Double plating
1. Principles
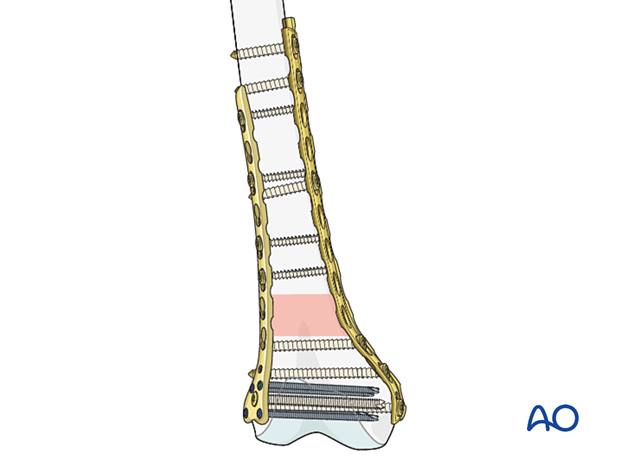
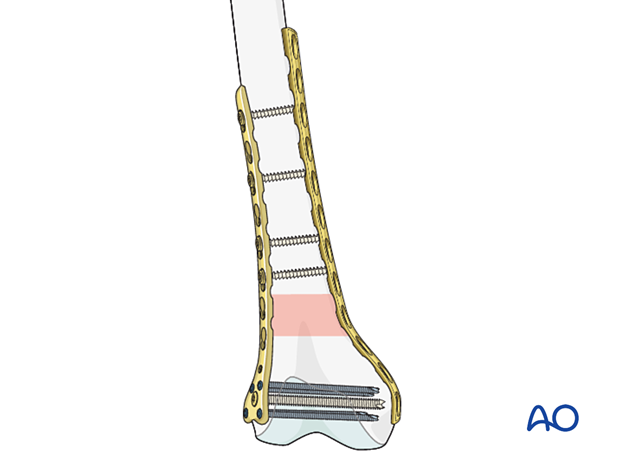
Principle of double plating
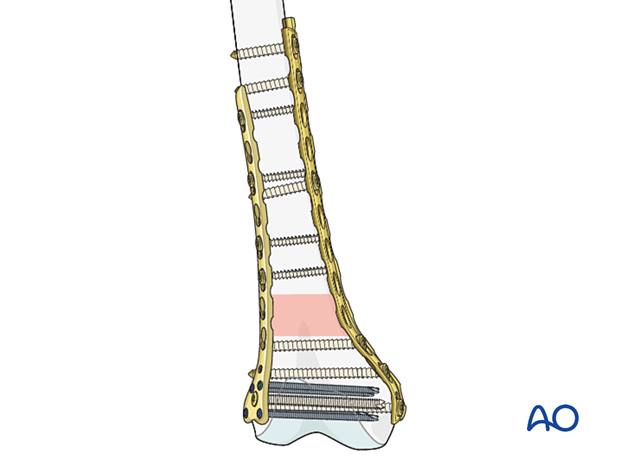
This technique is used when the biomechanical advantage of a single plate is not ideal. The double plate, with medial and lateral plates, provides much more biomechanical stability where a mulfragmentary fracture pattern, particularly in the presence of osteoporosis, makes stability a challenge.
The strategy is similar to other types of fixation in that the articular block must still be reconstructed but two plates are used maintain the reduction between the proximal and distal end segment. This is a bridge plate construct.
In instances of osteoporosis, locking fixation is virtually always used.
As most surgeons have more experience in lateral plate fixation (compared to medial fixation) most surgeons will perform reduction and plate fixation on the lateral side first.
The medial incision is then made, and a surgeon-contoured plate is then added to provide additional stability.
Plate selection
The lateral side is usually plated with an LCP as these plates are readily available.
The medial side will accommodate a surgeon-contoured plate which can be a LCDCP or a LCP.
Another adjunct in such situations is an intrameddulary cortical allograft strut or intramedullary plate, however, this will not be described in detail here.
2. Patient preparation and approach
Patient positioning
This procedure may be performed with the patient in one of the following positions:
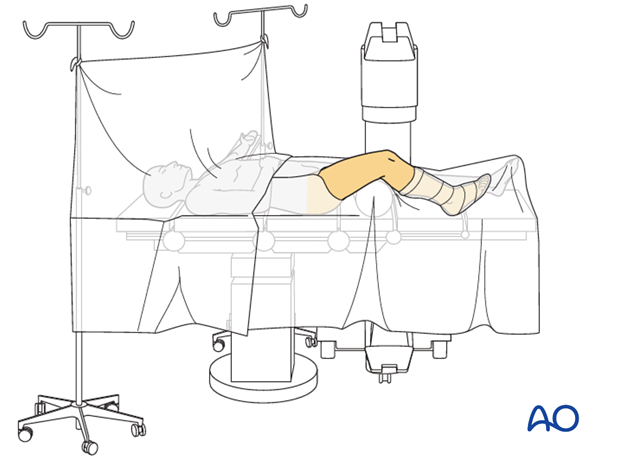
Selection of approach
Fixation of the articular blockThese difficult fractures will require a parapatellar approach for articular block reduction and fixation.
