ORIF, 3-point fixation (without orbital reconstruction)
1. Principles
General considerations
Correct anatomical reduction is required to reproduce the original structure of the zygomaticomaxillary complex and the proper alignment of the orbital walls. In order to achieve proper reduction of the lateral orbital wall the greater wing of the sphenoid and the zygoma must be properly aligned.
3-point fixation ensures accurate 3-D repositioning of the fractured zygoma. Resulting orbital floor defects must also be addressed.
The aim is to restore the proper orbital volume and to restore proper width, AP projection, and height of the midface. Proper reduction of the zygoma addresses the issues of AP projection of the width of the midface.
It is possible that the periorbital contents may have been affected by the reduction of the zygomatic-complex fracture. Forced duction tests should be performed before and after reduction of the zygoma to make sure that the patient does not have entrapment of the soft tissues. Pre- and postoperative ophthalmologic exams should be considered in all patients who have sustained periorbital trauma.
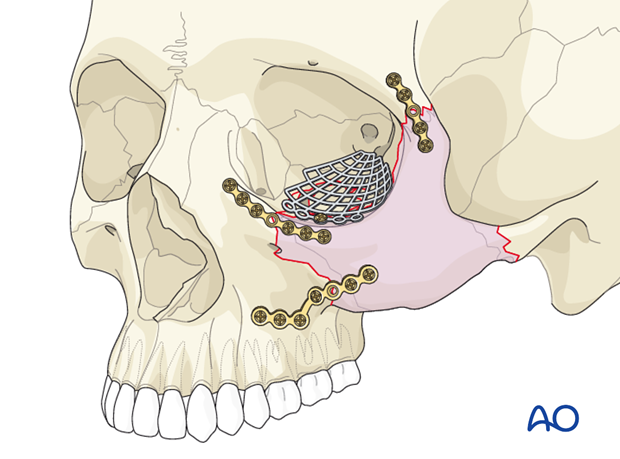
Plate fixation
As a general principle with all plate fixation, at least two screws should be placed on both sides of the fracture. This often requires a plate with at least one extra screw hole to span the fracture. Ideally, the first screw should be placed on the side of the mobile fragment, and the plate used as a handle to close the gap and reduce the bone.
The first two screws should be placed in the plate holes closest to the fracture, one on each side of the fracture. Make sure that the fracture is adequately spanned so that each screw is placed in solid bone.
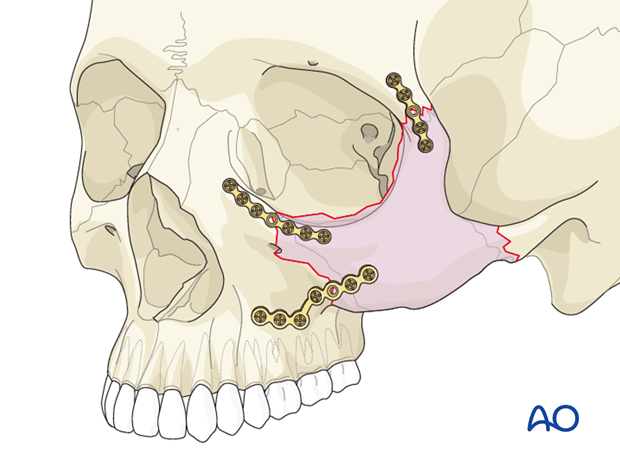
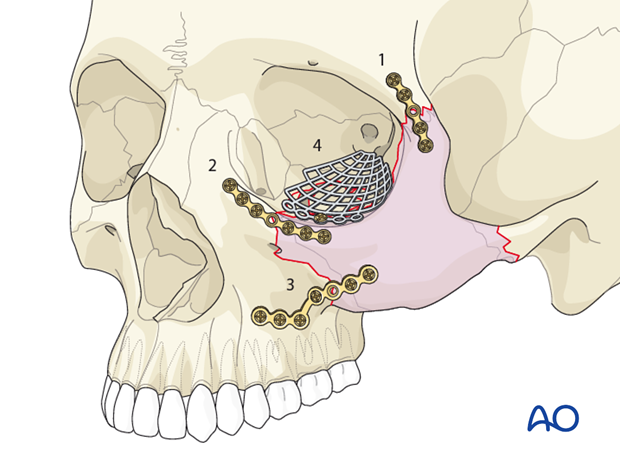
Order of reduction and fixation
In a zygomatic fracture that requires orbital floor reconstruction, after exposing the zygoma and orbital floor, the zygoma should be disimpacted prior to dissecting herniated orbital soft tissues from the maxillary sinus.
