ORIF through Kocher-Langenbeck
1. General considerations
Sequence of the treatment
Pre-operative traction will be advantageous if the hip is subluxed medially.
For ORIF of transverse fractures with Kocher-Langenbeck approach, the following surgical sequence is common:
- Joint distraction and removal of incarcerated fragments
- Reduction of femoral head dislocation if not achieved closed on admission
- Reduction
- Assessment of reduction (particularly of the anterior column indirect reduction)
- Fixation of the anterior column
- Fixation of the posterior column
Planning/templating
Preoperative templating is essential for understanding the complexity of an acetabular fracture.
When using implants on the innominate bone, it is important to know the best starting points for obtaining optimal screw anchorage (see General stabilization principles and screw directions).
Patient positioning
The Kocher-Langenbeck approach can be performed in either the prone or lateral position.
If a hip dislocation is expected, the patient should be positioned in the lateral position. However, lateral positioning enhances the inward displacement of the ischiopubic segment due to the weight of the femoral head. Therefore, prone position is preferred and greatly facilitates the reduction of the ischiopubic segment.
The maintenance of knee flexion (at 90°) and hip extension throughout the procedure reduces tension on the sciatic nerve.
Extending the approach
In cases with large superior wall fragments, further visualization of the superior acetabulum may be necessary. This is achieved with a trochanter osteotomy extension.
Indirect visualization
Unusually for a significant joint, articular reduction of acetabular fractures is indirect. The articular surface of the hip joint is not seen directly. Reduction must be assessed by the appearance of the extraarticular fracture lines and intraoperative fluoroscopic assessment. Some fracture lines are palpated manually but not seen directly such as transverse fracture lines on the quadrilateral plate.
Quality of reduction
Posttraumatic arthrosis is directly related to the quality of reduction - the better the reduction, the greater the chance of a good or excellent result.
Teaching video
AO teaching video: Use of the distractor on the pelvis
2. Reduction
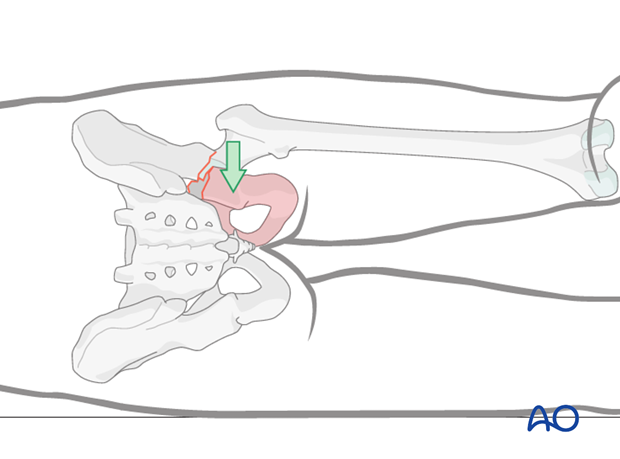
Femoral head subluxation
If the femoral head has been reduced in a closed fashion, subluxation of the joint to clear bony fragments would be required.
If the head is still dislocated then the joint can be cleaned before reduction.
Joint distraction
Apply longitudinal and/or lateral traction to reduce the femoral head under the superolateral fragment. This will also begin the reduction of the displaced ischiopubic fragment by ligamentotaxis.
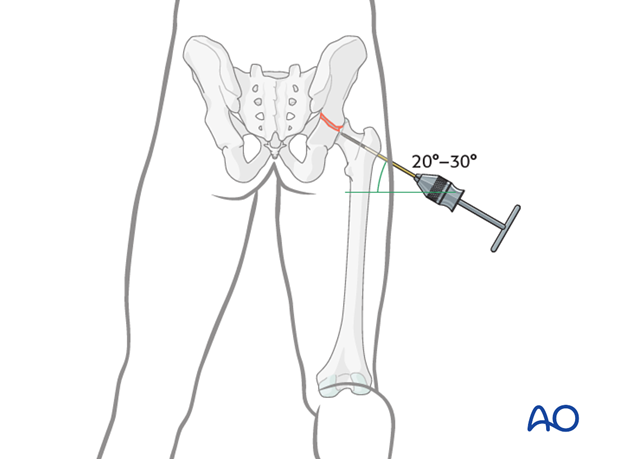
Traction may be applied laterally with a greater trochanteric Schanz screw, maintained with manual force or traction apparatus attached to the operating room table.
Alternatively, longitudinal traction applied through a distal femoral traction pin may allow sufficient joint distraction to reduce the femoral head under the superolateral fragment.
In some surgeon’s experience, the use of a traction table post or other traction frame is helpful during this operation.
