Lateral/anterolateral approach to the distal femur
1. General considerations
The lateral approach allows for visualization, reduction, and fixation of simple articular fractures of the distal femur. More complex fractures (particularly those involving the medial femoral condyle) are better exposed with a lateral or medial parapatellar approach.
The lateral approach relies on an atraumatic elevation of the vastus lateralis from the lateral aspect of the distal femur, and a lateral arthrotomy for joint visualization. Articular reduction and lateral plate application can both be achieved with the same approach. Additionally, the approach can be extended proximally, as described in the lateral approach to the femoral shaft.
The approach can also be used without an arthrotomy if the articular surface is not fractured.
2. Prophylactic antibiotics
Antibiotics are administered according to local antibiotic policy and specific patient requirements. Many surgeons use a gram-positive prophylactic antibiotic cover for closed fractures, adding gram-negative prophylactic cover for open fractures.
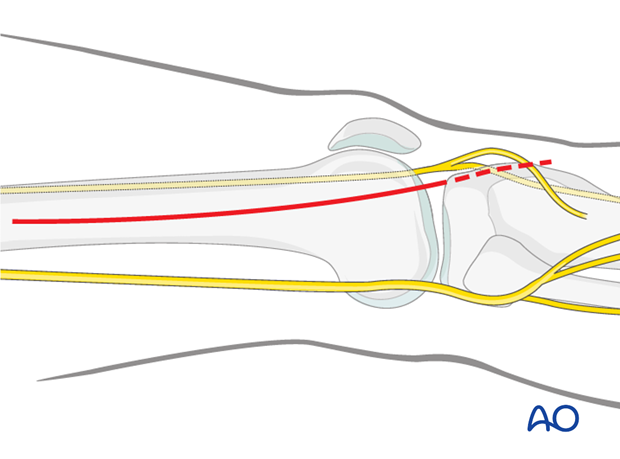
3. Skin incision
Begin the skin incision in the mid-lateral line of the femoral shaft at Gerdy's tubercle and curve it proximally over the lateral femoral condyle.
The proximal starting point for the skin incision depends on the most proximal extent of the fracture.
The need for a distal extension of the skin incision depends on whether an arthrotomy needs to be performed. If joint visualization is required, the incision is carried to the level of the Gerdy's tubercle (dashed line). If an arthrotomy is not necessary, you can stop the skin incision approximately 1-2 cm distal to the joint line.
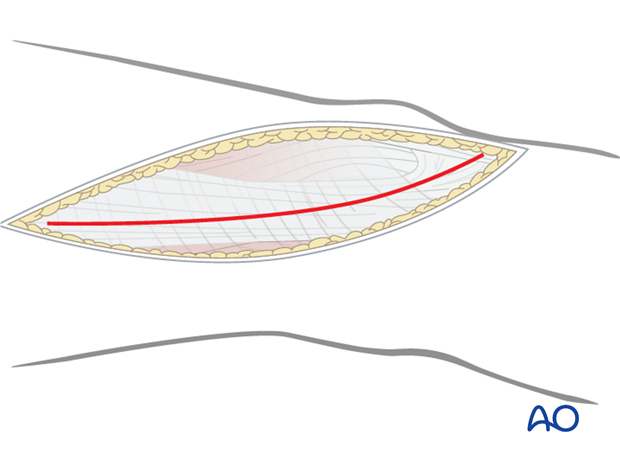
4. Division of the iliotibial band
Divide the iliotibial band (tract) in line with the skin incision. Distally, the fibers slope anteriorly towards the Gerdy's tubercle. The incision through the iliotibial band should follow the muscle fiber orientation. To facilitate a perfect closure, the iliotibial band should be divided in one precise incision only.
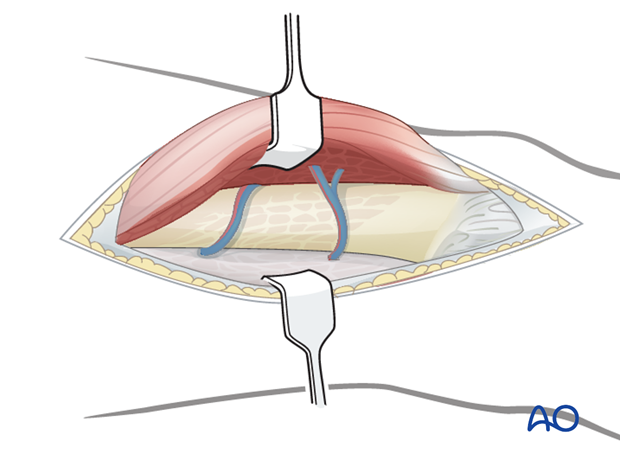
5. Elevation of vastus lateralis
Beneath the iliotibial band, the muscle fibers of the vastus lateralis are minimal in the distal 8-10 cm of the femur. Incise the muscle fascia surrounding the vastus lateralis just anterior to the lateral intermuscular septum and elevate the muscle fibers off the septum, working from distal to proximal. This is most easily accomplished by the use of a large elevator.