In a fracture of this nature, the reduction and fixation of the zygoma should be performed first. Reconstruction of the orbital floor should be performed after the zygoma has been reduced and stabilized.
It is debated whether the second site for fixation should be the orbital rim or the zygomaticomaxillary buttress.
Note: Check the proper alignment of the repositioned zygomatic complex along the lateral wall of the orbit (sphenozygomatic junction) before performing the fixation at the other points.
It is easier to visualize whether a proper reduction of the lateral orbital wall is achieved by placing the plate on the infraorbital rim as the second plate after the zygomaticofrontal suture plate. A smaller plate is recommended for the infraorbital rim. A larger plate (commonly an L-shaped plate) is recommended for the zygomaticomaxillary buttress.
When the lateral wall is comminuted, the lateral wall is not so reliable as a landmark in determining the proper reduction of the zygoma. In this situation the surgeon has to place higher emphasis in the reduction of other sites. Reconstruction of the lateral wall of the orbit with mesh, even when comminuted, is not necessary due to the bone support of the temporalis muscle.
It should be noted that using this 3-point fixation technique we have chosen not to plate the zygomatic arch. It is difficult to plate the zygomatic arch without performing a coronal or preauricular exposure. Perfect reduction of the zygoma through three approaches will generally result in a good alignment of the zygomatic arch. Click here for a description of the 4-point fixation.
Many surgeons argue that potential cosmetic defects caused by a coronal approach to the zygomatic arch are worse than the defect of a minimally displaced arch. These cosmetic defects include alopecia from the coronal scar, risk of injury to the temporal branch of the facial nerve, and temporal hollowing.
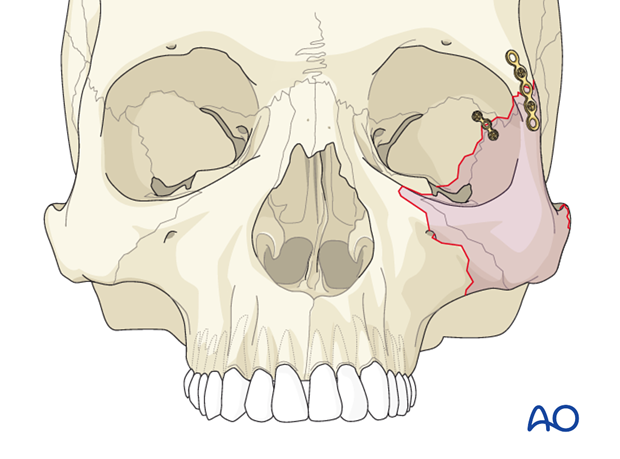
Involvement of lateral orbital wall
Isolated lateral orbital wall fractures are rare and only occur after isolated trauma to this anatomical structure. Much more common is a lateral orbital wall fracture together with a zygoma fracture (as shown).
Displacement of the lateral orbital wall (with or without combined zygomatic complex fracture) directly affects the intraorbital volume (ie, inwards displacement results in exophthalmos whereas outward displacement results in enophthalmos). However, such globe displacements are camouflaged by posttraumatic swelling so that the above mentioned sequelae often become apparent only after swelling has decreased, which normally takes about 2 weeks.
Click here for detailed description of clinical and radiographic examination.
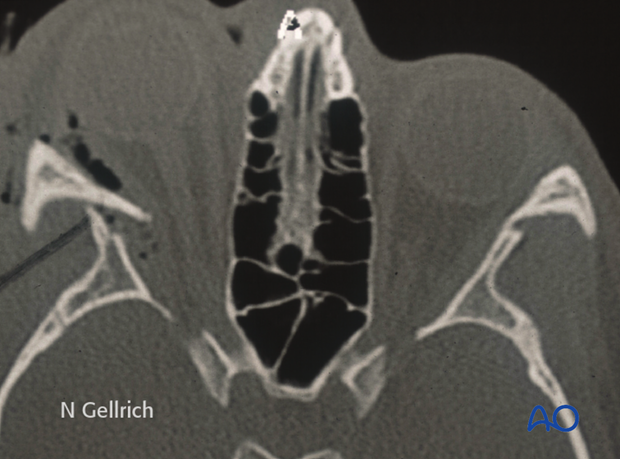
Clinical examination of the lateral orbital wall area is camouflaged by the overlying soft tissues. However, this CT scan nicely shows contour differences at the lateral orbital wall area.
