Open reduction internal fixation
1. Principles
General considerations
Modalities of treatment for open reduction internal fixation (ORIF) are controversial. With most options for treatment, the surgeon should plan on placing arch bars and using MMF. Depending on the nature of the fracture, the surgeon may or may not choose to leave the patient in MMF for a period of time postoperatively.
The first option is to perform an ORIF of the palatal fracture with fixation of one or more plates on the palate through a palatal approach. If there has been significant splaying, palatal laceration in this area is common. Alternative to placing the plate submucosally in the palatal region, it could be placed on the surface of the mucosa and removed at a later point. Locking screw/plate systems allow epimucusal application of bone plates. A second plate is placed on the anterior alveolar segment, taking care not to injure the tooth roots.
A second option is to reduce the fracture and use a palatal splint.
A third option is a combination of the first two options where ORIF is performed and a palatal splint added for further stability.
If there is significant splaying of the fracture and instability of the palate, most surgeons opt for the first or third option. Some surgeons feel that the first option alone would provide adequate stability. Others feel that if the first option is not combined with a palatal splint, there is a risk of having some lingual splaying of the teeth when the patients are placed into MMF.
In the following explanation we will demonstrate the third option.
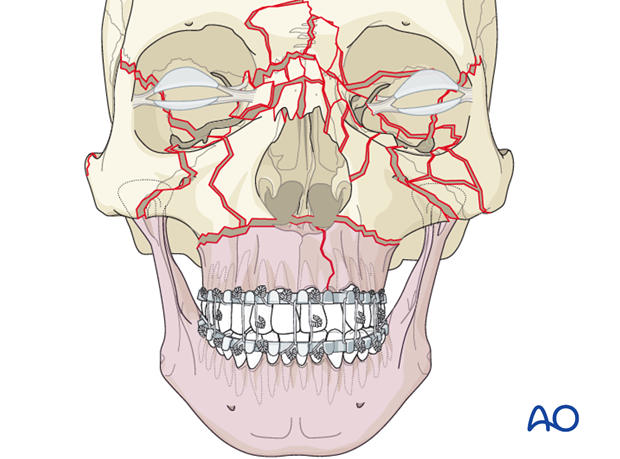
Panfacial trauma
In a panfacial trauma, which is the common situation where we see a palatal fracture, high priority should be given to reestablishment of the maxillomandibular unit early in the case. In the illustrated case, reduction and fixation of the palatal fracture should be the first step in the procedure.
Teaching video
AO Teaching video on fixation of a complex midface fracture
2. Approach
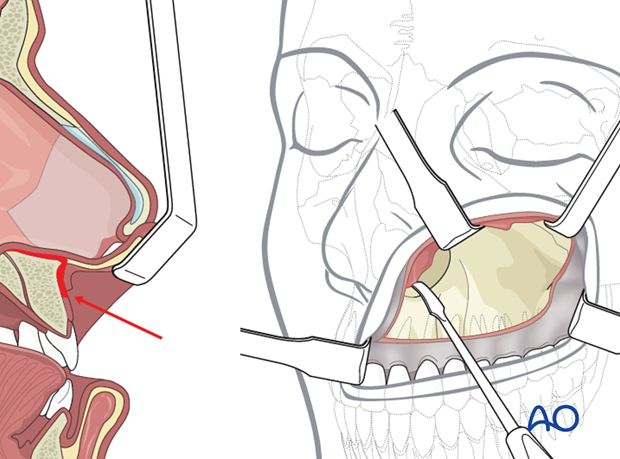
For this procedure, standard approaches to the maxilla are used. However, if present, lacerations can be used to directly access fracture site for fracture managment.
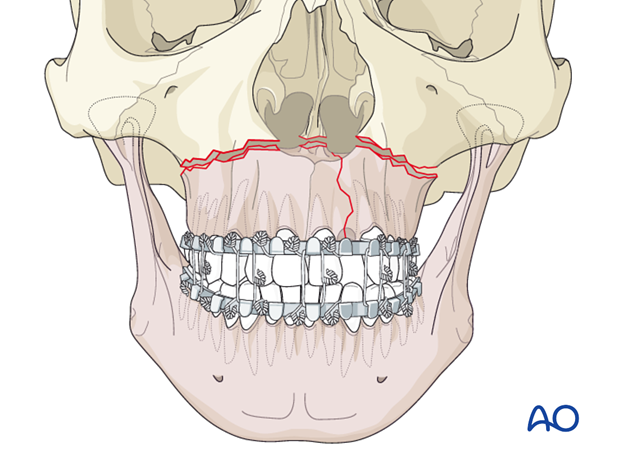
3. Reduction
Manual reduction
Perform the reduction by applying pressure laterally on the two maxillary halves to reduce the splayed fracture.