The appropriately positioned femoral head can be used as a template for reduction of the distal ischiopubic fragment.
Fracture reduction
Begin the reduction by cleaning all clot and bone fragments from the fracture plane. The posterior column fracture along the retroacetabular surface is easily accessed directly.
The anterior column involvement requires palpation of the fracture along the quadrilateral surface as it crosses from the pelvic brim. The surgeon will develop the space through the sciatic notch and with their finger, or a curved instrument, clear the obturator internus muscle and all debris from the fracture line on the internal surface.
It is important to see the fracture well both inside and outside the joint. In pure transverse fractures, without a posterior wall component, the capsule may be completely intact, limiting visualization of the intraarticular surface. In these cases, the hip joint should be opened with a capsulotomy, just distal to the labrum. Additional traction on the femur makes it easier to see into the joint.
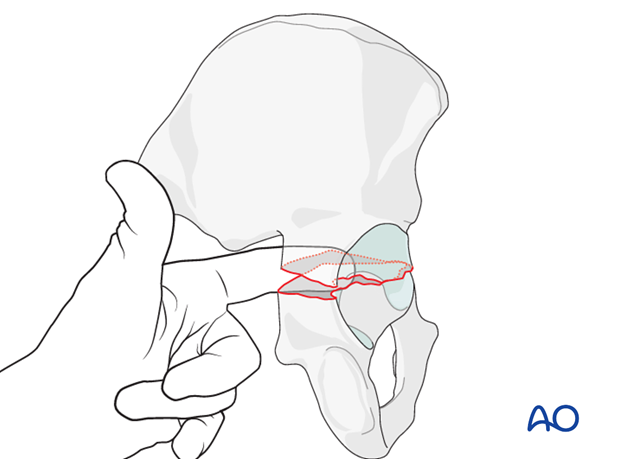
Reduction of a transverse fracture requires two main steps: lateralization, and derotation of the ischiopubic fragment. It is important that the reduction is correct across the entire fracture, as the posterior surface may appear to be reduced satisfactorily while anteriorly rotation or displacement persists.
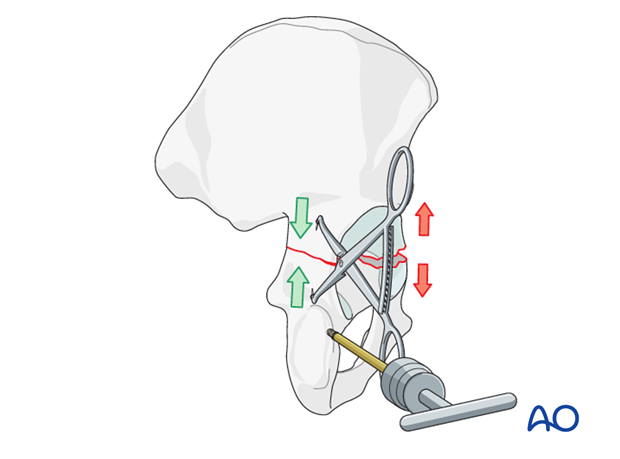
Manipulation of the ischiopubic fragment requires several instruments, but is typically begun with a Schanz screw in the ischium to be used as a joystick. This will be used to lateralize and derotate the ischiopubic fragment.
The reduction of the cranial aspect of the fracture, as it crossed the posterior border of the bone, will be fine-tuned utilizing a variety of tools.

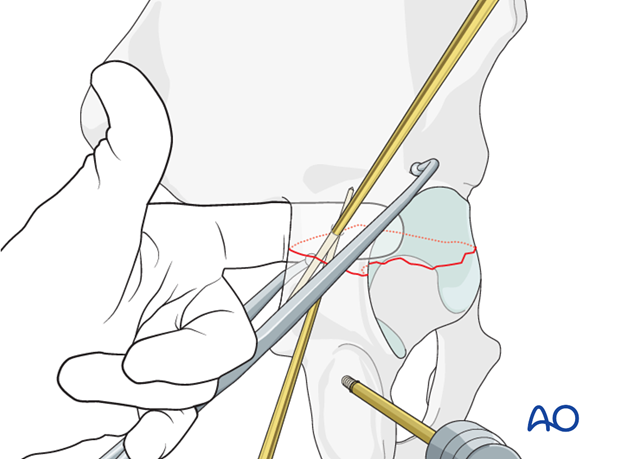
A hook inserted through the greater sciatic notch can help to manipulate the cranial aspect of the ischiopubic fragment by pulling it laterally.
