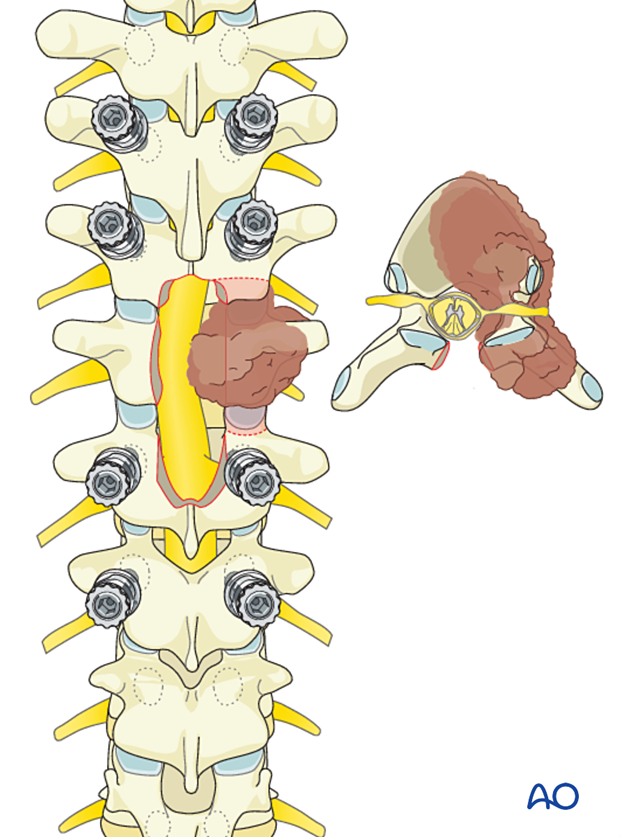
Intralesional resection (T1 to T12)
1. Introduction
Preoperative management
Proper planning is instrumental in the management of primary spine tumors. A multidisciplinary approach may be required depending on the localization of the tumor.
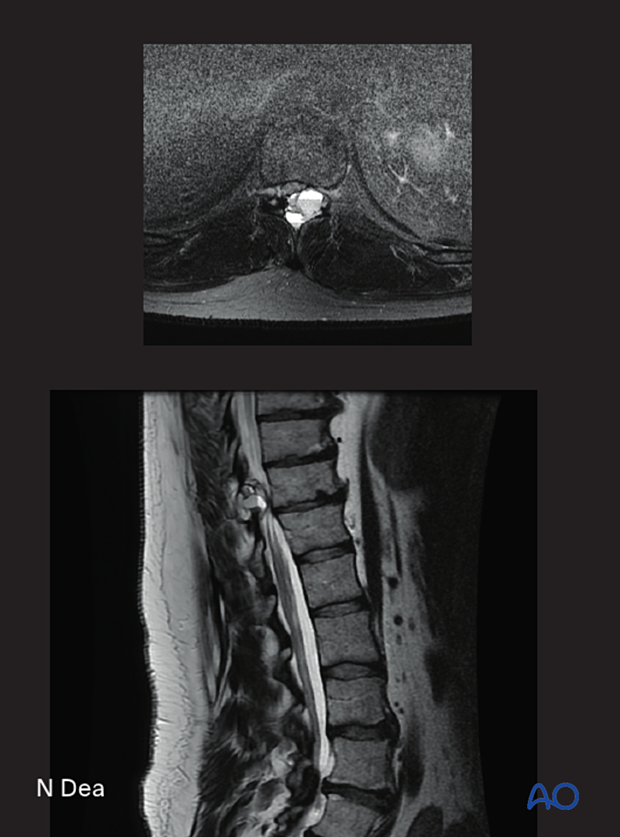
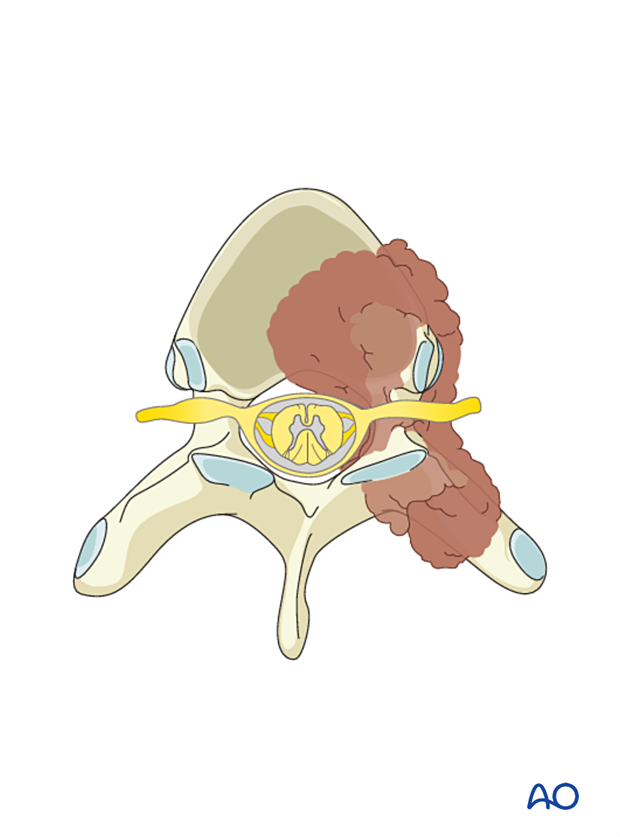
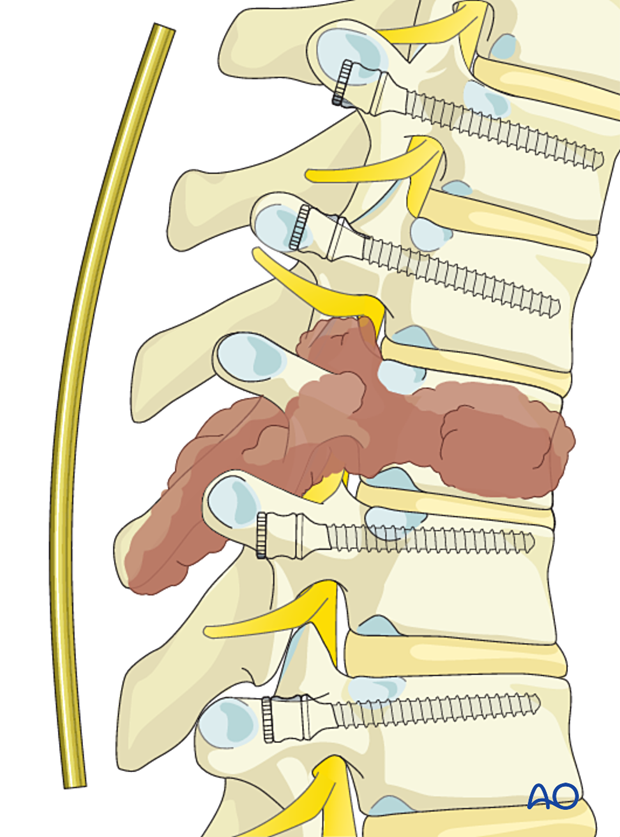
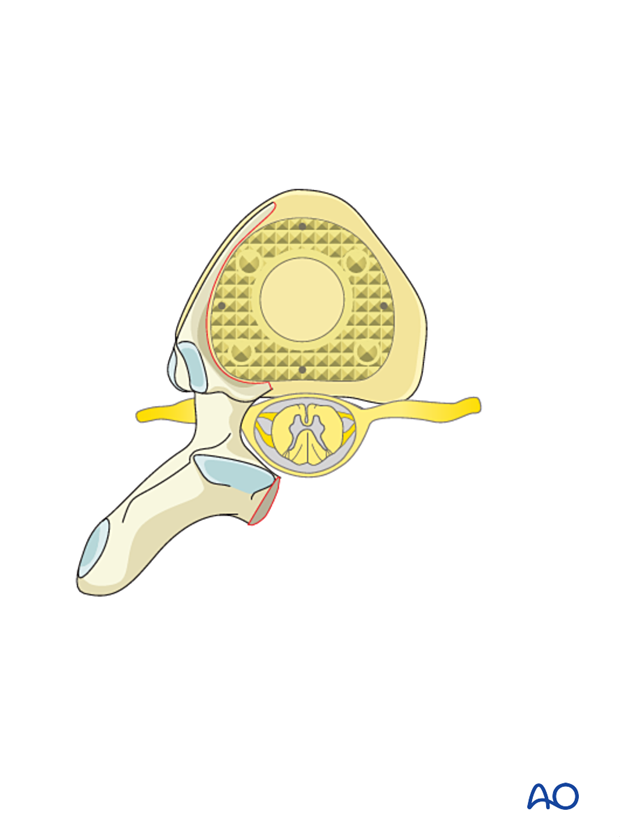
This picture shows a T11 aneurysmal bone cyst.
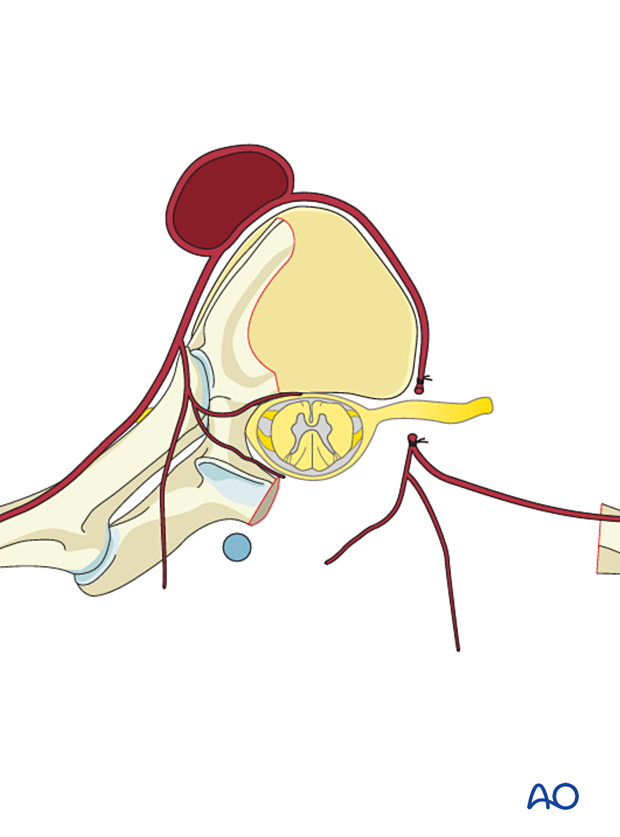
Embolization