Depending on the stability of the reduction and the number of assistants in the operating room, the surgeon decides as to whether to begin with the arch bars or the plating.
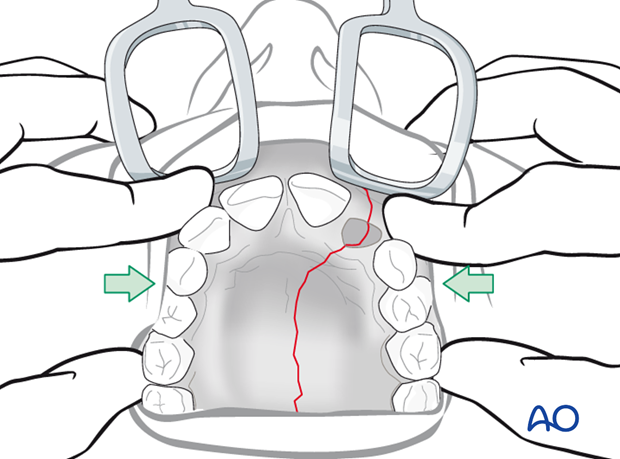
Reduction might be facilitated by placing a transpalatal wire to span the molars and compress whereby the fracture is reduced.
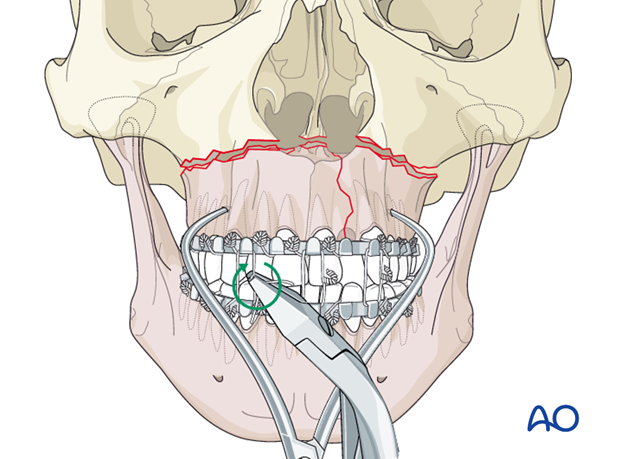
Apply MMF
Arch bars are applied and the occlusion is checked. The occlusion is then secured by mandibulomaxillary fixation (MMF). Click here for a detailed description of the MMF technique.
Pearl: securing the reduction
It can be beneficial to use forceps to maintain the reduction while securing the MMF.
4. Fixation
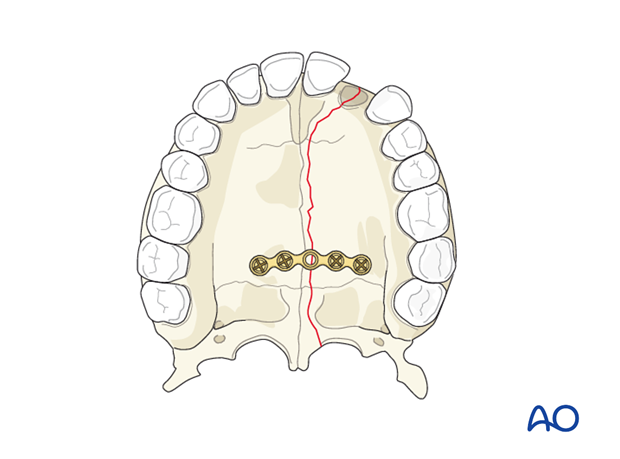
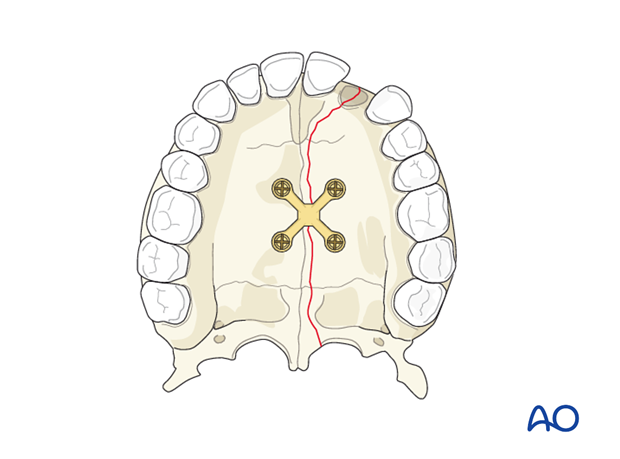
Plate application
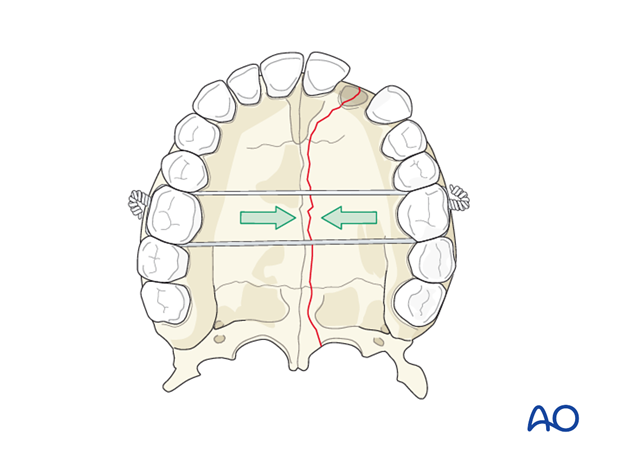
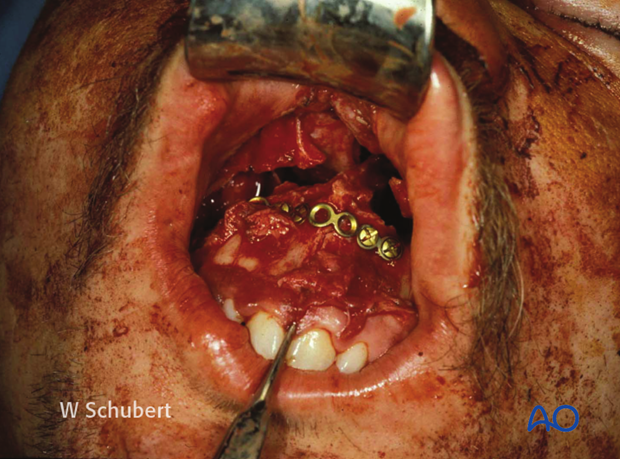
Fixation should be considered in two planes. This includes placement of plates in the palate, and a plate in the anterior alveolar arch, taking care to avoid injury to the dental roots.
