Percutaneous screw fixation through a palmar approach
1. General considerations
Introduction
Scaphoid waist fractures may be fixed with a cannulated headless compression screw (2.4 or 3.0 mm). In nondisplaced fractures, the screw can be applied percutaneously using a palmar approach in a retrograde fashion.
Percutaneous (minimally invasive) treatment brings the advantages of internal fixation without the disadvantages of a wide surgical approach, eg, preserving the palmar ligament complex and local vascularity, and avoiding postoperative immobilization.
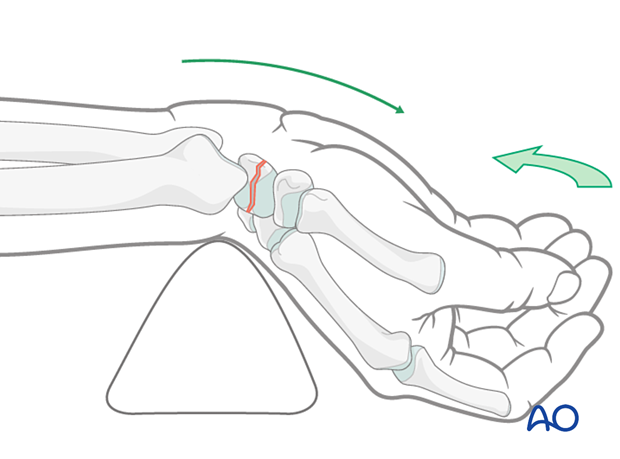
Displaced and oblique fractures need closed reduction with standard reduction maneuvers (hyperextension and ulnar deviation). If these do not lead to adequate reduction, be prepared to switch to ORIF. An oblique fracture in the coronal plane requires most often ORIF.
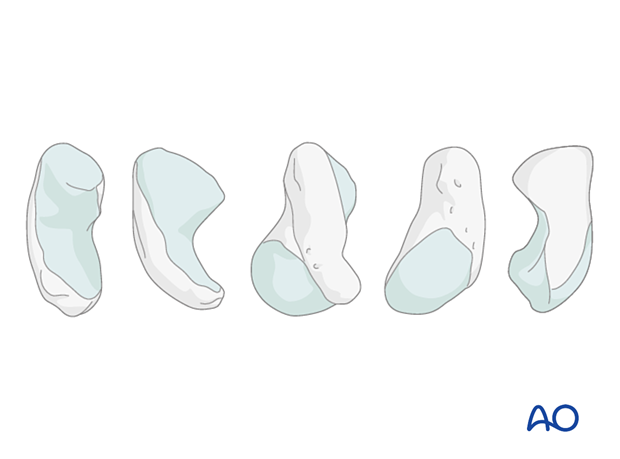
Anatomical considerations
80% of the surface of the scaphoid is covered with articular cartilage. This greatly limits potential points of entry for fixation devices.
An additional constraint is the curved shape of the scaphoid.
This means that a wire or fixation device along the true central axis of the scaphoid is not possible from a palmar approach. Occasionally, access to a distal entry point for a device can only be gained by a limited excavation of the edge of the trapezium.
Preoperative planning
Conventional radiographs do not adequately demonstrate the complete fracture configuration. A CT scan is recommended if a percutaneous procedure is planned.
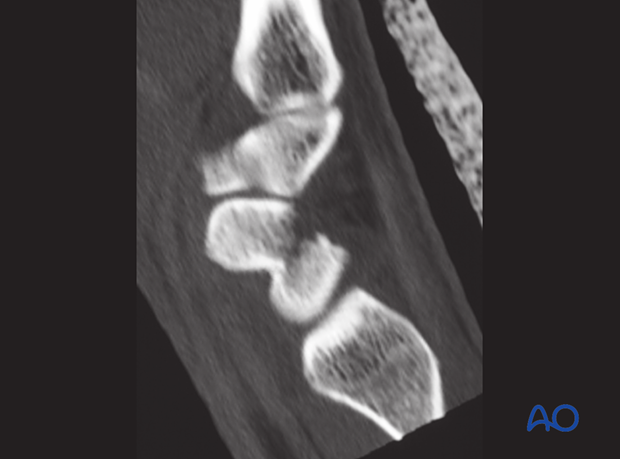
Before starting the surgical procedure, reexamine the fracture pattern under the image intensifier. Ensure the fracture is suitable for a percutaneous technique and that no secondary displacement has occurred. This is especially indicated for displaced or oblique fractures.