Embolization procedures are recommended to reduce operative blood loss in hypervascular tumors, especially during more extensive resections.
Embolization should be considered for hypervascular tumors, such as giant cell tumors, aneurysmal bone cysts, and hemangiomas.
The role of the embolization is:
- To reduce the vascularity of the tumor
- To facilitate dissection around the tumor
- Mapping of spinal cord vascular supply
Embolization on its own may also have a therapeutic effect.
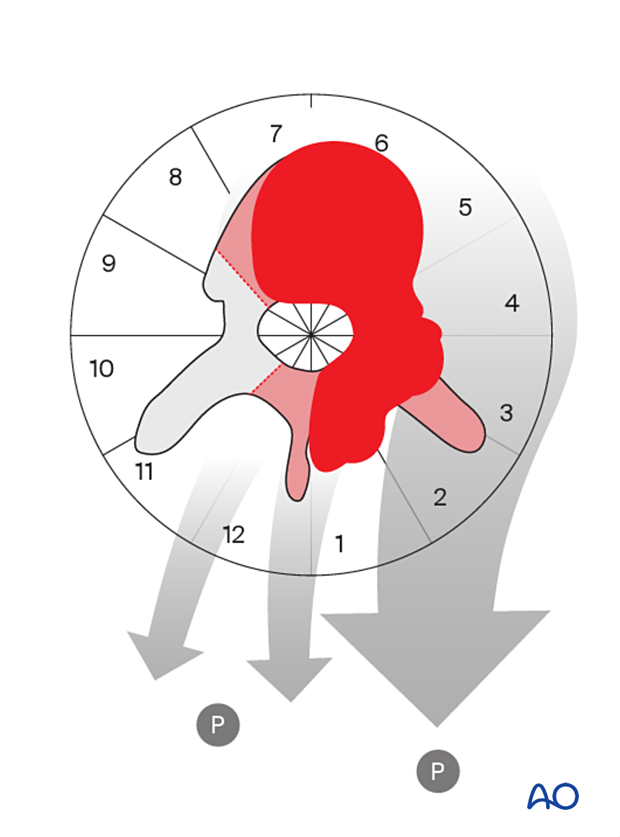
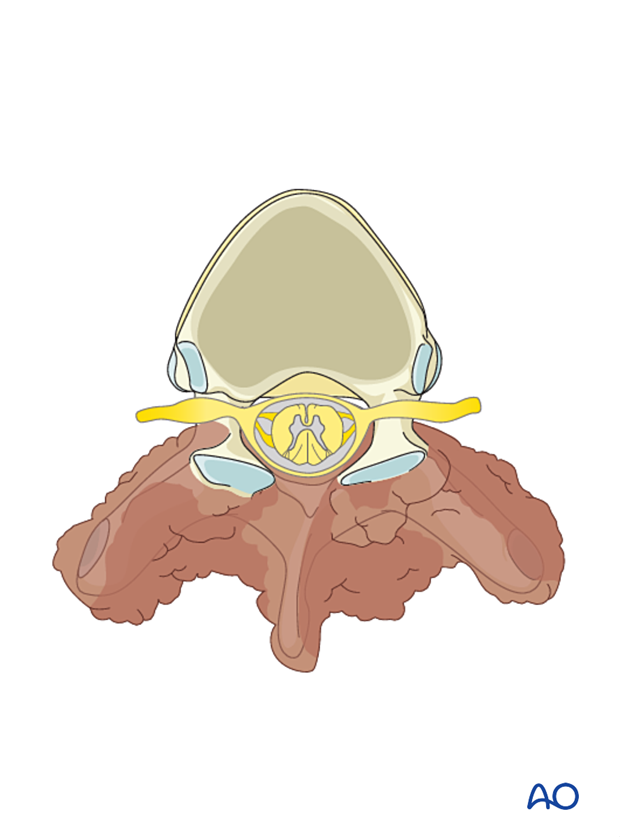
This image shows the embolization of a hypervascular tumor.