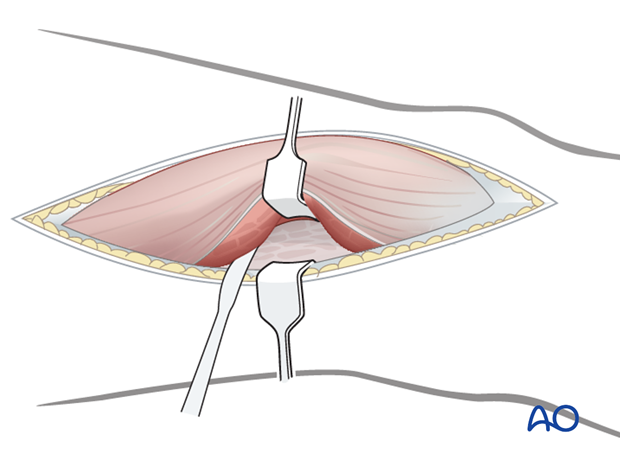
Retract the vastus lateralis anteromedially. Several perforating vessels of the profunda femoris artery and vein must be ligated. Failure to do so will result in excessive bleeding. It is important to only remove muscles from the lateral surface of the distal femur and protect as much periosteum surrounding the distal femur as possible for later fracture healing.
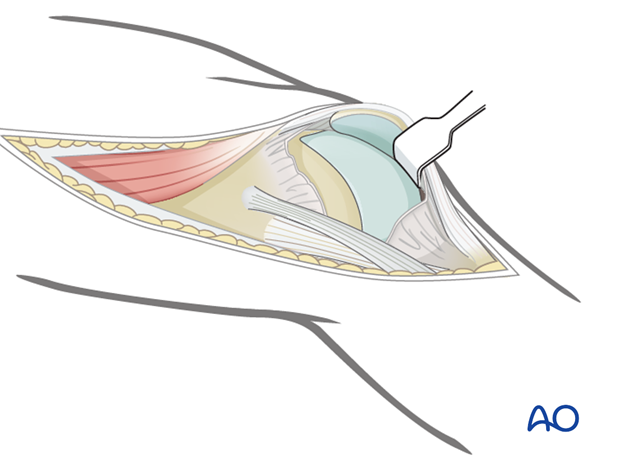
6. Joint capsule arthrotomy for articular surface visualization (optional)
For cases in which the articular surface needs to be exposed, perform a joint capsule arthrotomy.
Distally, incise the joint capsule over the anterior third of the lateral femoral condyle. This joint arthrotomy can be carried distally as far as the lateral meniscus.
To facilitate exposure of the articular surface, use a blunt angled retractor. Take care to avoid excessive tension on the patellar tendon, especially in osteoporotic individuals.
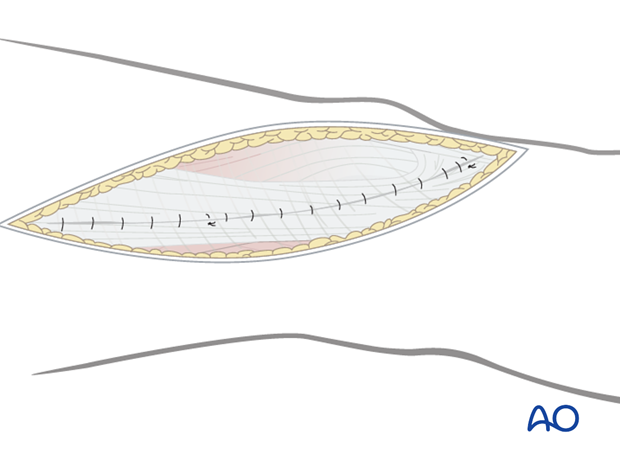
7. Wound closure
Close any joint capsule arthrotomy with absorbable sutures.
Proximally, close the fascia of the vastus lateralis with a running absorbable suture or interrupted sutures.
Close the iliotibial band with absorbable sutures. Close the skin and subcutaneous tissues in a routine manner.