Postoperative treatment of carpal injuries
1. Introduction
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
2. Inflammatory phase (injury to the end of week 3 after injury)
- Principle: protection of the injured (operated) hand to facilitate uneventful healing
- Aim: healing without complications while facilitating early movement
Resting and positioning the limb
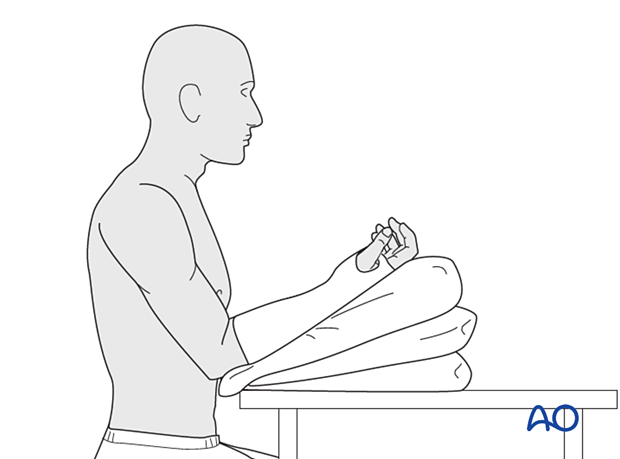
The patient is encouraged to position the arm to facilitate lymphatic and venous drainage to avoid swelling.
External splintage - Full time
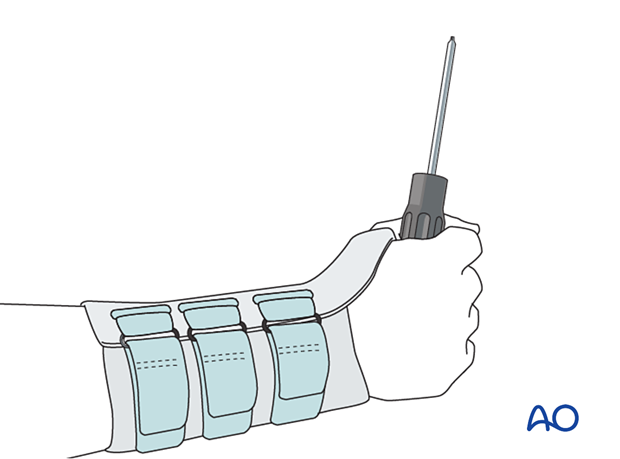
Splinting helps with soft-tissue healing, especially of skin and ligaments incised during a surgical approach. The position of the wrist and splint is determined by the specific injury and approach.
Rest the wrist with a well-padded below-elbow splint applied for up to 6 weeks. A double-layered bandage may be sufficient for simple reconstruction procedures. A firmer plaster or synthetic splint may be required for the support of more complex reconstructions over a longer period. Splintage should not be applied in a complete circumferential manner: if the bandage becomes wet it may shrink and act like a tourniquet causing swelling in the distal part of the limb, and even a compartment syndrome.
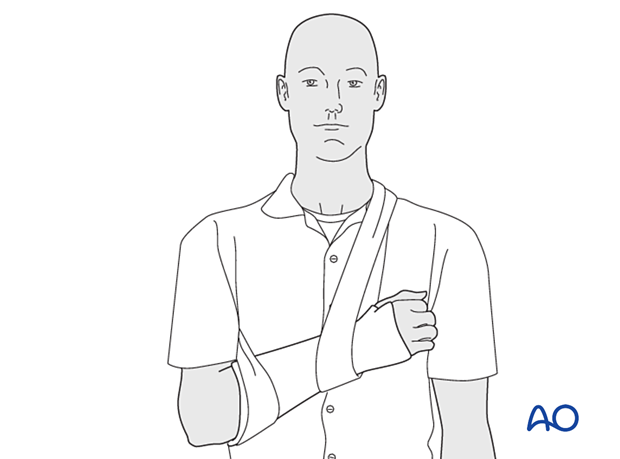
A sling should be used to support the hand and forearm when the patient is mobile. Ideally, the hand should be held higher than the elbow to avoid edema caused by dependency.
Functional exercises
These are intended to avoid edema in inactive soft tissues leading to interstitial fibrosis, adhesions, and contractures.
The patient should be encouraged to touch the skin of the affected hand (and fingers) and to use the hand (and fingers) to touch surfaces and objects as comfort permits. This encourages the restoration, retention, and maintenance of cutaneous and articular sensibility and may contribute to avoiding adverse events such as complex regional pain syndrome.
Specific exercises are determined by the injury pattern and treatment undertaken. Patient education and monitoring are ideally undertaken by a hand therapist.
Exercises should not provoke pain. Self-directed exercises are encouraged: frequent sets of low-amplitude, high-repetition movements are safer and more easily performed than infrequent sets of high-amplitude movements.
Resting between sets of exercises must be in a posture which avoids dependent swelling.