Resection strategy
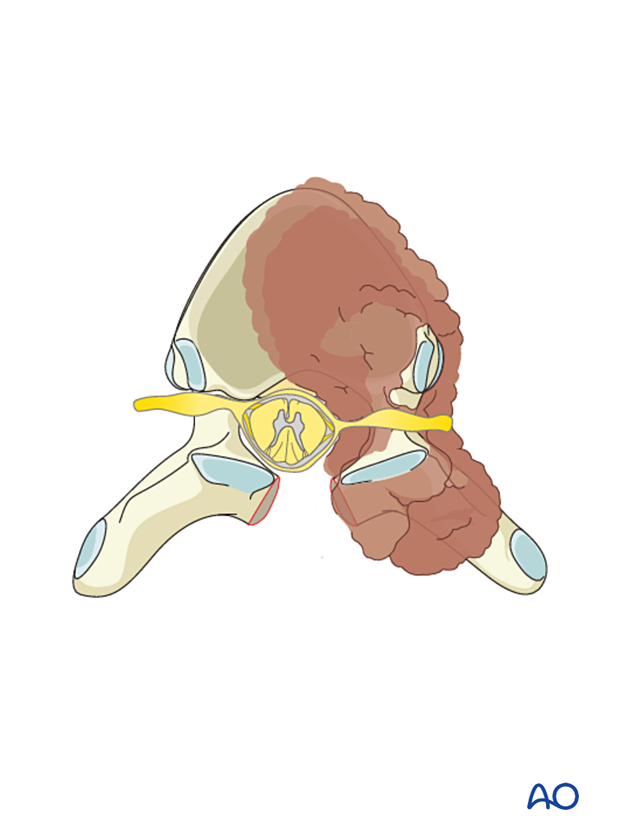
Most benign primary tumors will be localized in the posterior element with variable extension into the vertebral body. These tumors are approached and resected through a posterior approach only.
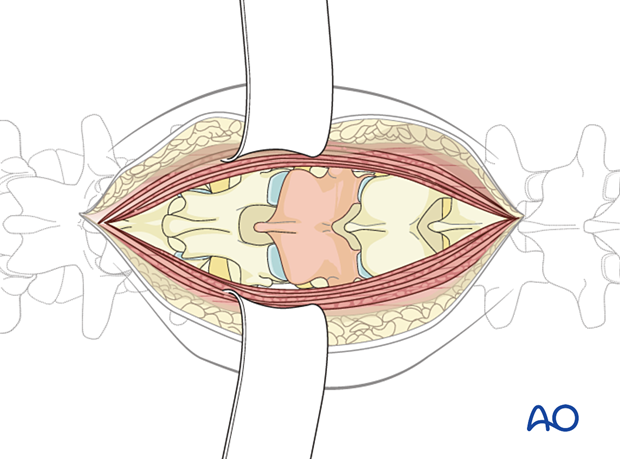
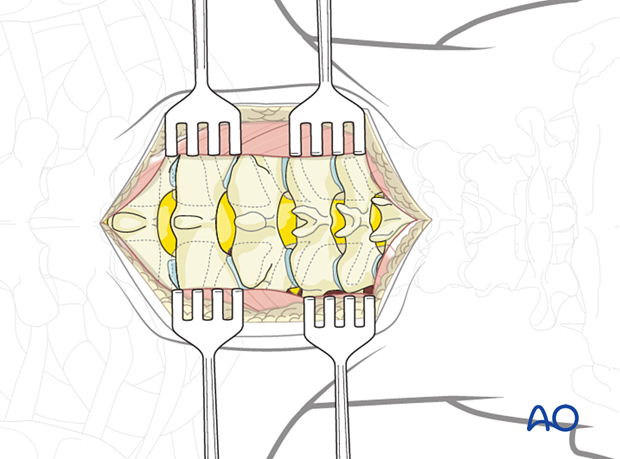
A wide visualization is essential in these cases, and a laminectomy involving half a level above and below the tumor is recommended.