Severely inward displaced lateral orbital wall fractures might require emergency treatment, if intraorbital pressure (due to displacement and/or intraorbital hematoma) is compromising optic nerve function (see axial CT scan).
Lateral orbital wall plate
Some surgeons recommend placement of a plate to reduce and fixate the lateral wall of the orbit between the greater wing of the sphenoid and the zygoma. This helps to guarantee a proper reduction of this fracture. It can only be used if there is no comminution of the lateral wall of the orbit. Placement of this plate is difficult because of necessary globe retraction. If a surgeon decides to position a plate in this location there is limited room, and often only one screw can be placed on each side of the fracture. If this plate is to be used, the authors recommend placing this as the second plate after the plate on the zygomaticofrontal suture.
This plate can be placed through the upper eyelid incision or if the fracture is not as posterior as in this illustration through the inferior eyelid incision.
Teaching video
AO Teaching video on fixation of a zygomaticomaxillary fracture and an orbital floor fracture
2. Selection of approach
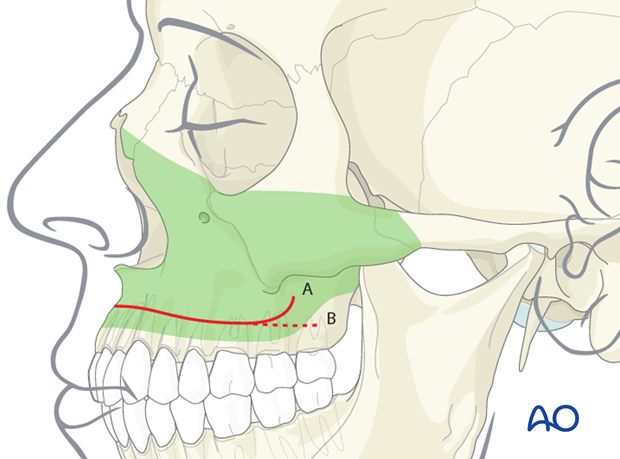
Three approaches are required for this procedure. They commonly include a intraoral maxillary vestibular approach, a lower-eyelid incision ( transcutaneous or transconjunctival), and a coronal incision with direct exposure of the zygomatic arch and lateral orbital region. Existing lacerations may also be used.
The intraoral maxillary vestibular approach facilitates the exposure of the lateral buttress of the midface. It can also be used to expose the inferior orbital rim. The lateral maxillary vestibular approach can also be used to help reposition the depressed zygoma.
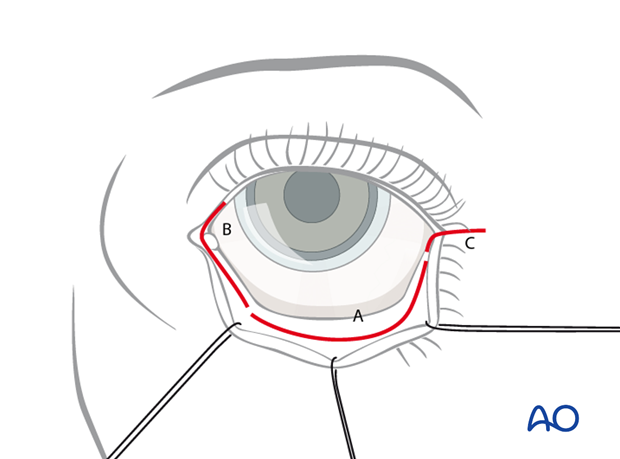
The lower-eyelid incision is ideal for exposing the orbital floor, the orbital rim, and the lateral orbital wall.
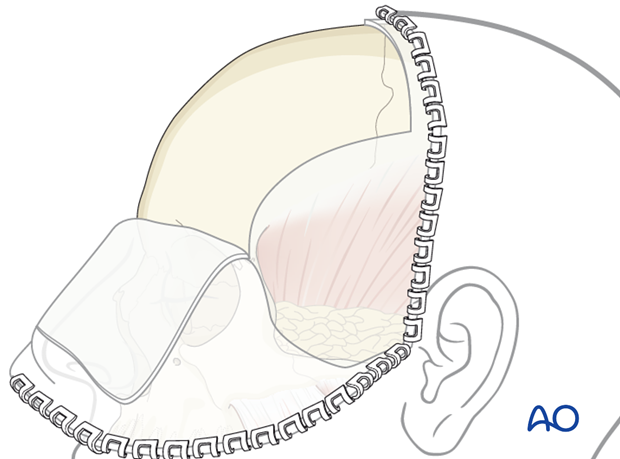
The coronal incision is ideal for exposure of the zygomatic arch, lateral orbital rim (frontozygomatic suture), lateral wall of the orbit (sphenozygomatic suture), and can also be used to harvest split calvarial bone graft.