It may be desirable to first plate the palate while a perfect reduction of the previously splayed palate is visualized.
More information on CMF implants can be found here.
This illustration shows a straight plate placed on the bone or on the mucosa thus through transmucosal screws.
Alternatively, an X plate can be considered.
If the surgeon decides to also use a palatal splint to provide further stabilization of the palatal unit, the palatal laceration (if present) needs to be repaired, prior to application of the splint.
Note: An acrylic splint can help 3-D stabilization of the dental arch and protect the palatal tissues.
Placing the second plate
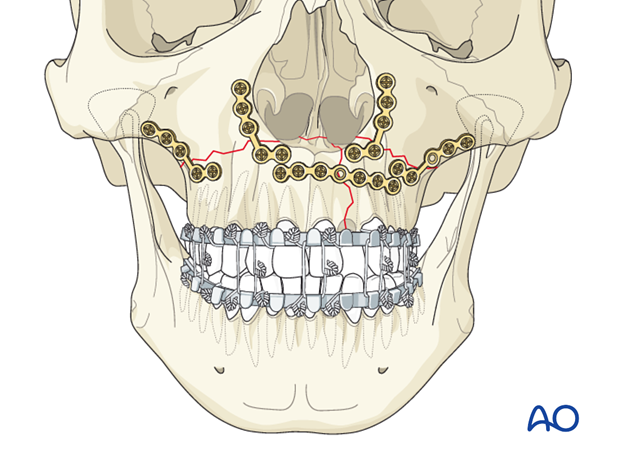
In placing the second plate on the anterior alveolar fracture, consider the position of additional plates to be placed for the fixation of the Le Fort I fracture.
Care must be taken to avoid the dental roots.