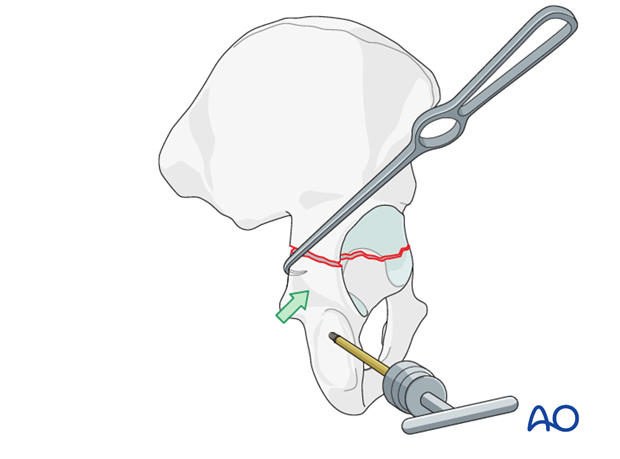
Use of reduction forceps
Appropriately chosen and placed forceps can aid reduction and provisional stabilization of the ischiopubic segment.
The pointed reduction forceps (or Weber clamp) is a very powerful reduction tool. It may be necessary to drill a small hole for application of the clamp points to prevent slipping on the convexity of the retroacetabular surface.
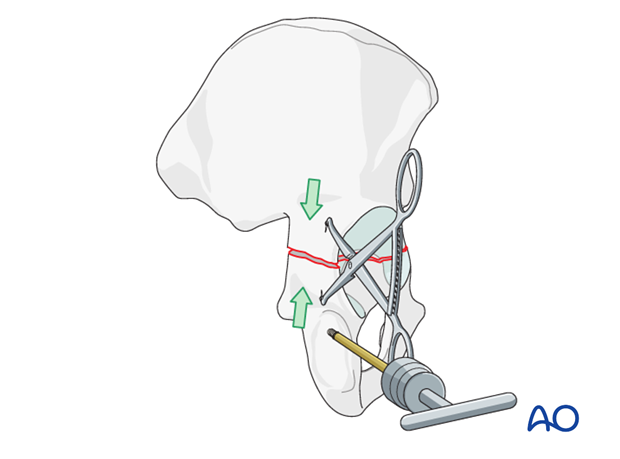
One must be careful not to over compress the posterior cortex and distract the anterior elements of the ischiopubic segments.
An asymmetric (A), angled quadrangular (B), or collinear clamp (not shown) can be inserted carefully through the greater notch.
The internal point is applied to the anterior quadrilateral surface of the displaced ischiopubic segment, or on the posterior border of the bone. The external point is applied to the intact iliac fragment cranial and lateral to the fracture along the retroacetabular surface.
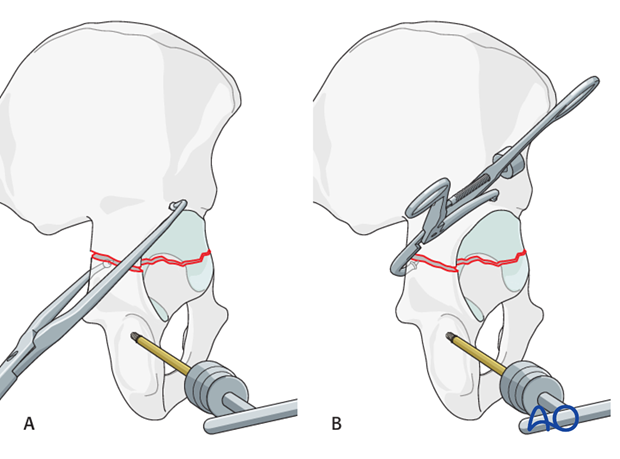
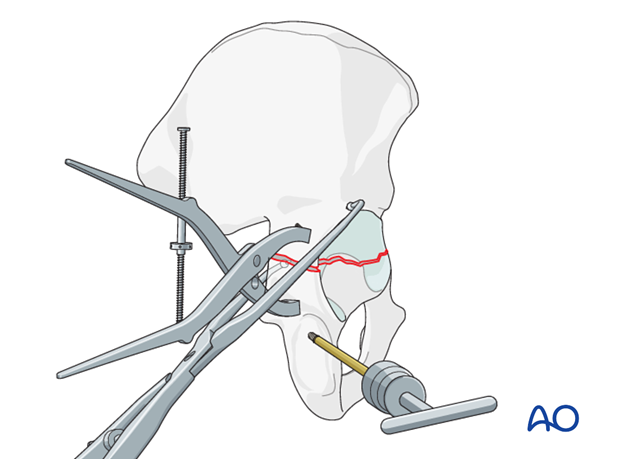
Another reduction option is to use the Jungbluth clamp, which is attached to the bone with two screws. One is on the iliac fragment and the other on the posterior column of the displaced ischiopubic fragment.