The goal is to achieve:
- Good visualization of normal and abnormal anatomy
- Safe decompression of the neural elements
Reconstruction strategy
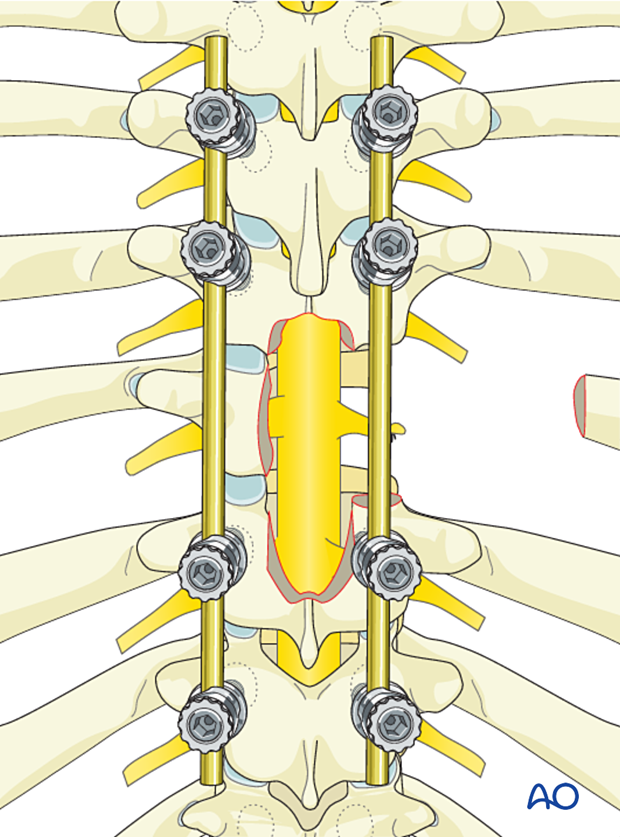
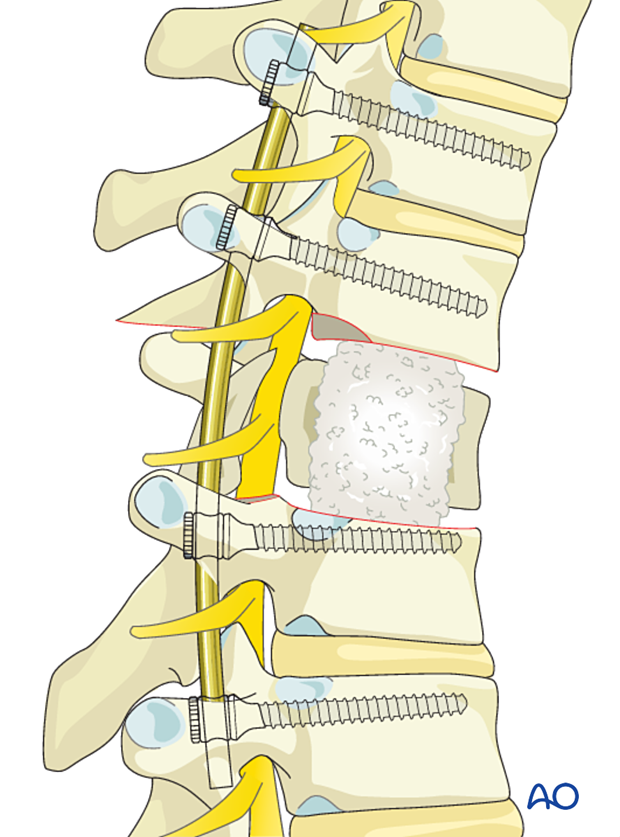
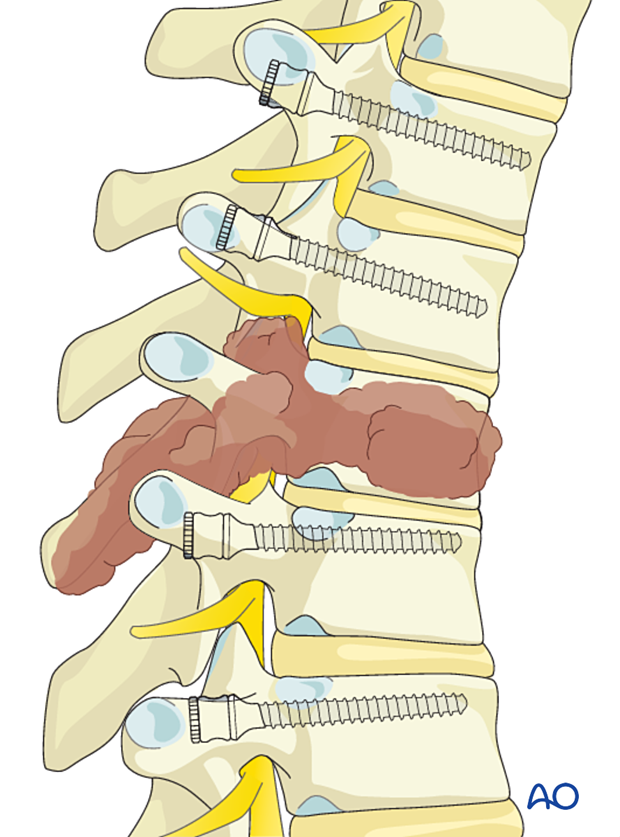
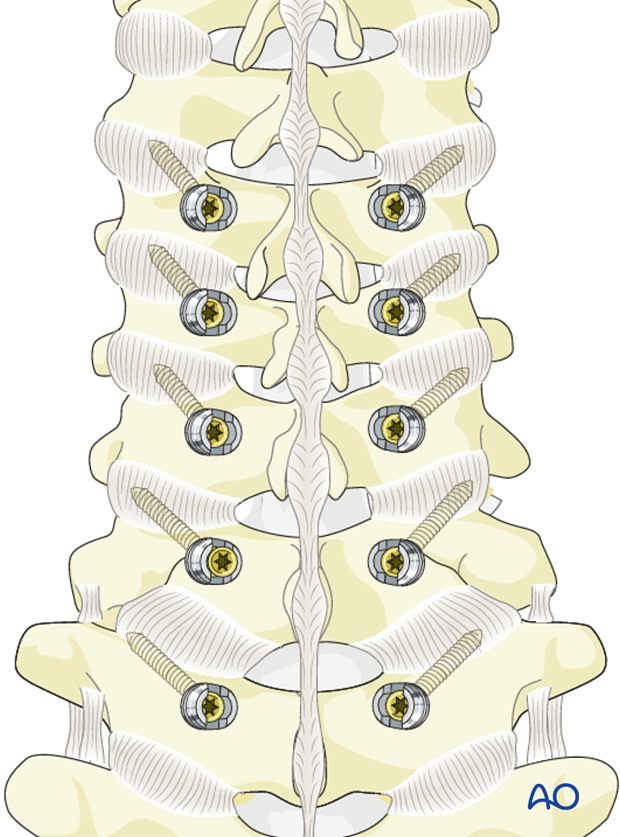
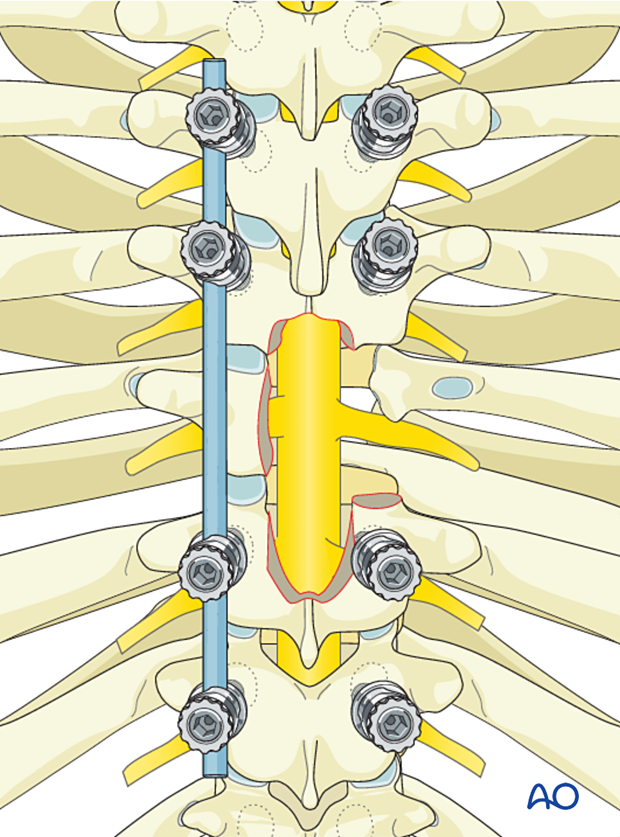
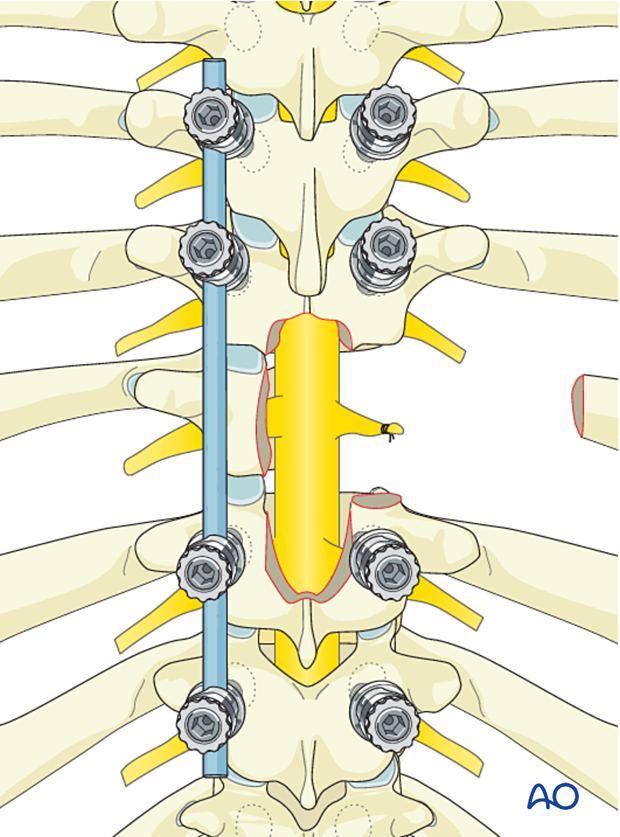
Posterior reconstructionIn patients requiring posterior lateral decompression but no anterior column reconstruction, at least one level above and below the involved segment should be instrumented.