3. Zygoma reduction methods
The first step is to obtain proper 3-D reduction of the zygoma using an elevator, hook, screw, or Carroll-Girard type device to mobilize the zygoma into its proper position.
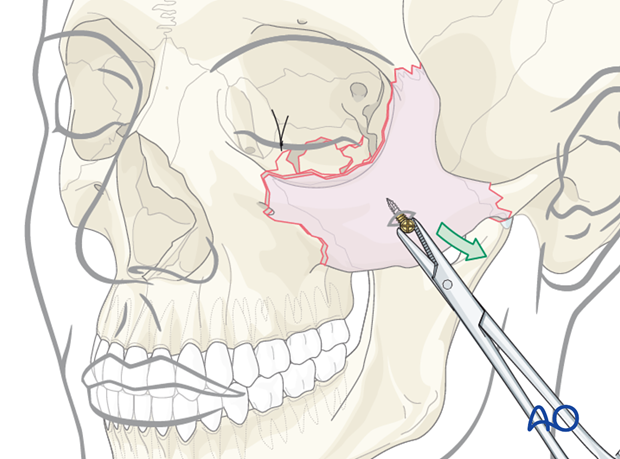
Illustration shows reduction being performed via a transoral (Keen) approach placed through the maxillary vestibular incision using an elevator …
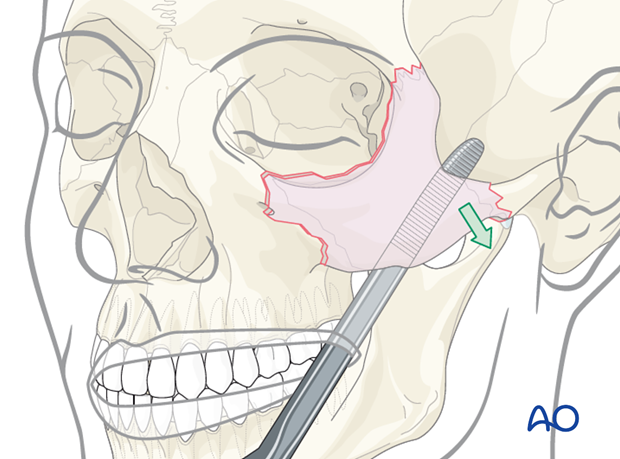
… or using a hook.
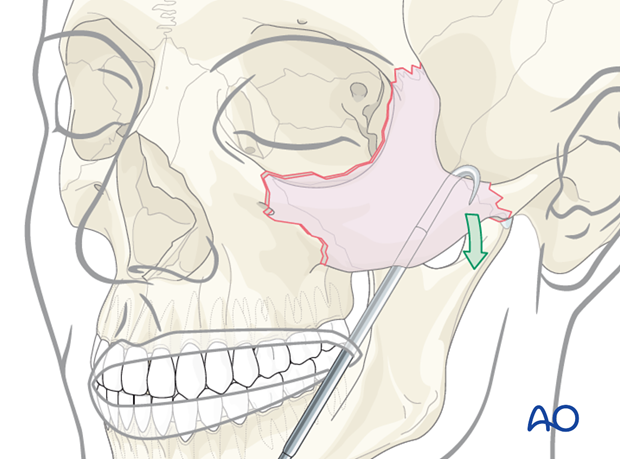
Alternative: screw and traction
A screw is inserted into the zygomatic bone through the skin. This allows fracture reduction using the screw and a holding instrument.
