ORIF through dorsal approach - Antegrade screw fixation
1. General considerations
Introduction
For the fixation of proximal pole fractures of the scaphoid, headless compression screws may be used in an antegrade fashion through a dorsal approach.
Choice of implant
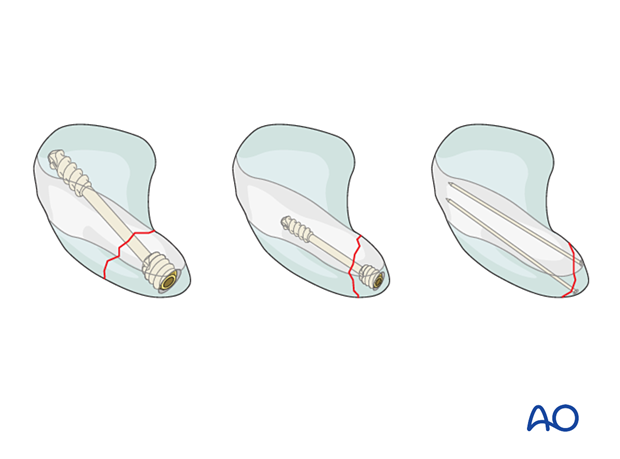
If the proximal pole fragment is larger than 5 mm, a cannulated, headless, self-compressing screw (2.4 or 3.0 mm) is the implant of choice.
For smaller proximal pole fragments, the use of a mini headless bone screw is advisable.
K-wires may be a better option for fixation of very small fragments (flakes).
Scapholunate ligament reattachment
If a bony avulsion fracture of the scapholunate ligament from the scaphoid is present, fixing the fragment, either with K-wires, or a small screw (1.5 mm), is necessary.
Comminuted scaphoid fractures
In case of a wedge fracture or comminution, a temporary K-wire may help to maintain the anatomy during screw insertion.
It is recommended to remove this K-wire after fracture compression.
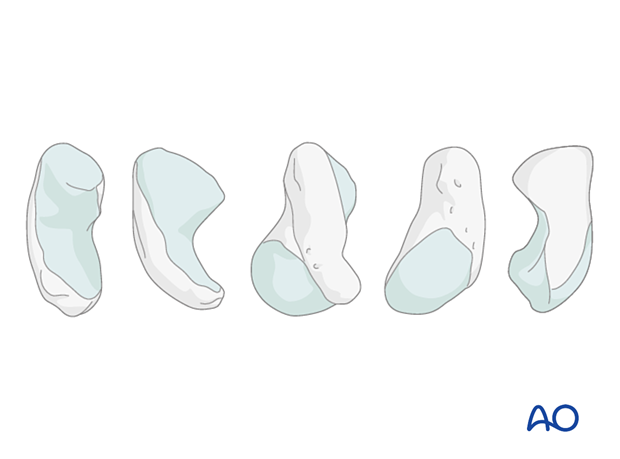
Anatomical considerations
80% of the surface of the scaphoid is covered with articular cartilage. This greatly limits potential points of entry for fixation devices.
An additional constraint is the curved shape of the scaphoid.
This means that a wire or fixation device along the true central axis of the scaphoid is not possible from a palmar approach. Occasionally, access to a distal entry point for a device can only be gained by a limited excavation of the edge of the trapezium.
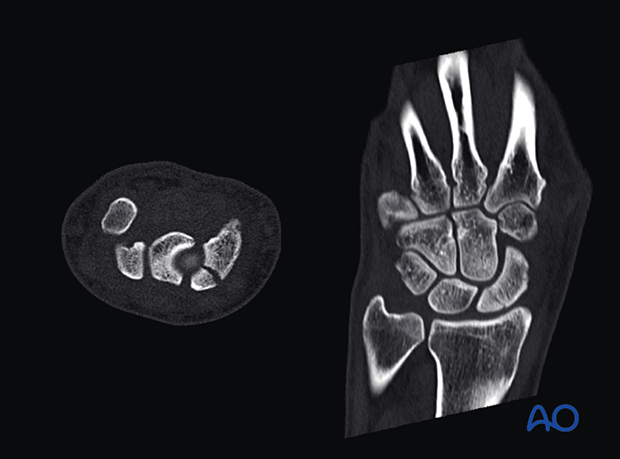
Preoperative planning
Conventional radiographs do not always adequately demonstrate the proximal pole fracture configuration.

A CT scan is recommended to reveal the degree of displacement.