If the vertebral body is involved, at least two levels above and below the involved segment should be instrumented.
Short segment constructs lead to increased stress on the posterior implants, which increases the risk of implant failure (screw pullout/fracture).
The risk of implant failure may be decreased by cement augmentation of fenestrated screws and reconstitution of the anterior column using cement augmentation or a cage.
As the procedure is often curative, it is important to verify that the spine is reconstructed in good alignment, and a solid bony union should be attempted.
If a posterior element tumor only involves segments 1 and/or 12, resection can be performed without the need for an instrumented fusion.
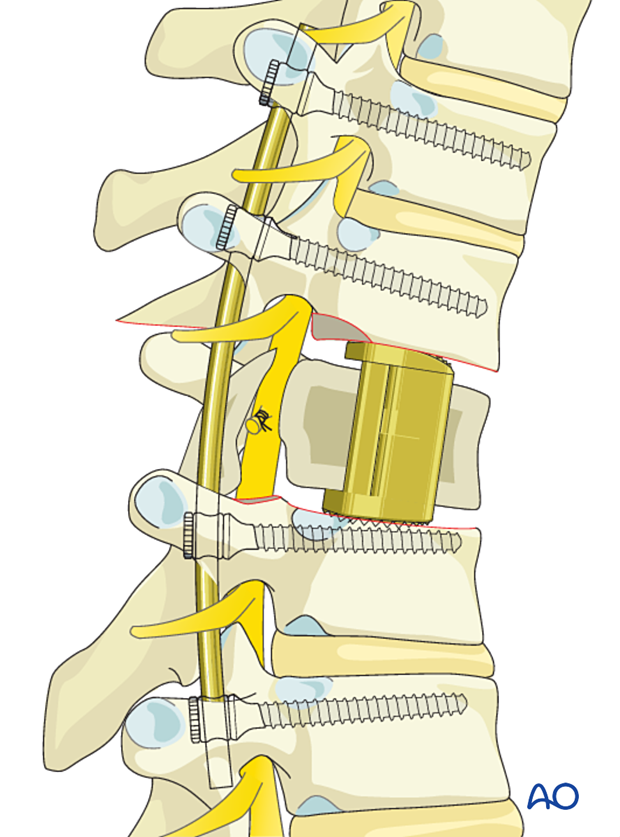
Depending on the extent of the vertebral body resection, anterior reconstruction may be required. Reconstruction can be achieved with PMMA or an expandable cage.
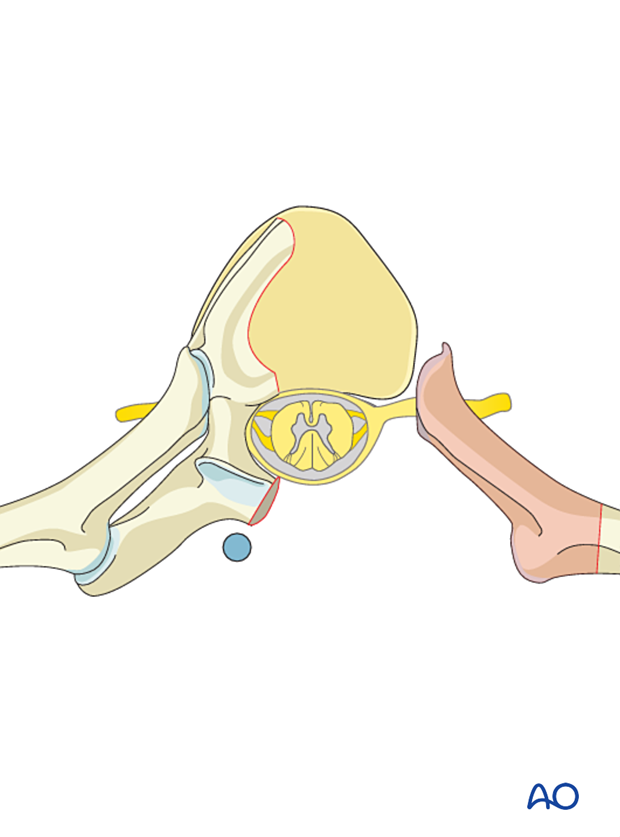
When an expandable cage is chosen, a unilateral sacrifice of the thoracic nerve root will be required.