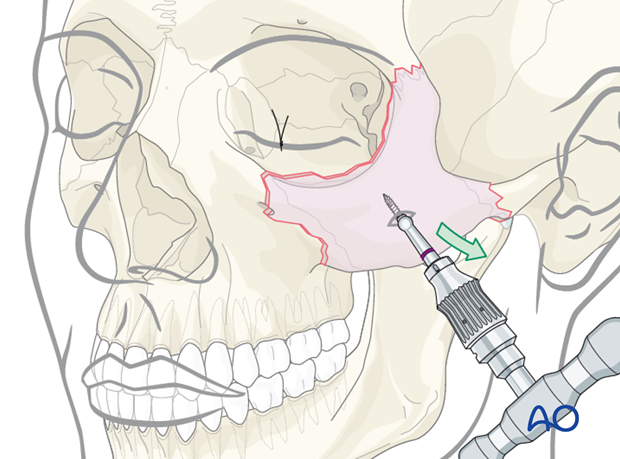
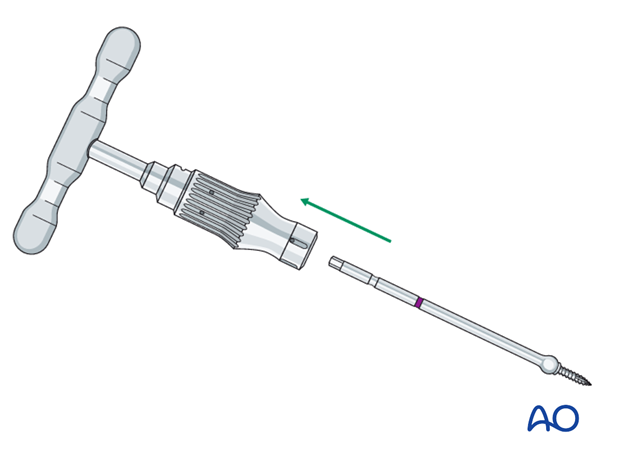
Threaded reduction tool
A threaded reduction tool (Carroll-Girard screw) is inserted into the zygoma through the lower eyelid incision or directly through the skin of the face and used for reduction.
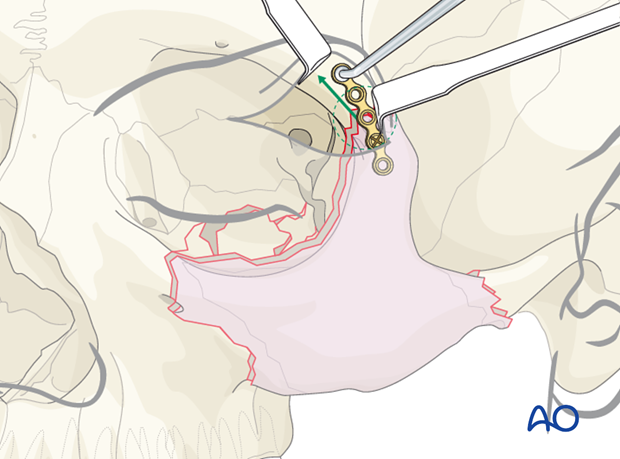
4. Placement and fixation of first plate
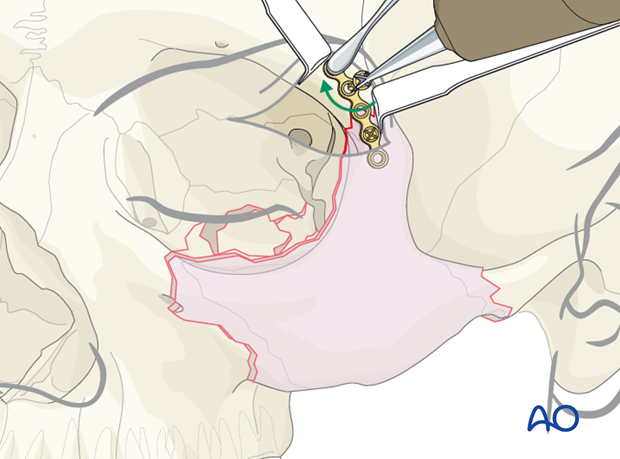
Placement of first plate
The first plate is placed across the frontozygomatic fracture area.
We recommend a minimum of a 5-hole plate with one hole spanning the fracture line. The plate should be properly adapted.
In this illustration, the first screw is placed in the unstable zygomatic fracture. An instrument is then used to pull the plate and zygomatic fragment in the cephalad direction to further reduce the fracture.