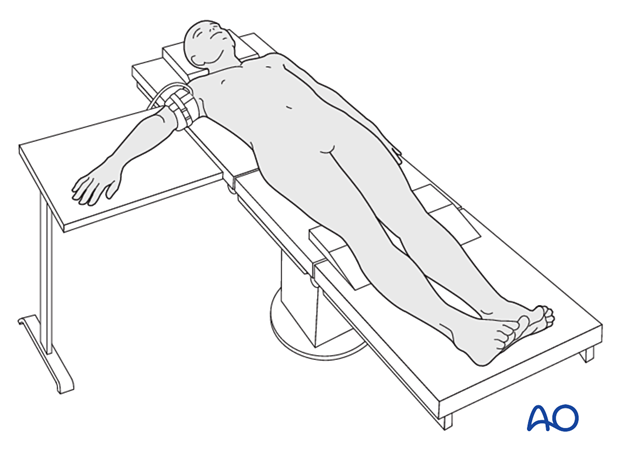
2. Patient preparation
The patient is usually supine with the arm on a radiolucent side table.
3. Approach
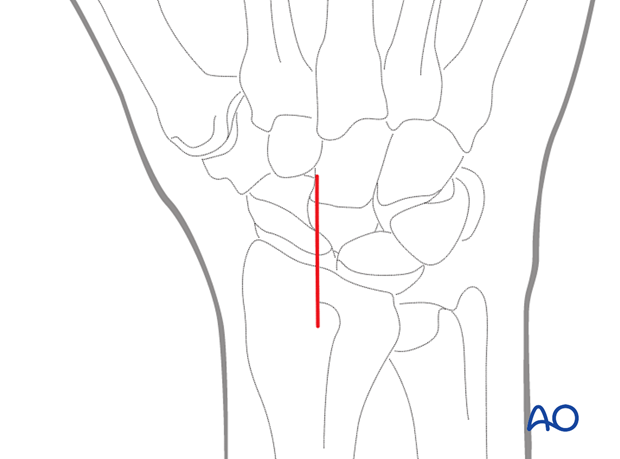
Dorsal approach
Perform a straight dorsal skin incision, starting over Lister’s tubercle, and extending distally for about 3–4 cm.
4. Reduction
Inspection of the fracture
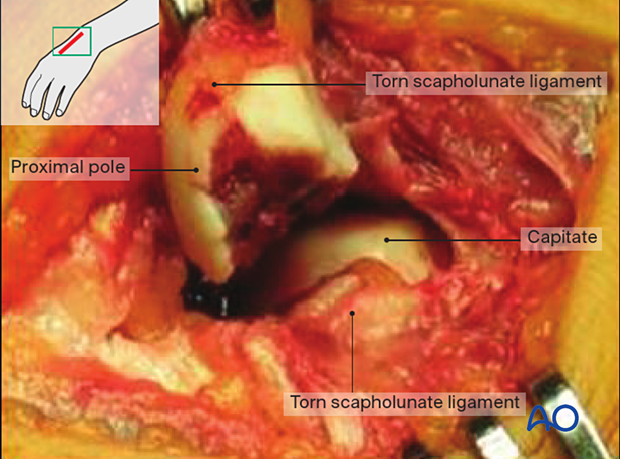
Look for additional lesions, especially scapholunate ligament ruptures.
The picture shows a proximal pole fracture combined with a complete scapholunate rupture. The head of the capitate is visible deeper in the wound. The proximal pole fragment has been delivered into the wound and has no soft-tissue attachments to the remaining carpus. Its vitality is therefore in question.
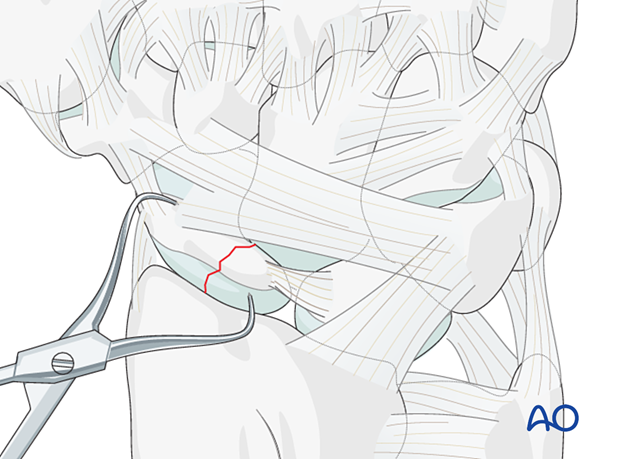
Reduction
If the fracture is displaced, reduce it with small pointed reduction forceps.