AO teaching video
Scaphoid-Fracture – Percutaneous Fixation with the 3.0 mm Headless Compression Screw (HCS)
At 9:28, a clinical case shows the steps for percutaneous screw fixation of a scaphoid fracture.
2. Patient preparation
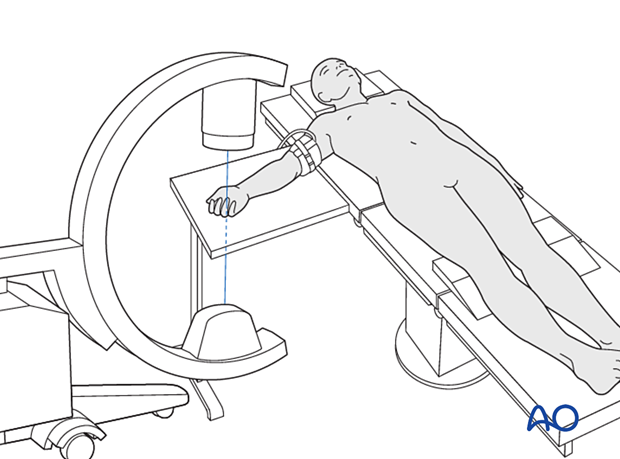
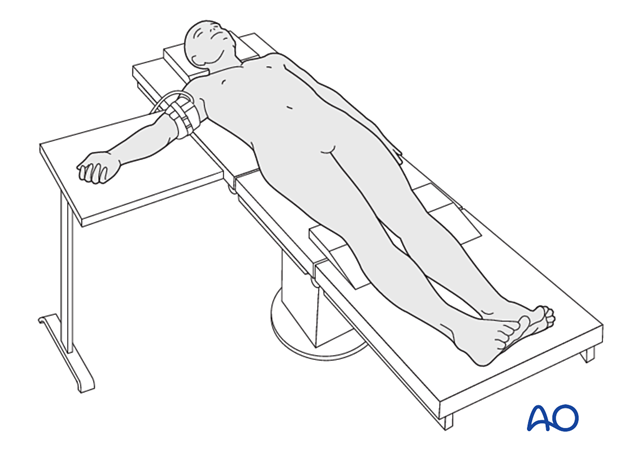
The patient is usually supine with the arm on a radiolucent side table.
3. Preliminary reduction
Hyperextension and ulnar deviation of the wrist will facilitate any necessary fracture reduction.
Hyperextension also assists in bringing the trapezium dorsal to the insertion point of the guide wire at the scaphoid tubercle.
Check with an image intensifier if adequate reduction has been achieved.
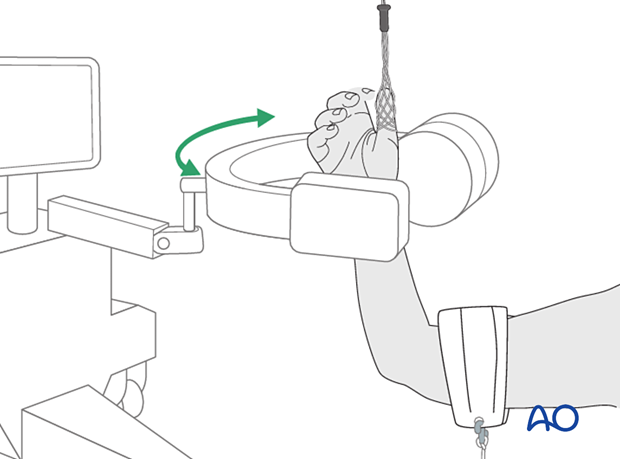
Alternative: reduction by traction
This setup allows the surgeon to check the reduction quality and a possibility to use arthroscopy if needed.