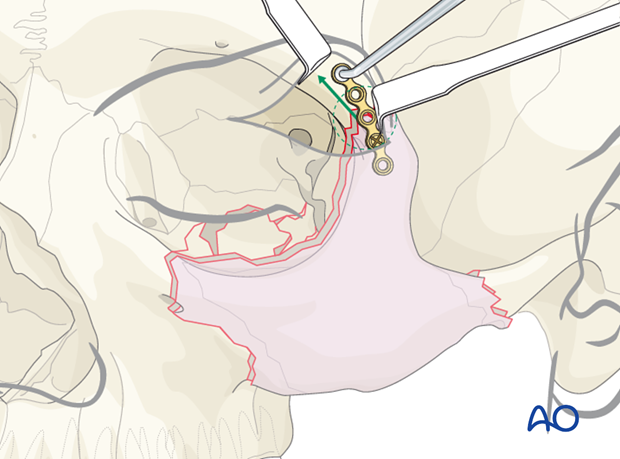
Fixation of first plate
Only one screw should be placed on each side of the fracture in the holes nearest to the fracture, until the surgeon has verified the proper 3-D reduction of the zygoma at the other two points. Looking through the upper eyelid incision, it is very difficult to determine the 3-D rotation of the zygoma.
While drilling holes in the periorbital area, it may be desirable to use a drill bit with a stop (commonly 6 mm stop).
The final two screws in the zygomaticofrontal plate should be placed at the end of the intervention.
5. Placement of additional plates
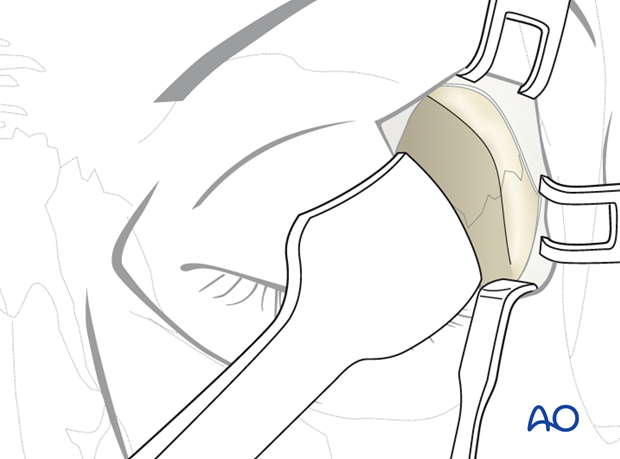
Placement of second plate
When looking through the lower eyelid incision, the orbital rim plate should be properly adapted. Use a minimum of a 5-hole plate with the extra hole spanning the fracture line. Reconfirm that the lateral orbital wall (greater wing of the sphenoid and zygoma) has been properly reduced prior to placing this plate. A minimum of two screws should be placed on each side of the fracture.
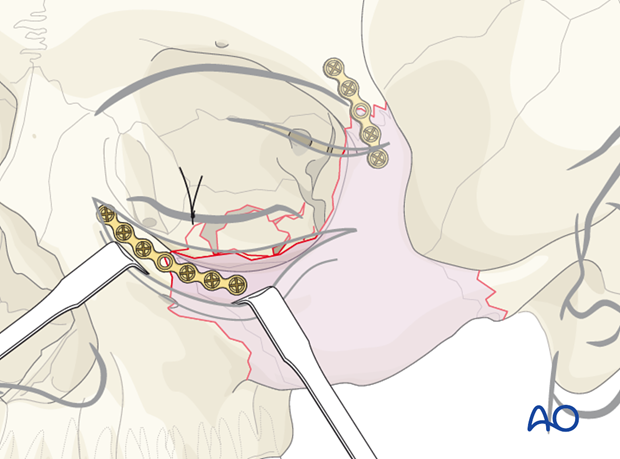
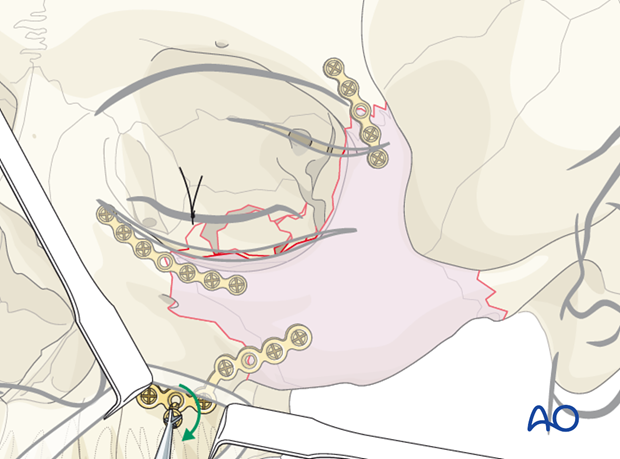
Placement of third plate
Looking through the maxillary vestibular approach, the fracture of the zygomaticomaxillary buttress is aligned. A larger L-shaped plate is ideal for the fixation of this fracture. This is the most difficult plate to properly adapt in a zygoma fracture. It is important that the leg of the L-plate be placed on the most lateral portion of the lateral maxillary buttress, where the bone is fairly thick.