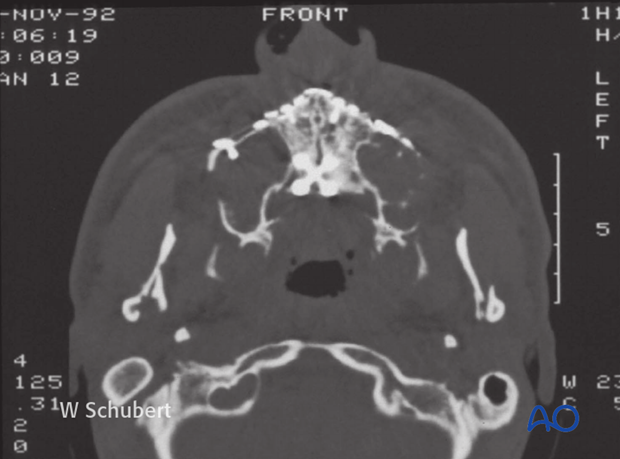
In this axial CT scan the surgeon has chosen an X-plate for fixation of the palatal fracture. Further stabilization has been accomplished with the use of the anterior alveolar plate.
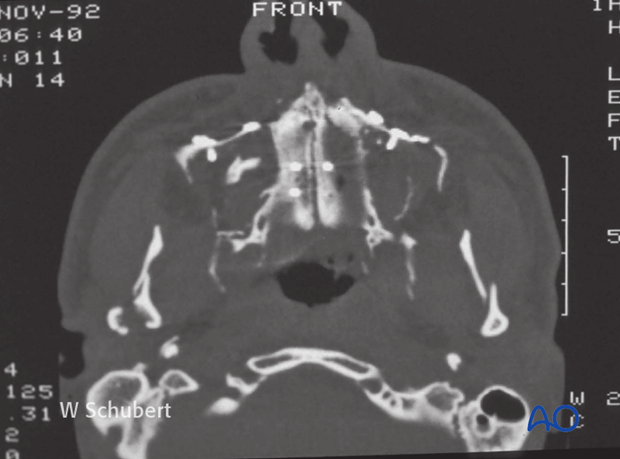
This is an axial view of the same patient and better demonstrates the palatal reduction.
Splint application
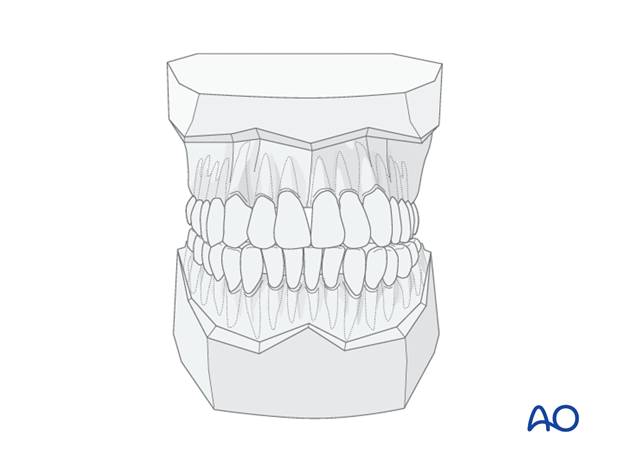
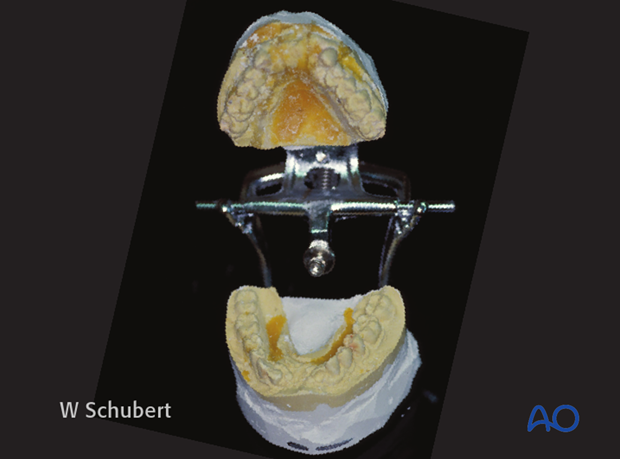
In some cases, the surgeon may consider taking dental impressions, making dental models, and from these models making a palatal splint. Such a splint will support soft-tissue healing in the palate. The palatal splint is then wired to the dentition also possibly using arch bars. Depending on the stability of the palatal unit, as well as other complicating issues regarding other midface fractures and postoperative airway, the surgeon may choose to leave the patient in postoperative MMF.