Choose the anchor screws for the clamp in such a way that interference with the preliminary or definitive fixation is avoided. Also these screws need to be carefully positioned to avoid intraarticular penetration.
This is a very powerful clamp for both reduction and the application of compression to the fracture. However, if the screws are not placed correctly, this clamp may allow overcompression of the posterior column and distraction of the anterior aspect of the fracture.
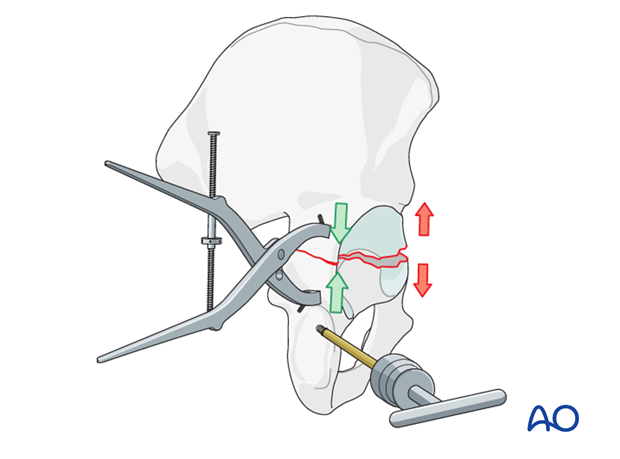
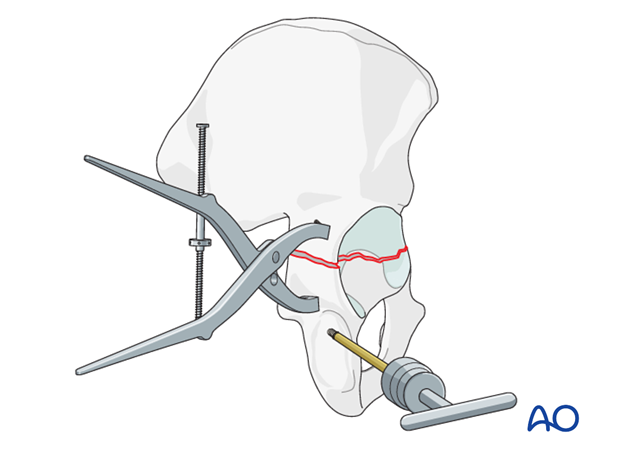
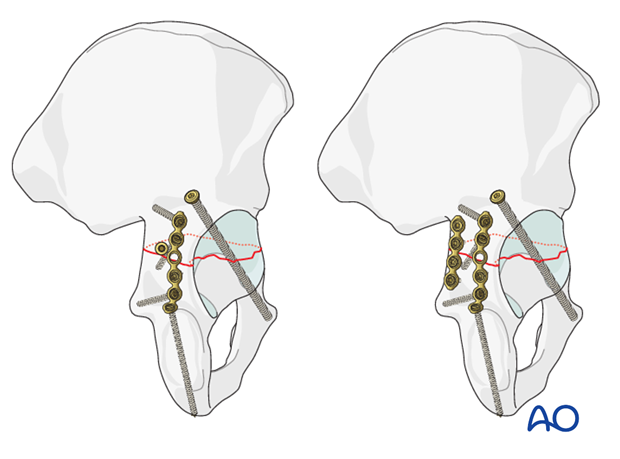
Dual clamps
Commonly, a single clamp does not achieve an anatomic reduction. Addition of a second clamp is often required.
In our illustration, the first clamp is a Jungbluth clamp on the posterior column. The second clamp is a large asymmetric clamp, with the internal point applied through the sciatic notch, resting on the quadrilateral surface. The external point is placed anteriorly on the proximal fragment. This clamp corrects displacement of the anterior part of the transverse fracture.
In all cases the Schanz screw in the ischial tuberosity is used as a joystick for the ischiopubic segment.
3. Assessment of reduction
Every part of the fracture must be anatomically reduced.
Inspect the fracture inside the joint through the capsulotomy performed for intraarticular visualization. Additional traction may aid visualization of the articular reduction.
Direct visualization of the retroacetabular surface reduction indicates the quality of reduction of the posterior aspect of the ischiopubic segment.
Preliminary fixation (with K-wires, provisional plates or temporary screws) may allow for the removal of one or more clamps and give access to the sciatic notch for palpation of the internal pelvis.
Assess the reduction of the anterior column by palpation of the quadrilateral surface to the pelvic brim through the sciatic notch. This is critical as the anterior reduction cannot be directly visualized through the KL approach. However, with multiple clamps maintaining the reduction, intrapelvic palpation may not be possible.