The lateral plating can be performed through either of these two approaches:
In most instances, a MIP approach to the medial distal femur is used. This can involve a:
- Medial approach to the distal femur
- Medial parapatellar approach
- Medial subvastus approach (not described here).
Proximal plate fixation typically involves a small incision at the proximal end of the plate.
3. Lateral plate
For the insertion of the lateral bridging plate, please refer to the procedure for the insertion of a single lateral plate (in bridging mode).
4. Medial plate
Plate selection
The distal medial femoral anatomy requires appropriate contouring of a plate.
Either a 3.5 or 4.5 LCP or a LCDCP can be used, but careful contouring must be performed with the use of a malleable template.
A bending press and careful contouring is necessary for both plates. To demonstrate the principles, we will here show the use of a LCDCP.
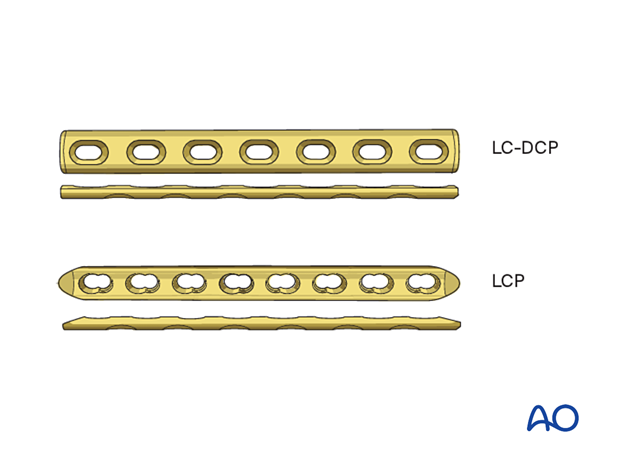
Plate contouring
A malleable template is used to precisely contour the LCDCP to fit the medial aspect of the reconstructed distal femur.
The length of the plate is less dogmatic as it is only biomechanically supporting the LCP fixation on the lateral side. But, usually this plate should have at least two bicortical screws proximally and distally.
The plate should extend as far distally as possible but remain subchondral after screw insertion, and thus achieving the strongest possible fixation.
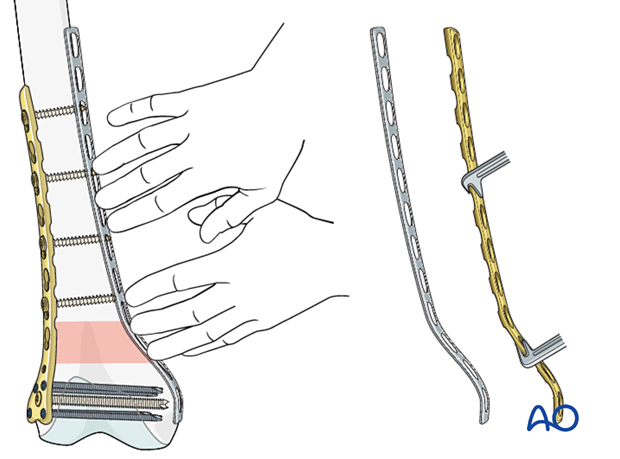
The contoured plate is placed on the medial distal femur to check for accurate contouring.
If the contouring is satisfactory, the plate is fixed to the bone by first inserting a screw in the distal screw hole.
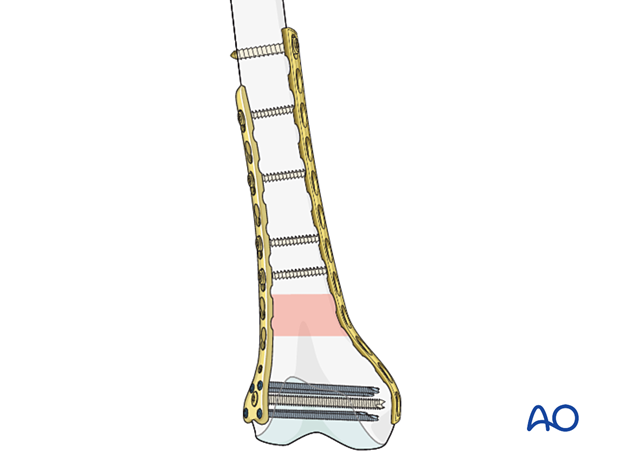
Then, the most proximal screw is inserted with fluoroscopic review in all planes to ensure that the distal femur is accurately reduced.