It is similarly important that the foot of the L-plate is placed along the alveolar bone in a manner that the screws will not be placed into the dental roots. A common problem with this third plate is failure to properly adapt the L-plate, resulting in screw placement into the thin wall of the anterior maxillary sinus. It is not uncommon for the lateral maxillary buttress to be comminuted. In this instance using a longer L-plate with multiple screw holes may be ideal.
We recommend that lower profile plates are used at the zygomaticofrontal suture and the infraorbital rim. A stronger plate is recommended for the zygomaticomaxillary buttress.
6. Postoperative examination
Postoperative cone beam images show the position of a fan plate reconstructing the orbital floor and medial orbital wall in a coronal …
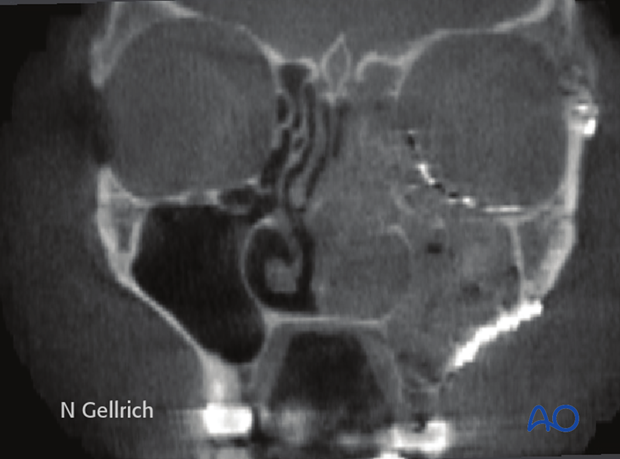
… and oblique parasagittal view in a patient with associated zygomatic-complex fracture.
Note: recontouring of the plate shown was accomplished using an intraoperative model. A standard fan plate can cover up to three walls of the orbit.

7. Aftercare
Evaluation of the patients vision is performed as soon as they are awakened from anesthesia and then at regular intervals until they are discharged from the hospital.
A swinging flashlight test may serve in the unconscious and/or noncooperative patient; alternatively electrophysiological examination has to be performed but is dependent on the appropriate equipment (VEP).
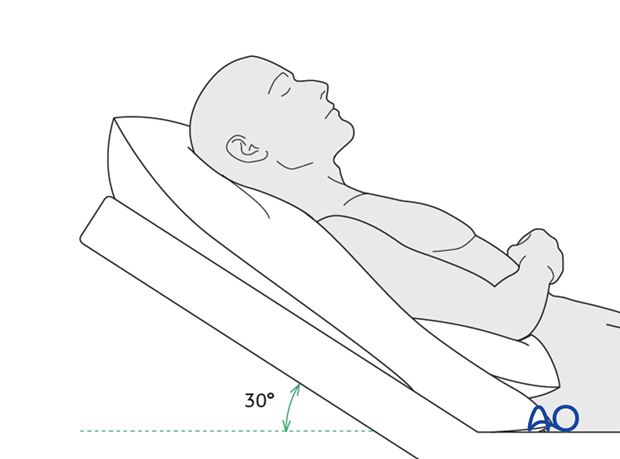
Postoperative positioning
Keeping the patient’s head in an upright position both preoperatively and postoperatively may significantly improve periorbital edema and pain.
Nose-blowing
To prevent orbital emphysema, nose-blowing should be avoided for at least 10 days following orbital fracture repair.
Medication
The use of the following perioperative medication is controversial. There is little evidence to make strong recommendations for postoperative care.
- No aspirin or nonsteroidal antiinflammatory drugs (NSAIDs) for 7 days
- Analgesia as necessary
- Antibiotics (many surgeons use perioperative antibiotics. There is no clear advantage of any one antibiotic, and the recommended duration of treatment is debatable.)
- Nasal decongestant may be helpful for symptomatic improvement in some patients.
- Steroids, in cases of severe orbital trauma, may help with postoperative edema. Some surgeons have noted increased complications with perioperative steroids.
- Ophthalmic ointment should follow local and approved protocol. This is not generally required in case of periorbital edema. Some surgeons prefer it. Some ointments have been found to cause significant conjunctival irritation.
- Regular perioral and oral wound care has to include disinfectant mouth rinse, lip care, etc.