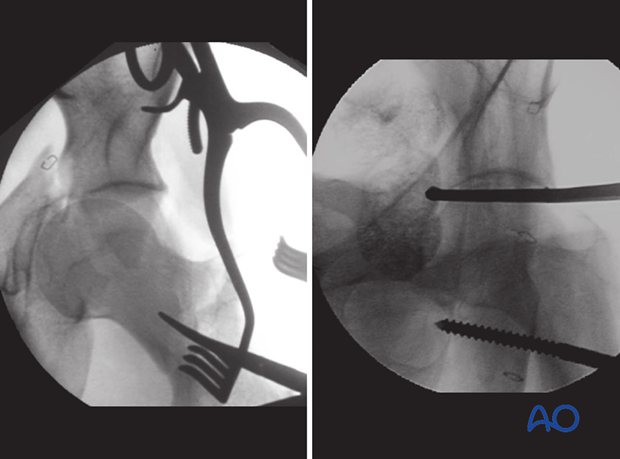
Reduction must also be assessed with fluoroscopy. The obturator oblique is particularly important as the anterior column reduction is not visualized through the Kocher-Langenbeck approach.
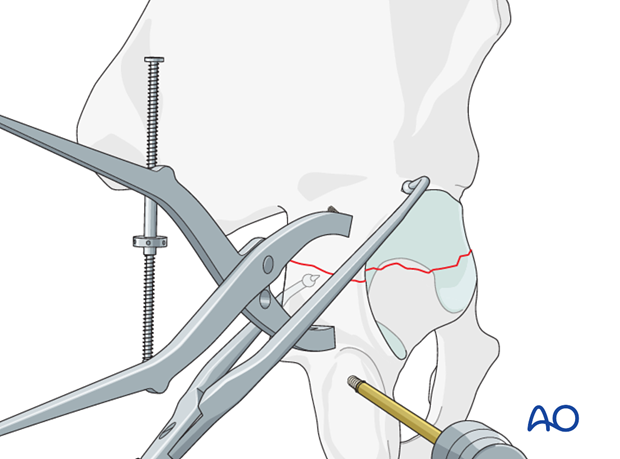
4. Fixation of the anterior column
After obtaining anatomical reduction of the fracture, definitive fixation begins with the anterior column.
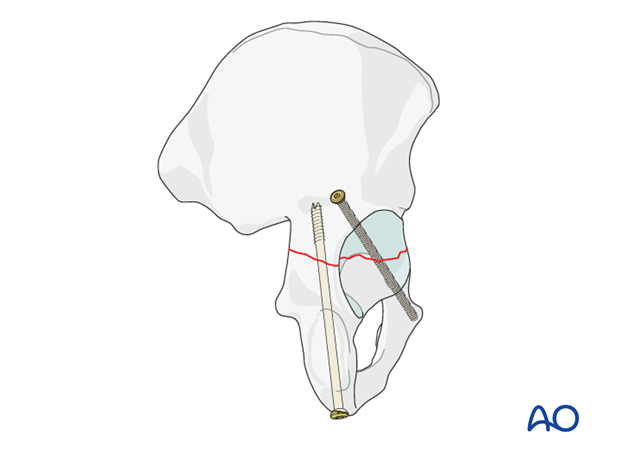
The anterior column screw
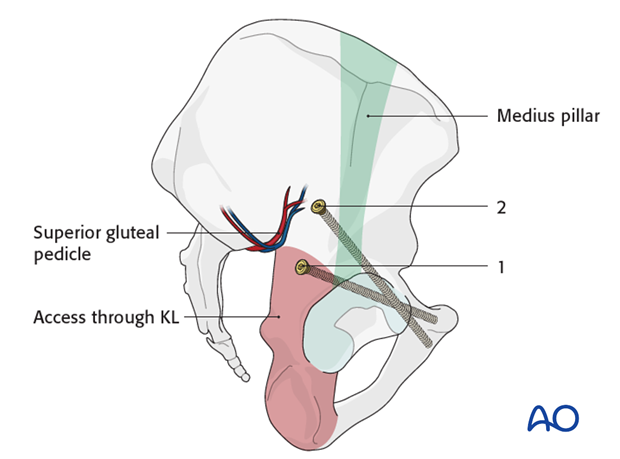
The anterior screw is placed obliquely from above the greater sciatic notch across the fracture. It is aimed anteriorly towards the root of the superior pubic ramus.
The starting point for the anterior column screw applied through the Kocher-Langenbeck exposure (1) is different than that applied through the extended iliofemoral (2). The exposure offered by the Kocher-Langenbeck approach is limited cranially and anteriorly by the superior gluteal neurovascular pedicle. Therefore, the anterior column screw entry point is placed percutaneously, or must be modified for the exposure.