The thumb is suspended by a single ‘finger-trap’. The wrist is in mild ulnar deviation and extension. The C-arm is oriented horizontally around the patient’s wrist.
There is limited dorsiflexion of the wrist possible. If necessary, reduction can be performed with K-wires as joysticks.
4. Guide-wire insertion
Insertion point for the guide wire
Use a hypodermic needle to determine the insertion point radiologically before inserting the guide wire.
The insertion point is on the distal surface of the scaphoid tubercle, at the edge of the scaphotrapezial joint. If the fracture plane dictates, a transtrapezial approach should be used.
The wire trajectory should aim for the proximal pole of the scaphoid.
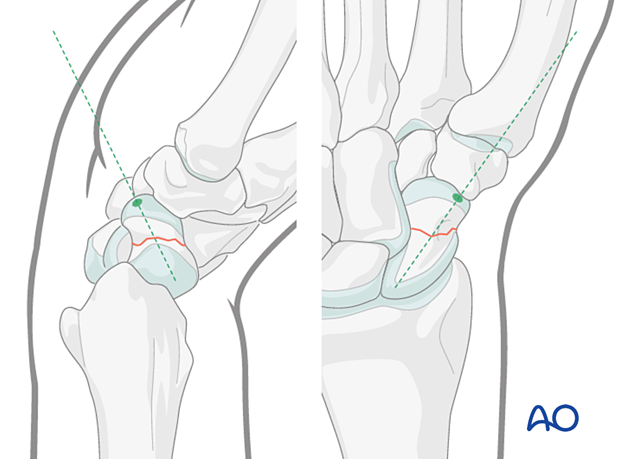
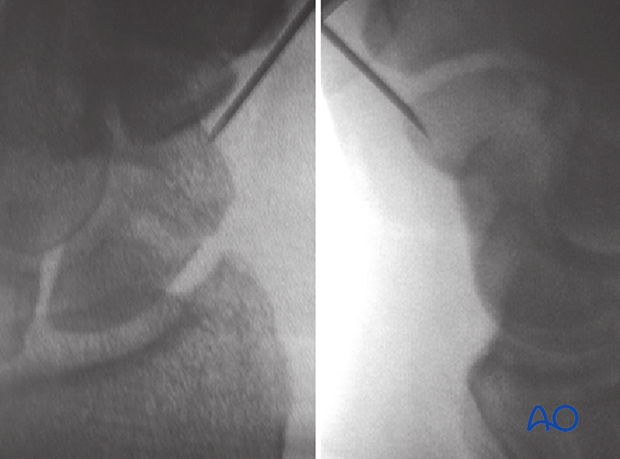
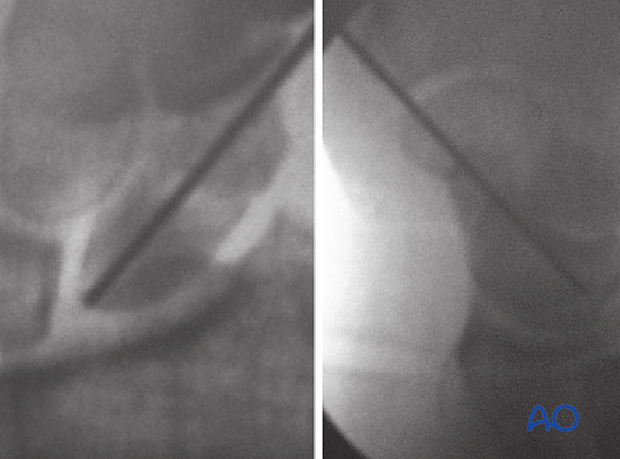
This case shows AP and lateral views with the tip of the needle and the insertion point.
Skin incisions
Perform a short stab incision distally to the scaphotrapezial joint.
For a complete description of the landmarks and the siting of this incision, click here.

Insertion of the guide wire
Insert the guide wire at the confirmed entry point through a drill guide.
If no drill guide is available, use a protective sleeve.