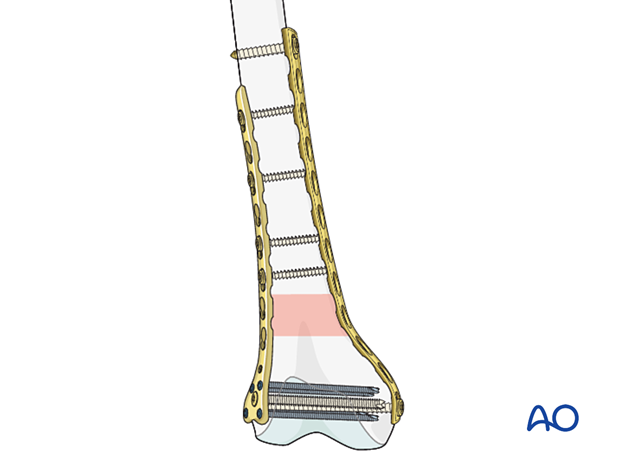
The final two screws are inserted. The distal femur with two plates applied has many screws in the distal articular block. Although this is a bridge plate construct, these multifragmentary fractures require enhanced biomechanical stability.
Final check of fracture reduction and fixation
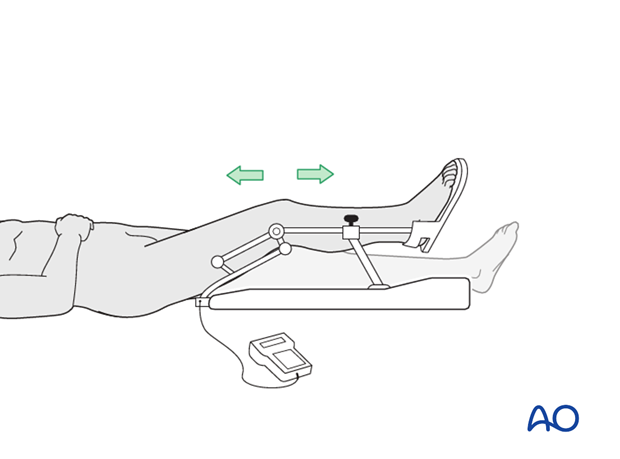
Gently move the knee through a full range of motion. Carry out a clinical assessment of the rotational profile. Finally, perform a radiographic assessment of the frontal-plane alignment (varus/valgus) and sagittal-plane alignment (extension/flexion).
Examine the knee for any ligamentous instability.
5. Aftercare
Impediments to the restoration of full knee function after distal femoral fracture are fibrosis and adhesion of injured soft tissues around the metaphyseal fracture zone, joint capsular scarring, intra-articular adhesions, and muscle weakness.
Early range of motion helps restore movement in the early postoperative phase. With stable fracture fixation, the surgeon and the physical therapy staff will design an individual program of progressive rehabilitation for each patient.
The regimens suggested here are for guidance only and not to be regarded as prescriptive.
Functional treatment
Unless there are other injuries or complications, knee mobilization may be started immediately postoperatively. Both active and passive motion of the knee and hip can be initiated immediately postoperatively. Emphasis should be placed on progressive quadriceps strengthening and straight leg raises. Static cycling without load, as well as firm passive range of motion exercises of the knee, allow the patient to regain optimal range of motion.
Weight bearing
Touch-down weight-bearing (10-15 kg) may be performed immediately with crutches, or a walker. This will be continued for 6-10 weeks postoperatively. This is mostly to protect the articular component of the injury, rather than the shaft injury. Touch-down weight-bearing progresses to full weight-bearing gradually, over a period of 2 to 3 weeks (beginning at 6–10 weeks postoperatively). Ideally, patients are fully weight-bearing, without devices (e.g., cane) by 12 weeks.
Follow-up
Wound healing should be assessed at two to three weeks postoperatively. Subsequently 6-week, 12-week, 6-month, and 12-month follow-ups are usually made. Serial x-rays allow the surgeon to assess the healing of the fracture.
Implant removal
Implant removal is not essential but should be discussed with the patient if there are implant-related symptoms after consolidated fracture healing.
Thrombo-embolic prophylaxis
Thrombo-prophylaxis should be given according to local treatment guidelines.