The entry corridor for the screw applied through the Kocher-Langenbeck approach is generally 1-2 cm anterior (lateral) to the apex of the sciatic notch.
3.5, 4.5 or 6.5 mm screws can be used. In difficult cases, particularly obese patients, cannulated screws may be beneficial. It is often preferred to have two 3.5 mm screws instead of larger fragment fixation to provide additional torsional stability to the anterior portion of the ischiopubic segment.
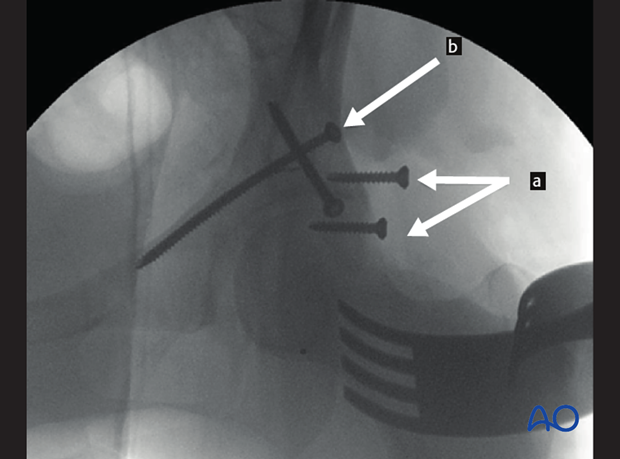
Fluoroscopy is utilized to ensure the trajectory of the screw as well as extraarticular insertion. Utilizing the obturator oblique image, the anterior column is visualized, and this image can be used to safely navigate the screw placement. In this image, the anchor screws for the Jungbluth clamp are seen (a). The clamp has been removed to avoid obscuring the anterior column. The anterior column screw has been placed across the fracture line (b).
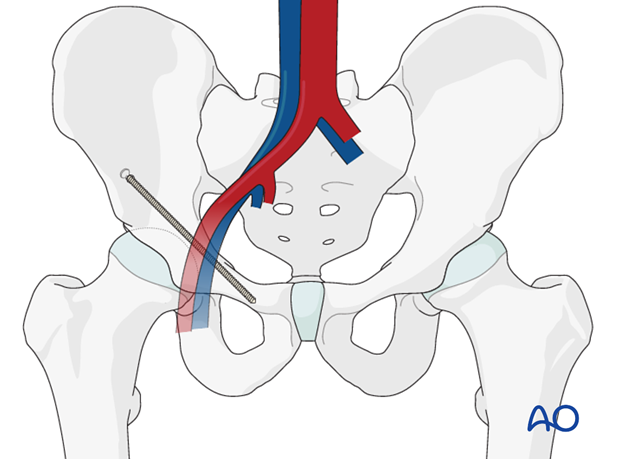
Pitfall: Risks to vessels
The external iliac vessels cross the pelvic brim anteriorly and may be injured with mal-positioned screws or imprecise drilling.
5. Fixation of the posterior column
Often two distinct points of fixation of the posterior aspect of the ischiopubic segment are required for absolute stability. Ideally, fixation is obtained medially, at the sciatic buttress to compress the posterior aspect of the transverse fracture. Additionally, a reconstruction plate will be added to augment stability.
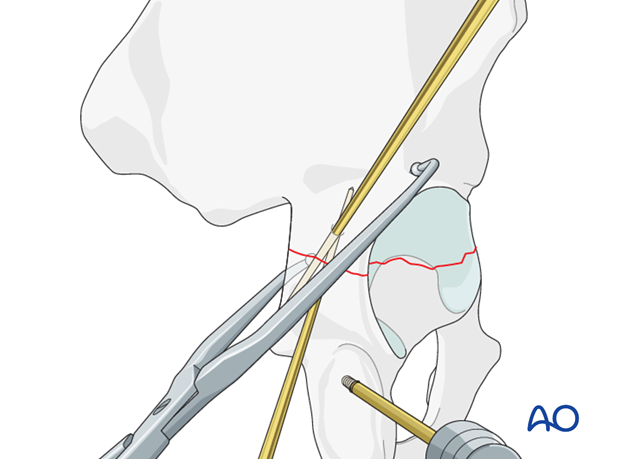
Posterior column screw
Depending upon the posterior location and orientation of the fracture, it may be suitable for posterior column screw fixation. Such a screw may be placed from distal to proximal, as illustrated. Care must be taken to avoid excessive traction on the sciatic nerve when placing the screw. Alternatively, it may be placed percutaneously through the gluteal flap.
