutures. Close the subcutaneous tissues and skin in a routine manner.
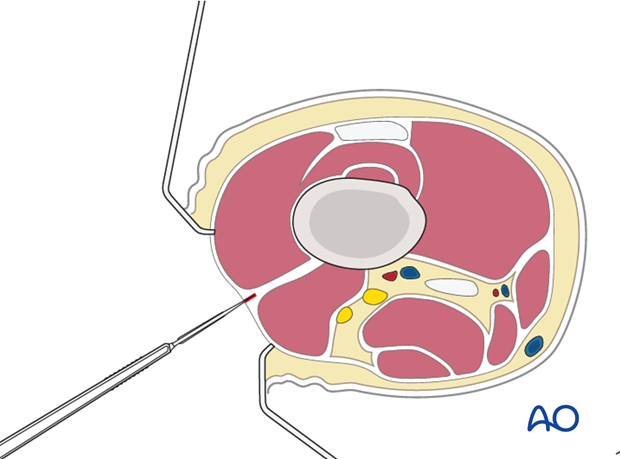
4. Stab incisions for percutaneous screw placement
Incision
Make a 1-1.5 cm wide incision in line with the screw hole of the plate. This incision is made as a single stab through the skin, subcutaneous tissue, iliotibial band, fascia of the vastus lateralis and finally through the muscle belly of the vastus lateralis. A common mistake is to make the stab incision too small. A 1–1.5 cm wide incision is sufficient for most screw insertions.
If two screws need to be placed close to each other a smaller version of the lateral approach to the femur can be used for this purpose.
Closure
Close the iliotibial band with absorbable sutures. Close the subcutaneous tissues and skin in a routine manner.
5. Case
Lateral parapatellar approach with surface landmarks indicated, showing patella and tibial tubercle.
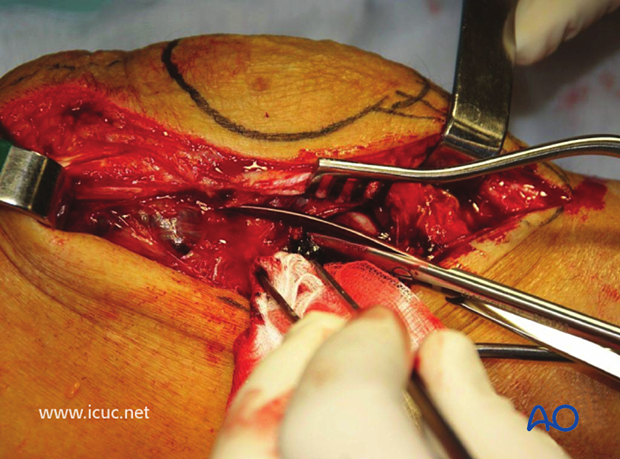
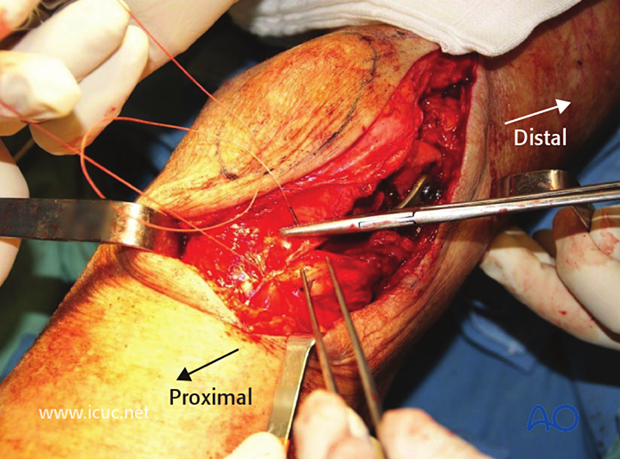
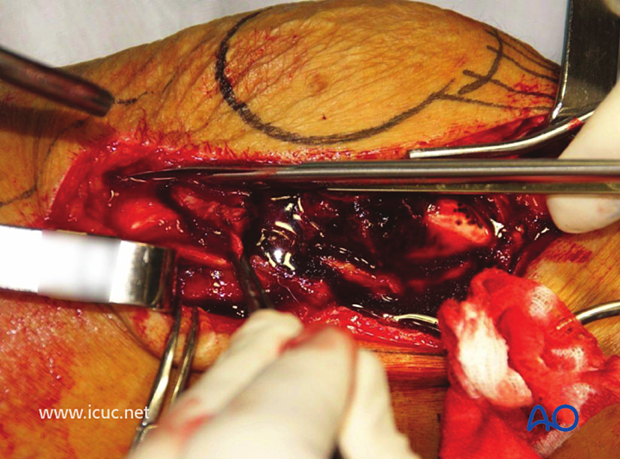
The approach has been deepened with the identification of the tensor fascia lata and lateral retinaculum. The patella and quadriceps are retracted medially so that the whole distal lateral femur will be visualized.
This image shows the patella retracted medially with the patellar tendon attached to the tibial tuberosity, but the whole of the distal femur can be visualized. This makes it easier to achieve anatomic reduction.
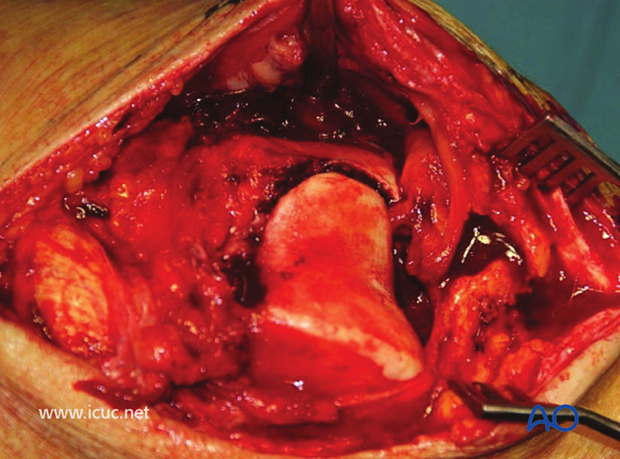
This shows the extent of the approach proximally and distally. Note that the metaphyseal region (which is commonly fractured) is not seen and left with its blood supply intact.
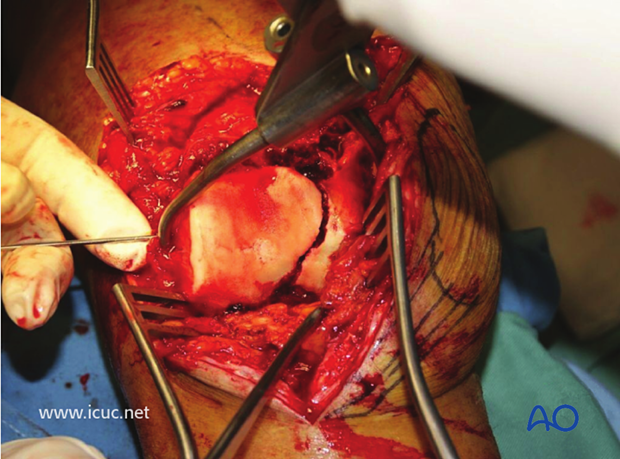
This image shows closure of the lateral parapatellar approach with a heavy suture approximating the tensor fascia lata and the lateral retinaculum.