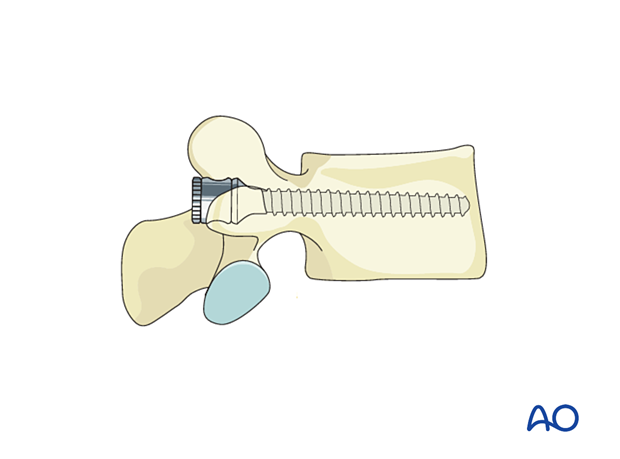
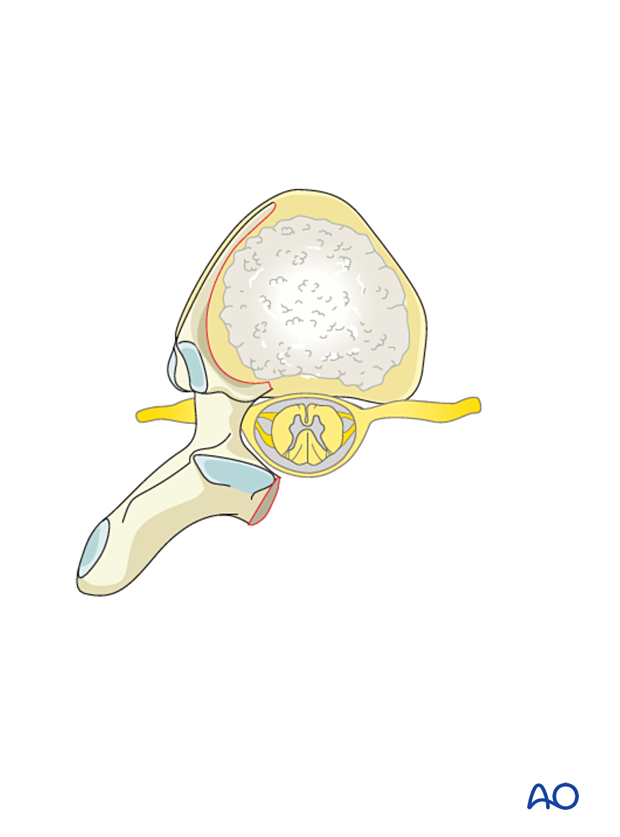
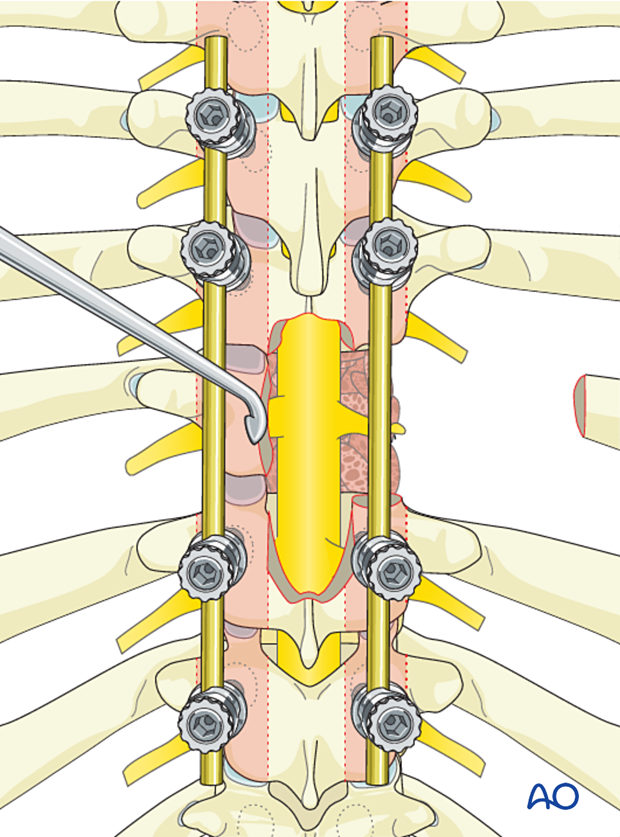
Reconstruction with PMMA can be done in different ways, as shown here:
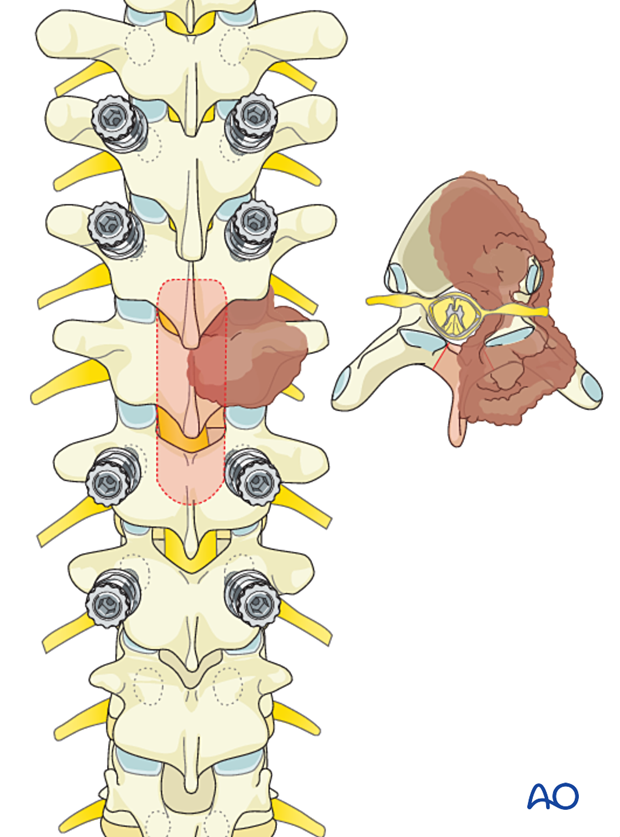
For unilateral primary tumors, the noninvolved side will often be instrumented.
When postoperative SBRT is considered, the affected vertebras should not be instrumented to facilitate radiotherapy planning and delivery.
If the tumor involves the posterior element bilaterally, then the affected vertebra will not be instrumented.
Case-based scenario
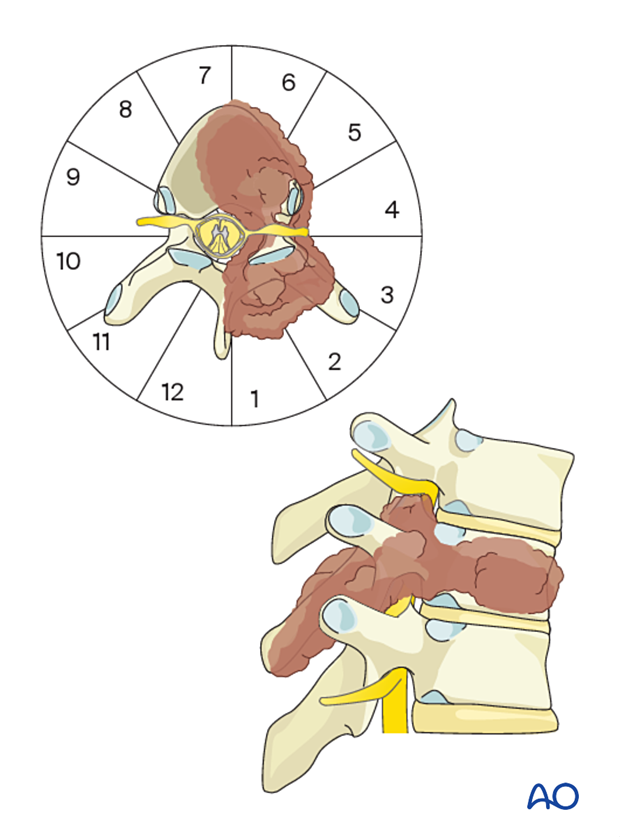
Most benign primary tumors will be localized in the posterior element with variable extension into the vertebral body.