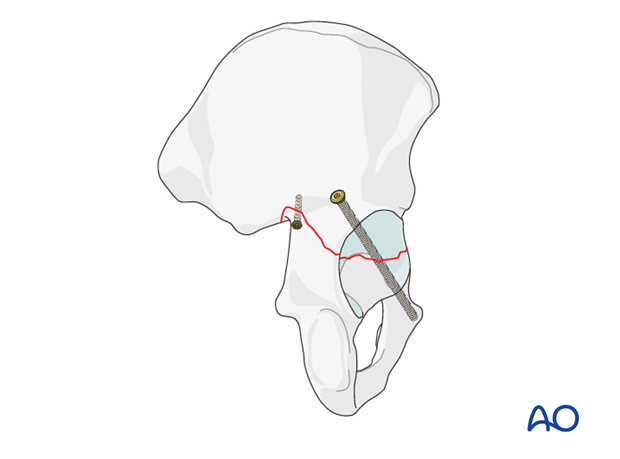
An axial posterior column screw provides interfragmentary compression across the posterior part of the fracture. This is inserted from distal to proximal.
A 7.3 mm partially threaded cannulated screw is inserted through a separate stab incision in the buttock crease over a guide wire.
The start point is at the ischial tuberosity, and a finger in the greater sciatic notch is used to guide the wire and screw up the posterior column, exiting at the pelvic brim.
Care is taken to protect the sciatic nerve at the level of the ischial tuberosity.
The use of a screw aids the placement of the posterior wall plate as it increases the freedom of placement of the wall plate.
This is commonly referred to as the “butt screw”.
If posterior column screw fixation cannot be achieved, a small or mini fragment plate may be applied along the sciatic notch to control the posterior aspect of the transverse fracture.
This plate needs to be positioned carefully so as not to obstruct placement of the definitive reconstruction plate.
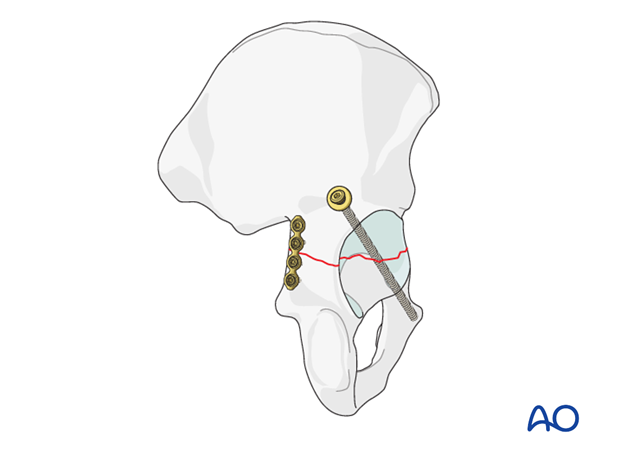
Posterior column plate
Generally, screw fixation alone is insufficient for torsional control of the ischiopubic segment. A reconstruction plate applied to the retroacetabular surface is commonly the mainstay of posterior column fixation.
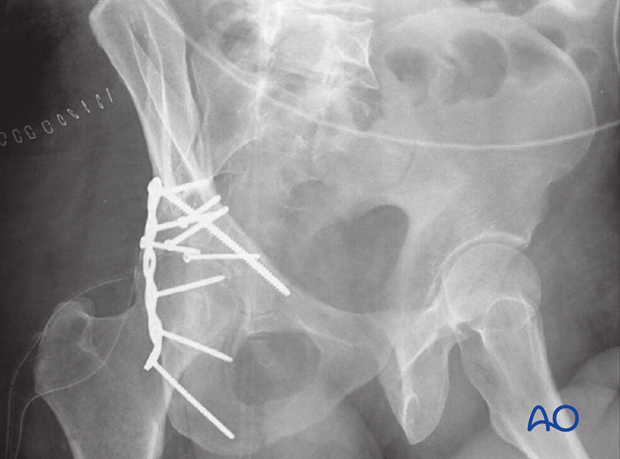
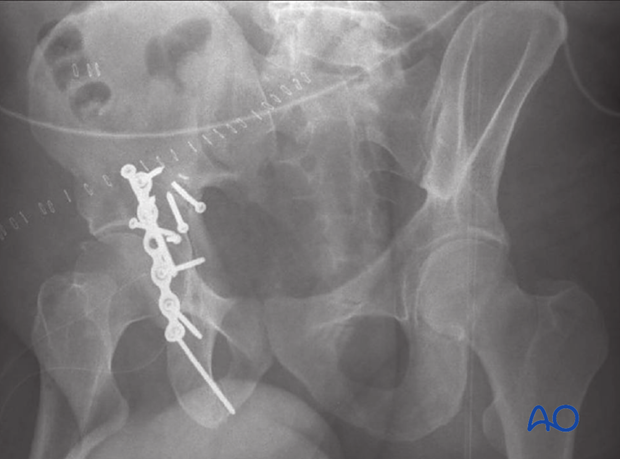
6. Final radiographic assessment
After completion of fixation, 3 views (AP, obturator oblique, iliac oblique view) are obtained to confirm anatomical reduction and fixation.