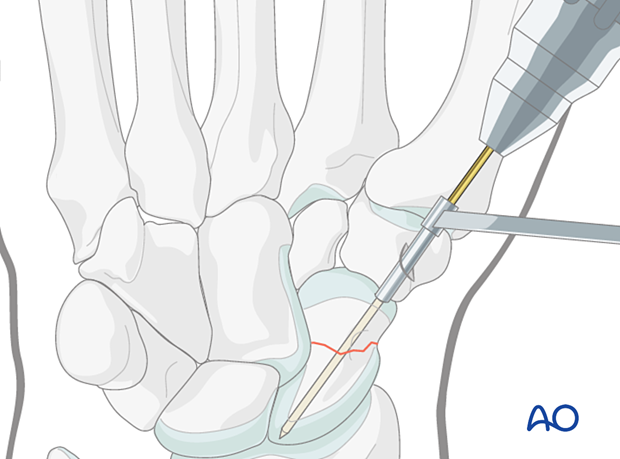
The guide wire track should be approximately angled 45° dorsally and 45° ulnarly along the mid-axis of the scaphoid.
Do not penetrate beyond the proximal cortex of the scaphoid.
The position of the wire should be as perpendicular as possible to the fracture line. In oblique fractures, this principle may have to be compromised.
Occasionally, access to a distal entry point for a device can only be gained by a limited excavation of the edge of the trapezium or through it.
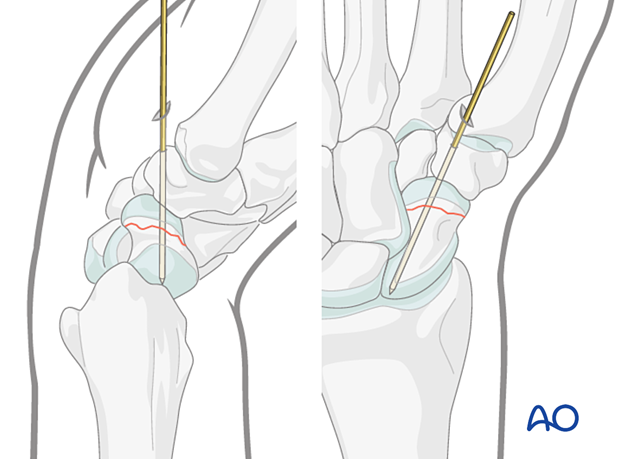
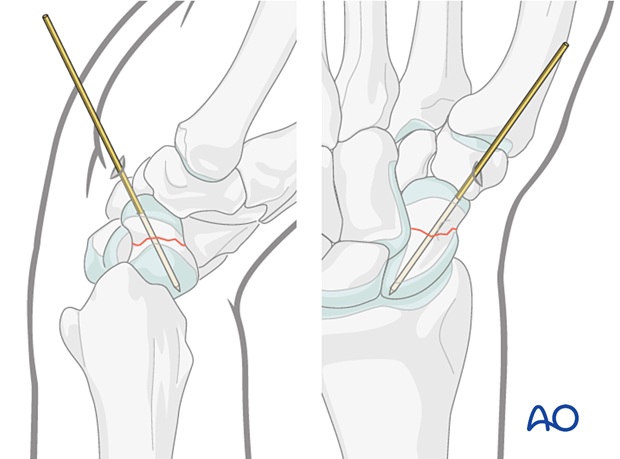
The case shows AP and lateral views of a guide wire in a transverse scaphoid waist fracture.
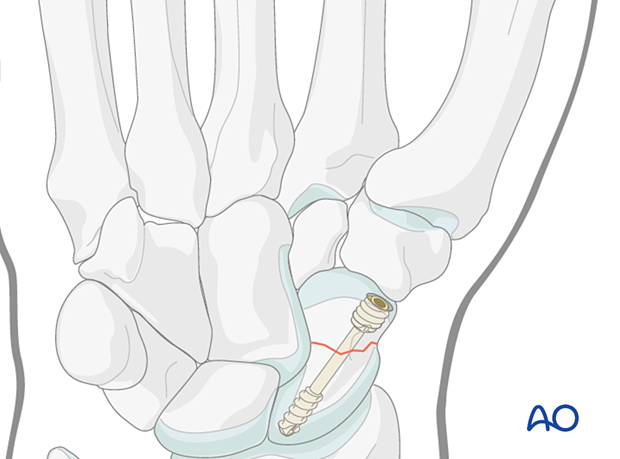
5. Screw insertion
Insert the headless compression screw in a standard manner.