Every case is unique.
To illustrate the surgical principle of a posterior intralesional resection, including a significant portion of the vertebral body, we will use a T9 tumor located in segments 1–7 of the WBB classification.
2. Patient preparation and surgical approach
Patient preparation
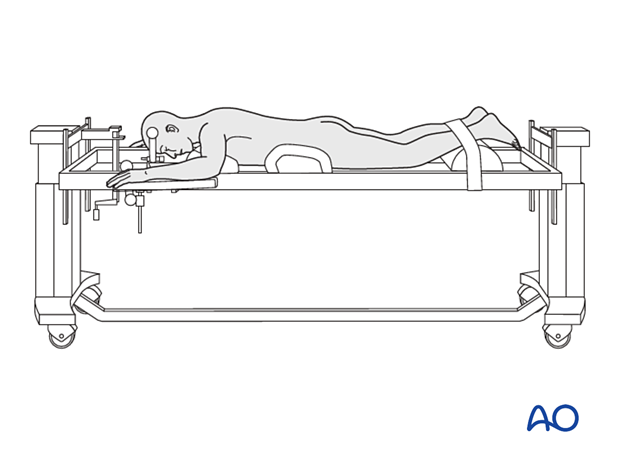
The patient is placed prone.
Surgical access
A posterior midline approach is used.
A wider dissection will typically be performed for primary tumors compared to a trauma case.
Careful analysis of the preoperative imaging is important to avoid tumor violation during the approach.
Following a midline incision, the subcutaneous tissues are dissected down to the chosen dorsal plane of dissection.
The incision may need a cranial extension when the tumor involves the cervicothoracic junction.
3. Instrumentation
Screw insertion
Insert all screws according to the preoperative plan.
Optimal pedicle screw purchase will, in order of importance, be achieved by:
- Selecting the largest possible screw diameter according to the pedicle diameter
- Selecting the longest possible screw
- Positioning of the screw under the cranial endplate
- Cement augmentation of the screw
Thoracic pedicle screws are inserted according to the standard technique.
Rod preparation
Every effort should be made to contour the rod to decrease the risk of induced sagittal or coronal malalignment.
For further details about sagittal spinal alignment, refer to this section.
Cervicothoracic instrumentation
Extending instrumentation to the cervical spine may be necessary when the tumor involves the cervicothoracic junction.
4. Decompression
Laminectomy
Perform a laminectomy according to the preoperative plan.
Dissection should progress from normal to abnormal tissues to protect normal neurological elements and facilitate dissection.
Removal of facet joints
Depending on the position of the tumor, a complete resection of the facet joint and the pedicle may be required.
5. Tumor resection
Dissection of the tumor should progress from normal to abnormal tissues to protect normal neurological elements and facilitate dissection.
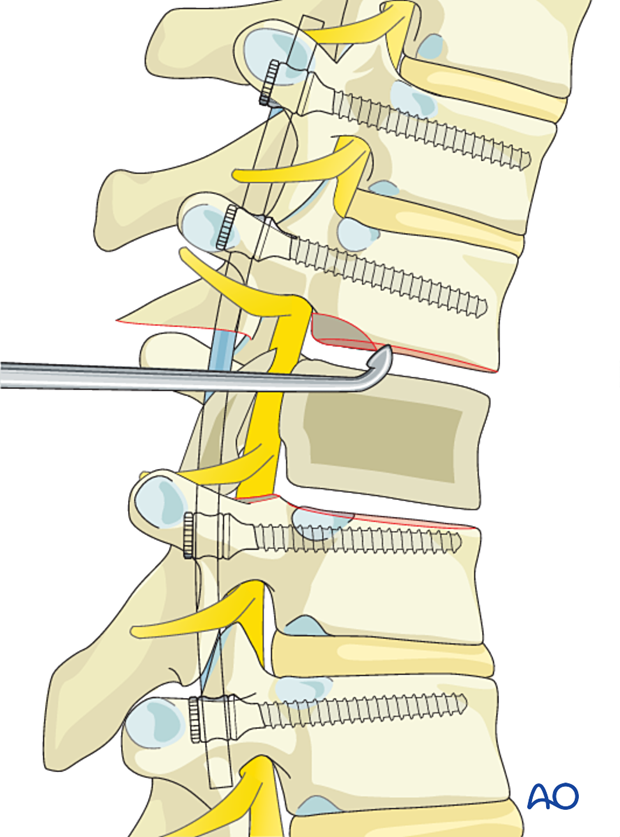
Use reverse-angle curettes and pituitary rongeurs to debulk the tumor.
Spinal cord mobilization should be minimized to reduce the risk of neurological injury.
The goal is to achieve gross total resection.
Intraoperative navigation can be used as an adjunct to maximize resection accuracy.
Once the tumor is entirely resected, the goal of the surgery is met.
6. Vertebral body reconstruction (if needed)
PMMA reconstruction
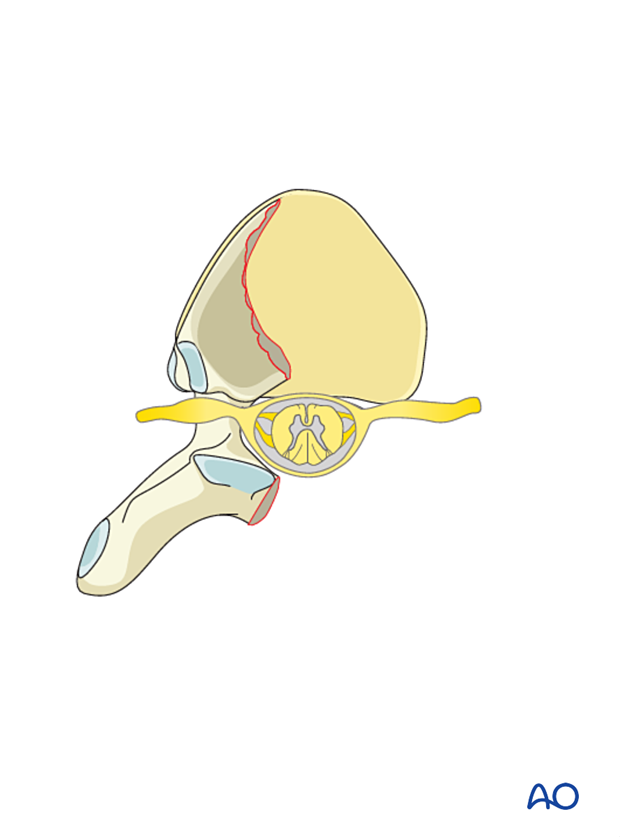
Depending on the extent of the vertebral body resection, anterior reconstruction may be required. Reconstruction can be achieved with PMMA or an expandable cage.