The AP radiograph demonstrates an anatomic reduction and restoration of the iliopectineal and ilioischial lines, the anterior rim, the posterior rim, and the radiological roof.
In this case, a 4.5 mm anterior column screw has been placed. Two interfragmentary posterior column lag screws have been placed (distal to proximal) near the sciatic notch. Two additional interfragmentary screws have been placed more distally on the retroacetabular surface. A six-hole reconstructive plate has been contoured to the retroacetabular surface.
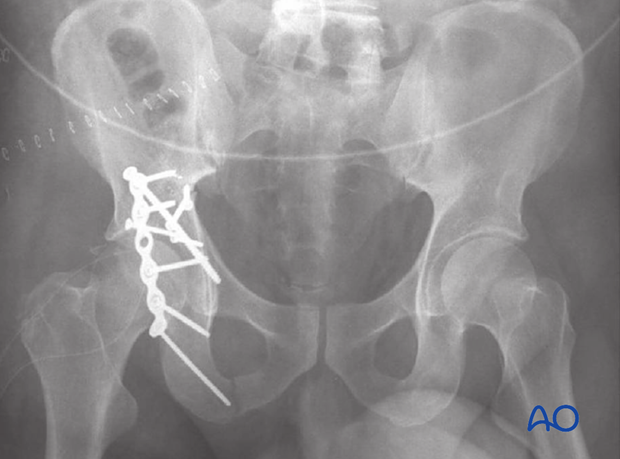
The obturator oblique demonstrates that the anterior column reduction is anatomic and that the anterior column screw does not violate the extraarticular surface.
The iliac oblique demonstrates that the posterior column reduction is anatomic. The distal to cranial interfragmentary lag screws can be seen at the apex of the fracture.
Postoperatively, obtain formal high-quality radiographs of AP and both oblique views.
7. Postoperative care
During the first 24-48 hours, antibiotics are administered intravenously, according to hospital prophylaxis protocol. In order to avoid heterotopic ossification in high-risk patients, the use of indomethacin or single low dose radiation should be considered. Every patient needs DVT treatment. There is no universal protocol, but 6 weeks of anticoagulation is a common strategy.
Wound drains are rarely used. Local protocols should be followed if used, aiming to remove the drain as soon as possible and balancing output with infection risk.
Specialized therapy input is essential.
Follow up
X-rays are taken for immediate postoperative control, and at 8 weeks prior to full weight bearing.
Postoperative CT scans are used routinely in some units, and only obtained if there are concerns regarding the quality of reduction or intraarticular hardware in others.
With satisfactory healing, sutures are removed around 10-14 days after surgery.
Mobilization
Early mobilization should be stressed and patients encouraged to sit up within the first 24-48 hours following surgery.
Mobilization touch weight bearing for 8 weeks is advised.
Weight bearing
The patient should remain on crutches touch weight bearing (up to 20 kg) for 8 weeks. This is preferable to complete non-weight bearing because forces across the hip joint are higher when the leg is held off the floor. Weight bearing can be progressively increased to full weight after 8 weeks.
With osteoporotic bone or comminuted fractures, delay until 12 weeks may be considered.
Implant removal
Generally, implants are left in situ indefinitely. For acute infections with stable fixation, implants should usually be retained until the fracture is healed. Typically, by then a treated acute infection has become quiescent. Should it recur, hardware removal may help prevent further recurrences. Remember that a recurrent infection may involve the hip joint, which must be assessed in such patients with arthrocentesis. For patients with a history of wound infection who become candidates for total hip replacement, a two-stage reconstruction may be appropriate.
Sciatic nerve palsy
Posterior hip dislocation associated with posterior wall, posterior column, transverse, and T-shaped fractures can be associated with sciatic nerve palsy. At the time of surgical exploration, it is very rare to find a completely disrupted nerve and there are no treatment options beyond fracture reduction, hip stabilization and hemostasis. Neurologic recovery may take up to 2 years. Peroneal division involvement is more common than tibial. Sensory recovery precedes motor recovery and it is not unusual to see clinical improvement in the setting of grossly abnormal electrodiagnostic findings.