In cases where there has been splaying of the palate, cuts are made in the maxillary portion of the dental model, along the line of the palatal fracture, with repositioning of the maxillary model to determine the premorbid contour of the maxillary arch. This is accomplished using the mandibular impression. Once the maxillary model has been adjusted to its premorbid shape, the palatal splint is made with the use of this maxillary model.
In the photographs, dental impressions have been taken, models have been made, …
… and a clear plastic palatal splint has been made.
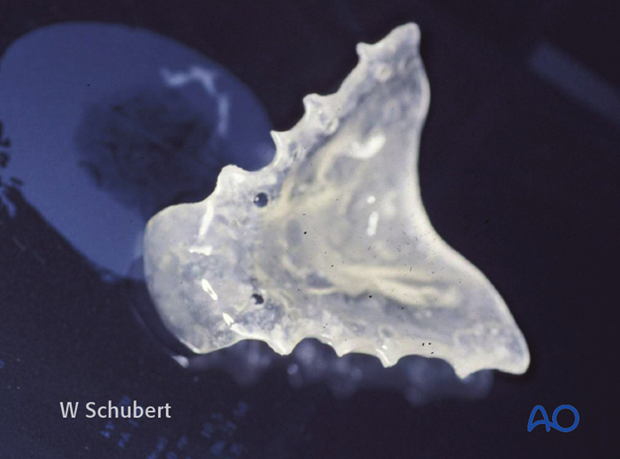
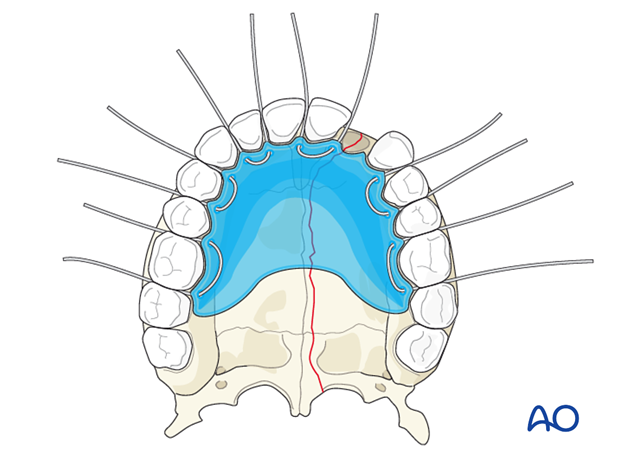
In this photograph, the palatal splint has been inserted. Holes have been drilled through the palatal splint and are used to fixate the wires to the arch bar.

Addressing the Le Fort I fracture
In the illustrated case, the Le Fort I fracture should be addressed after the palatal unit has been repaired. Please refer to the section on Le Fort fractures for further details.
5. Aftercare following open reduction and internal fixation of Le Fort I and palatoalveolar fractures
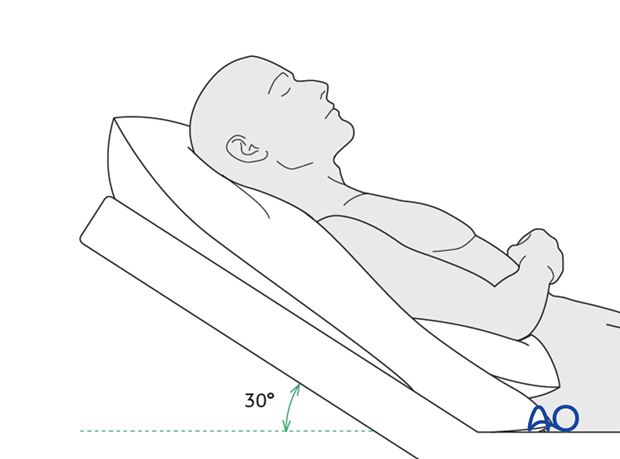
Postoperative positioning
Keeping the patient’s head in an upright position both preoperatively and postoperatively may significantly improve periorbital edema and pain.
Medication
The use of the following perioperative medication is controversial. There is little evidence to make strong recommendations for postoperative care.
- No aspirin or nonsteroidal antiinflammatory drugs (NSAIDs) for 7 days
- Analgesia as necessary
- Antibiotics (many surgeons use perioperative antibiotics. There is no clear advantage of any one antibiotic, and the recommended duration of treatment is debatable.)
- Nasal decongestant may be helpful for symptomatic improvement in some patients.
- Steroids, in cases of severe orbital trauma, may help with postoperative edema. Some surgeons have noted increased complications with perioperative steroids.