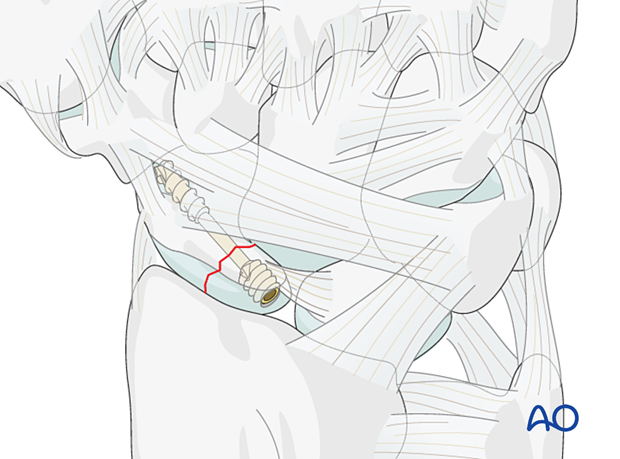
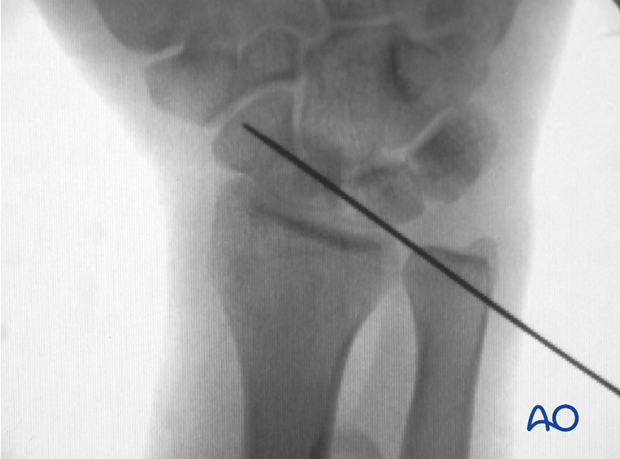
5. Guide-wire insertion
The entry point is at the proximal pole, directly adjacent to the scapholunate ligament insertion.
Insert the guide wire in the axis of the shaft of the first metacarpal, in radial abduction.
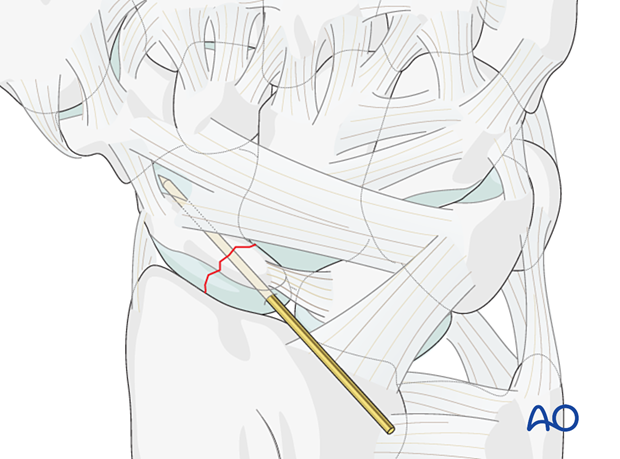
Confirm accurate advancement of the guide wire in the scaphoid axis with an image intensifier in at least two planes and perpendicular to the fracture plane.
Do not penetrate the scaphotrapezial joint with the guide wire.