Select a screw 2–4 mm shorter than the measured length with the appropriate thread length.
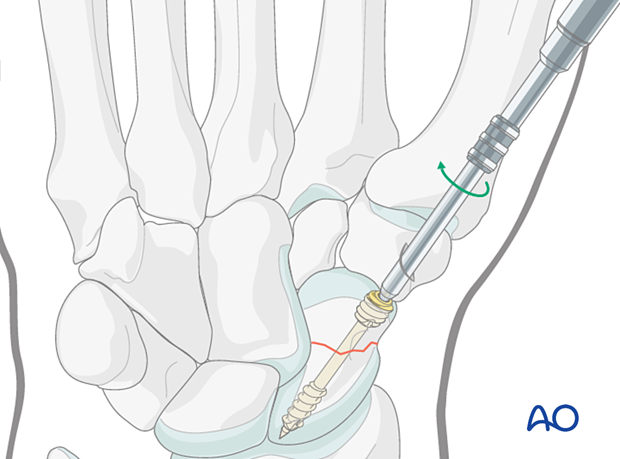
Check the final position of the screw and the scaphoid stability with an image intensifier.
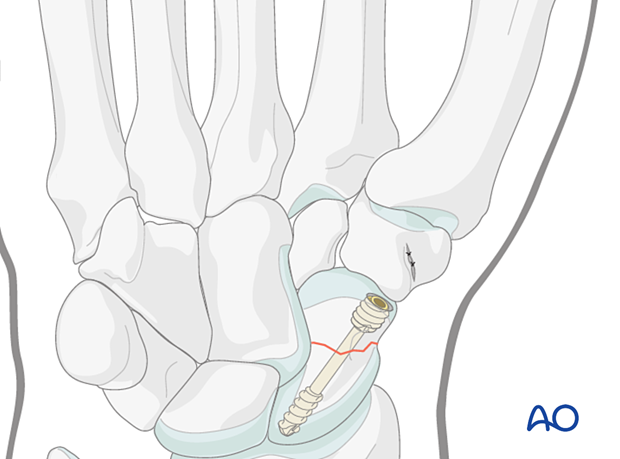
Case of screw fixation of a transverse scaphoid waist fracture

6. Aftercare
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.
Pain control
To facilitate rehabilitation, it is important to control the postoperative pain adequately.
- Management of swelling
- Appropriate splintage
- Appropriate oral analgesia
- Careful consideration of peripheral nerve blockade
Immediate postoperative treatment
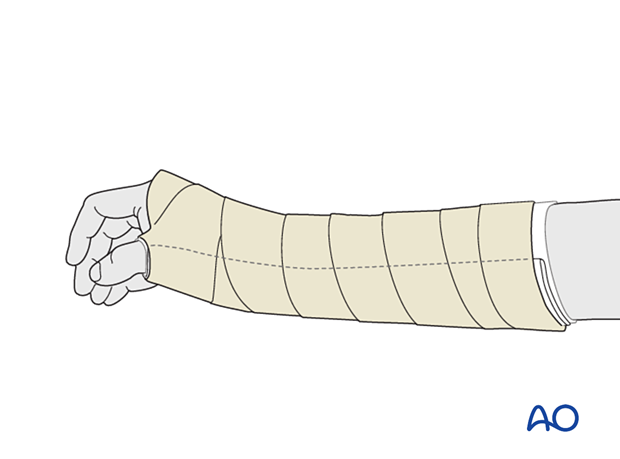
Immobilize the wrist with a well-padded below-elbow splint for 2 weeks.
Splinting helps with soft-tissue healing, especially of the ligaments cut during a palmar approach.