- Ophthalmic ointment should follow local and approved protocol. This is not generally required in case of periorbital edema. Some surgeons prefer it. Some ointments have been found to cause significant conjunctival irritation.
- Regular perioral and oral wound care has to include disinfectant mouth rinse, lip care, etc.
Ophthalmological examination
Postoperative examination by an ophthalmologist may be requested. The following signs and symptoms are usually evaluated:
- Vision (except for alveolar ridge fracture, palatal fracture)
- Extraocular motion (motility) (except alveolar ridge fracture, palatal fracture)
- Diplopia (except Le Fort I, alveolar ridge fracture, palatal fracture)
- Globe position (except Le Fort I, alveolar ridge fracture, palatal fracture)
- Perimetric examination (except Le Fort I, alveolar ridge fracture, palatal fracture)
- Lid position
- If the patient complains of epiphora (tear overflow), the lacrimal duct must be checked.
Note: In case of postoperative double vision, ophthalmological assessment has to clarify the cause. Use of prism foils on existing glasses may be helpful as an early aid.
Postoperative imaging
Postoperative imaging has to be performed within the first days after surgery. 3-D imaging (CT, cone beam) is recommended to assess complex fracture reductions. An exception may be made for centers capable of intraoperative imaging.
Especially in fractures involving the alveolar area, orthopantomograms (OPG) are helpful.
Wound care
Remove sutures from skin after approximately 5 days if nonresorbable sutures have been used.
Apply ice packs (may be effective in a short term to minimize edema).
Avoid sun exposure and tanning to skin incisions for several months.
Diet
Diet depends on the fracture pattern.
Soft diet can be taken as tolerated until there has been adequate healing of the maxillary vestibular incision.
Intranasal feeding may be considered in cases with oral bone exposure and soft-tissue defects.
Patients in MMF will remain on a liquid diet until such time the MMF is released.
Clinical follow-up
Clinical follow-up depends on the complexity of the surgery, and whether the patient has any postoperative problems.
With patients having fracture patterns including periorbital trauma, issues to consider are the following:
- Globe position
- Double vision
- Other vision problems
Other issues to consider are:
- Facial deformity (incl. asymmetry)
- Sensory nerve compromise
- Problems of scar formation
Issues to consider with Le Fort fractures, palatal fractures and alveolar ridge fractures include:
- Problems of dentition and dental sensation
- Problems of occlusion
- Problems of the temporomandibular joint (TMJ), (lack of range of motion, pain)
Implant removal
Implant removal is rarely required. It is possible that this may be requested by patients if the implant becomes palpable or visible. In some countries it will be more commonly requested. There have been cases where patients have complained of cold sensitivity in areas of plate placement. It is controversial whether this cold sensitivity is a result of the plate, a result of nerve injury from the original trauma, or from nerve injury due to trauma of the surgery. Issues of cold sensitivity generally improve or resolve with time without removal of the hardware.
Generally, orbital implant removal is not necessary except in the event of infection or exposure. Readmission might be indicated if long term stability of the orbital volume has not been maintained.
MMF
The duration and/or use of MMF is controversial and highly dependent on the particular patient and complexity of the trauma. In some cases where long-term MMF may be recommended, the surgeon may choose to leave the patient out of MMF immediately postoperatively because of concerns of edema, postoperative sedation, and airway. In these cases the surgeon may choose to place the patient in MMF after these concerns have been resolved.
The need and duration of MMF is very much dependent on:
- Fracture morphology
- Type and stability of fixation (including palatal splints)
- Dentition
- Coexistence of mandibular fractures
- Premorbid occlusion
Oral hygiene
Patients with arch bars and/or intraoral incisions and/or wounds must be instructed in appropriate oral hygiene procedures. The presence of the arch bars or elastics makes this a more difficult procedure. A soft toothbrush (dipped in warm water to make it softer) should be used to clean the surfaces of the teeth and arch bars. Elastics are removed for oral hygiene procedures. Chlorhexidine oral rinses should be prescribed and used at least 3 times a day to help sanitize the mouth.
For larger debris, a 1:1 mixture of hydrogen peroxide/chlorhexidine can be used. The bubbling action of the hydrogen peroxide helps remove debris. A Waterpik® is a very useful tool to help remove debris from the wires. If a Waterpik is used, care should be taken not to direct the jet stream directly over intraoral incisions as this may lead to wound dehiscence.