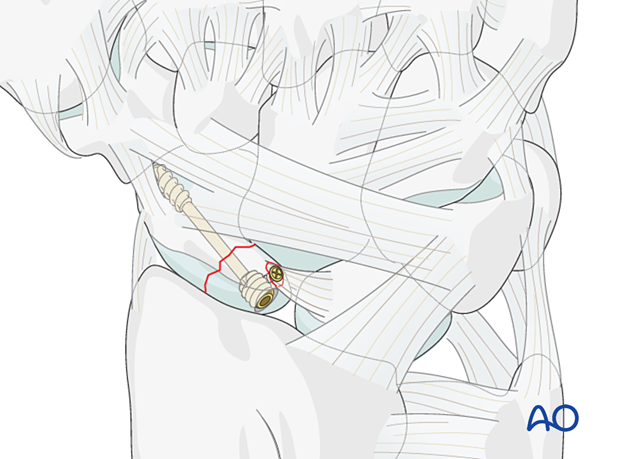
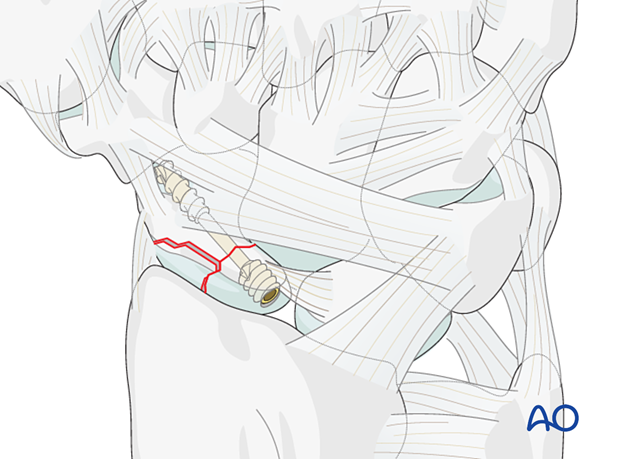
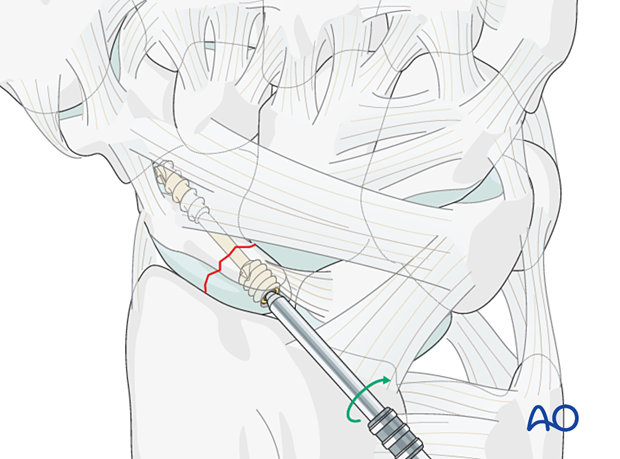
6. Screw insertion
Insert the headless compression screw in a standard manner.
Select a screw 2–4 mm shorter than the measured length with the appropriate thread length. In most cases, a 16–20 mm cannulated screw is the appropriate length.
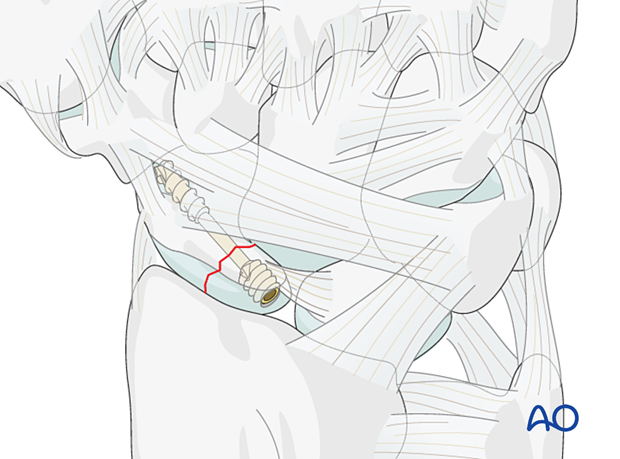
Confirming screw position
Check the final position of the screw and the scaphoid stability with an image intensifier.
7. Aftercare
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.
Pain control
To facilitate rehabilitation, it is important to control the postoperative pain adequately.
- Management of swelling
- Appropriate splintage
- Appropriate oral analgesia
- Careful consideration of peripheral nerve blockade
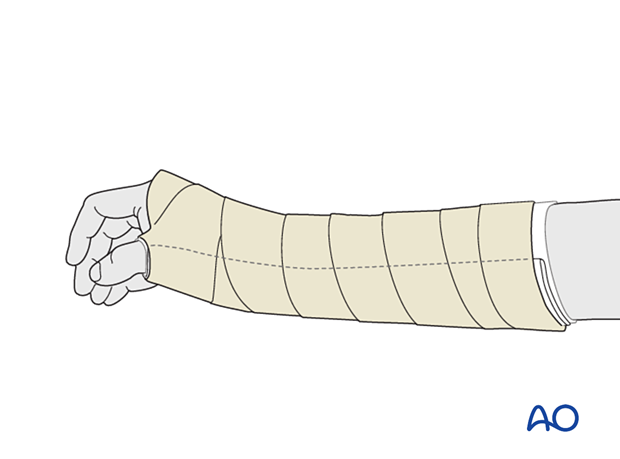
Immediate postoperative treatment
Immobilize the wrist with a well-padded below-elbow splint for 2 weeks.
Splinting helps with soft-tissue healing, especially of the ligaments cut during a palmar approach.