Ophthalmological examination
Postoperative examination by an ophthalmologist may be requested. The following signs and symptoms are usually evaluated:
- Vision (except for alveolar ridge fracture, palatal fracture)
- Extraocular motion (motility) (except alveolar ridge fracture, palatal fracture)
- Diplopia (except Le Fort I, alveolar ridge fracture, palatal fracture)
- Globe position (except Le Fort I, alveolar ridge fracture, palatal fracture)
- Perimetric examination (except Le Fort I, alveolar ridge fracture, palatal fracture)
- Lid position
- If the patient complains of epiphora (tear overflow), the lacrimal duct must be checked.
Note: In case of postoperative double vision, ophthalmological assessment has to clarify the cause. Use of prism foils on existing glasses may be helpful as an early aid.
Postoperative imaging
Postoperative imaging has to be performed within the first days after surgery. 3-D imaging (CT, cone beam) is recommended to assess complex fracture reductions. An exception may be made for centers capable of intraoperative imaging.
Especially in fractures involving the alveolar area, orthopantomograms (OPG) are helpful.
Wound care
Remove sutures from skin after approximately 5 days if nonresorbable sutures have been used.
Apply ice packs (may be effective in a short term to minimize edema).
Avoid sun exposure and tanning to skin incisions for several months.
Diet
Diet depends on the fracture pattern.
Soft diet can be taken as tolerated until there has been adequate healing of the maxillary vestibular incision.
Intranasal feeding may be considered in cases with oral bone exposure and soft-tissue defects.
Patients in MMF will remain on a liquid diet until such time the MMF is released.
Clinical follow-up
Clinical follow-up depends on the complexity of the surgery, and whether the patient has any postoperative problems.
With patients having fracture patterns including periorbital trauma, issues to consider are the following:
- Globe position
- Double vision
- Other vision problems
Other issues to consider are:
- Facial deformity (incl. asymmetry)
- Sensory nerve compromise
- Problems of scar formation
Issues to consider with Le Fort fractures, palatal fractures and alveolar ridge fractures include:
- Problems of dentition and dental sensation
- Problems of occlusion
- Problems of the temporomandibular joint (TMJ), (lack of range of motion, pain)
Eye movement exercises
Following orbital fractures, eye movement exercises should be considered.
Implant removal
Implant removal is rarely required. It is possible that this may be requested by patients if the implant becomes palpable or visible. In some countries it will be more commonly requested. There have been cases where patients have complained of cold sensitivity in areas of plate placement. It is controversial whether this cold sensitivity is a result of the plate, a result of nerve injury from the original trauma, or from nerve injury due to trauma of the surgery. Issues of cold sensitivity generally improve or resolve with time without removal of the hardware.
Generally, orbital implant removal is not necessary except in the event of infection or exposure. Readmission might be indicated if long term stability of the orbital volume has not been maintained.
MMF
The duration and/or use of MMF is controversial and highly dependent on the particular patient and complexity of the trauma. In some cases where long-term MMF may be recommended, the surgeon may choose to leave the patient out of MMF immediately postoperatively because of concerns of edema, postoperative sedation, and airway. In these cases the surgeon may choose to place the patient in MMF after these concerns have been resolved.
The need and duration of MMF is very much dependent on:
- Fracture morphology
- Type and stability of fixation (including palatal splints)
- Dentition
- Coexistence of mandibular fractures
- Premorbid occlusion
Oral hygiene
Patients with arch bars and/or intraoral incisions and/or wounds must be instructed in appropriate oral hygiene procedures. The presence of the arch bars or elastics makes this a more difficult procedure. A soft toothbrush (dipped in warm water to make it softer) should be used to clean the surfaces of the teeth and arch bars. Elastics are removed for oral hygiene procedures. Chlorhexidine oral rinses should be prescribed and used at least 3 times a day to help sanitize the mouth.
For larger debris, a 1:1 mixture of hydrogen peroxide/chlorhexidine can be used. The bubbling action of the hydrogen peroxide helps remove debris. A Waterpik® is a very useful tool to help remove debris from the wires. If a Waterpik is used, care should be taken not to direct the jet stream directly over intraoral incisions as this may lead to wound dehiscence.
Special considerations for orbital fractures
Travel in commercial airlines is permitted following orbital fractures. Commercial airlines pressurize their cabins. Mild pain on descent may be noticed. However, flying in military aircraft should be avoided for a minimum of six weeks.
No scuba diving should be permitted for at least six weeks.