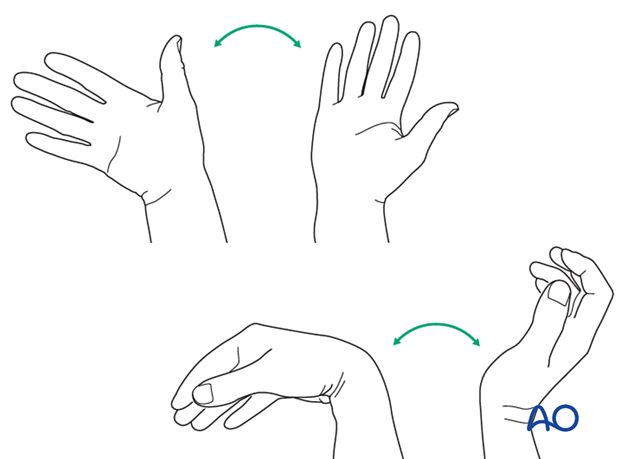
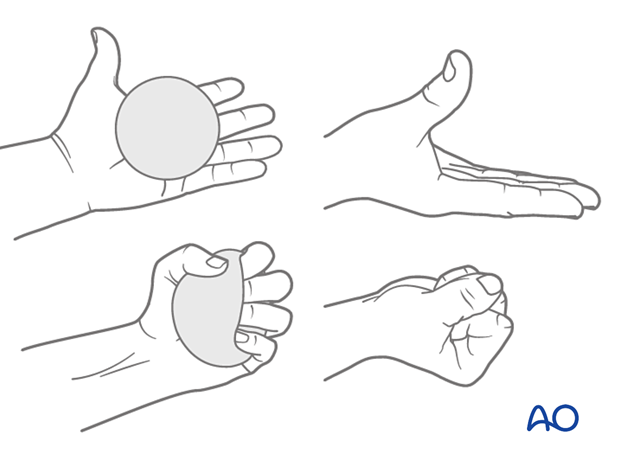
This illustration shows an exercise to mobilize the interossei muscles.
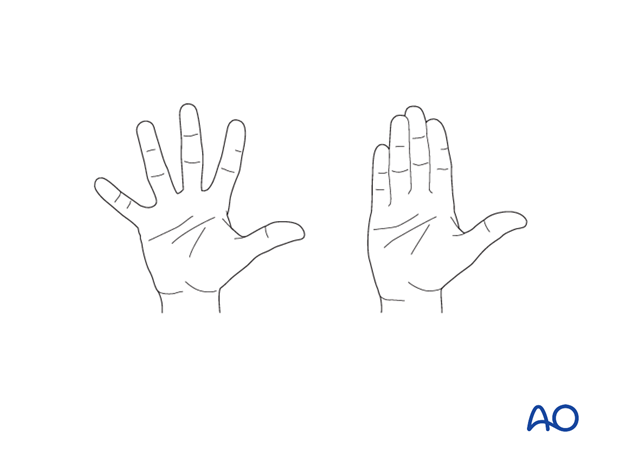
This illustration shows an exercise to mobilize the lumbrical muscles and superficial and deep flexor tendons.
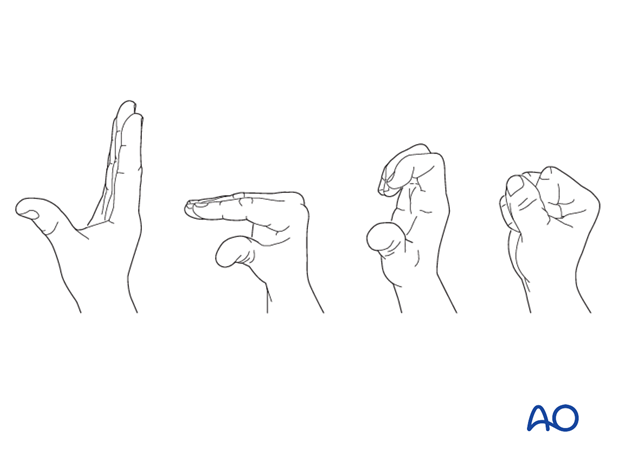
This illustration shows exercises to mobilize the carpal rows.
3. Early repair phase (beginning of week 4 to end of week 6 after injury)
- Principle: continued protection of the injured (operated) hand with the promotion of directed tissue repair
- Aim: established healing of injured tissues with isometric strength
Resting and positioning the limb
The same principles apply as in the first phase.
External splintage - Full-time progressing to part-time or no support
As soft-tissue healing progresses and swelling subsides, splintage can be removed for greater periods of time during which functional activities can be performed.
Functional exercises
Resistance exercises can be introduced in addition to the exercises of the first phase.
4. Late repair and early tissue remodeling phase (beginning of week 7 to end of week 12 after injury)
- Principle: reestablishment of proprioception in the hand
- Aim: encourage normal tissue structure and reinnervation through daily activities without secondary injury
Resting and positioning the limb
The limb can be rested without elevation. But long periods of dependent positioning should be avoided as swelling can still occur.
External splintage - Progressing to no support
The need for external splintage is dictated by functional demands. Temporary or removable splintage may be used to protect the healing limb or joint.
Functional exercises
Functional exercises are dictated by the specific injury or operation. The aim is to introduce activities relevant to the patient’s occupation or functional needs.
5. Remodeling and reintegration phase (beginning of week 13 after injury)
- Principle: normalization of the proprioceptive function with optimal biomechanics
- Aim: to establish normal tissue structure and reinnervation through training and practice for optimal endurance
Resting and positioning the limb
Recurring swelling should not occur in this stage and the need to rest or position the limb is no longer required.
External splintage - During ‘at risk’ activities
Functional bracing may still be indicated to protect the healed limb from overload in situation where instability can be provoked.
Functional exercises
Normal occupational and personal activities should be resumed.