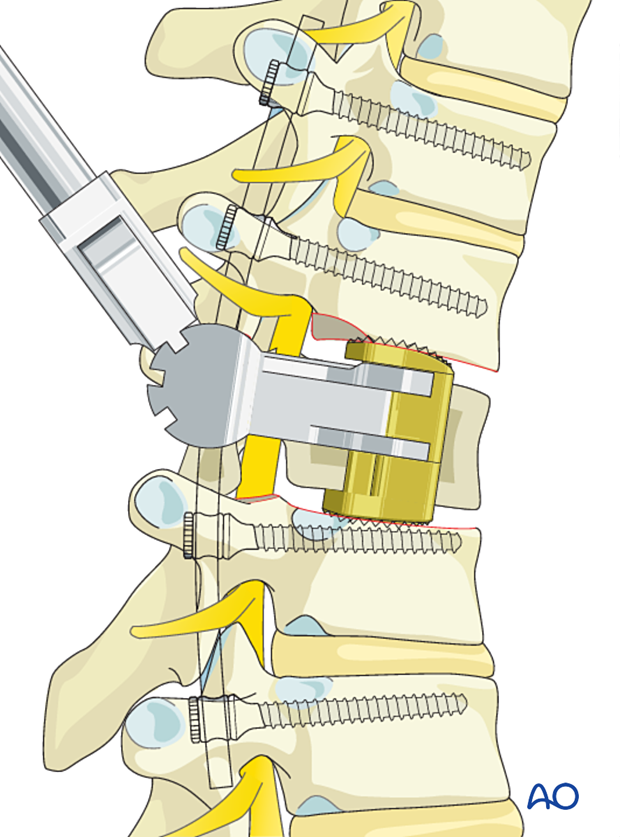
Reconstruction using cage
If a significant portion of the vertebral body is resected, stability may be compromised, and vertebral body stabilization should be considered.
Here we will describe an anterior column reconstruction from a posterolateral approach.
This technique can be used after an intralesional resection if most of the vertebral body has been resected.
A unilateral sacrifice of the thoracic nerve root will be required to insert the cage.
Insertion of contralateral rod
Insert a contralateral temporary rod to stabilize the spine and avoid spinal cord injury.
Remove the proximal rib (as shown in the illustration) to gain posterolateral access to safely insert the cage while minimizing spinal cord manipulation.
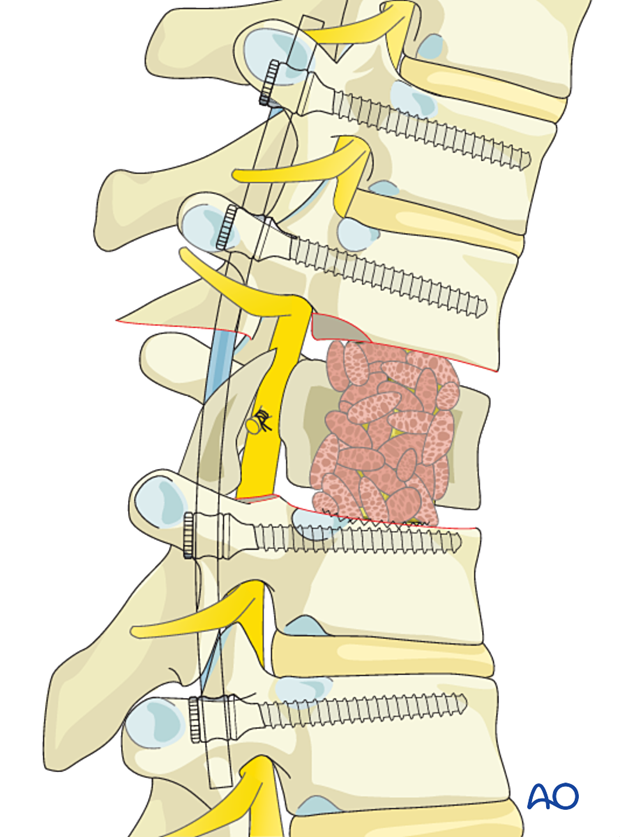
Discectomy
Incise the annulus fibrosis and remove the disc using a series of Kerrison rongeurs and curettes.
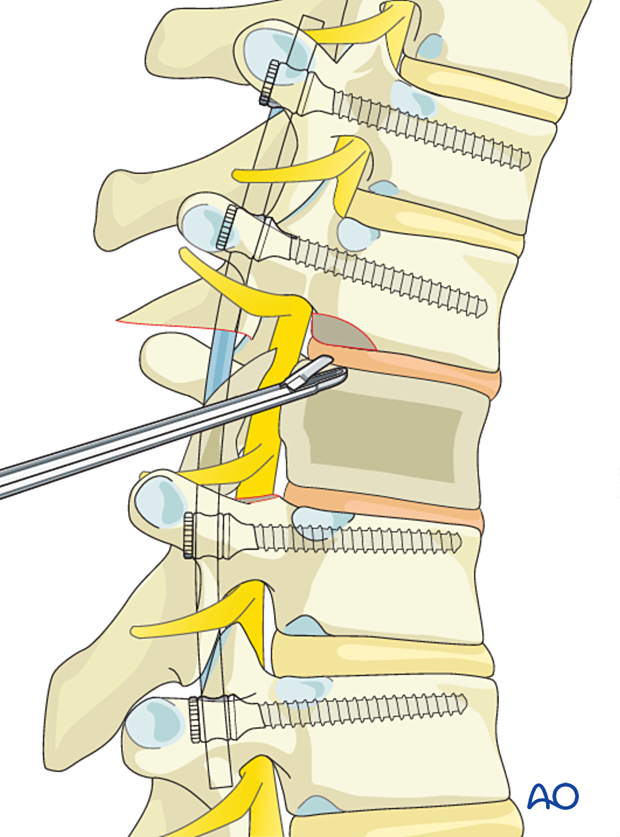
Prepare the endplates for fusion.
Ligation of segmental vessels
Ligate the segmental vessels according to the preoperative plan.
Nerve ligation
Ligate the thoracic nerve root of the involved level.
Cage insertion
Use calipers and implant templates to measure the height of the defect.
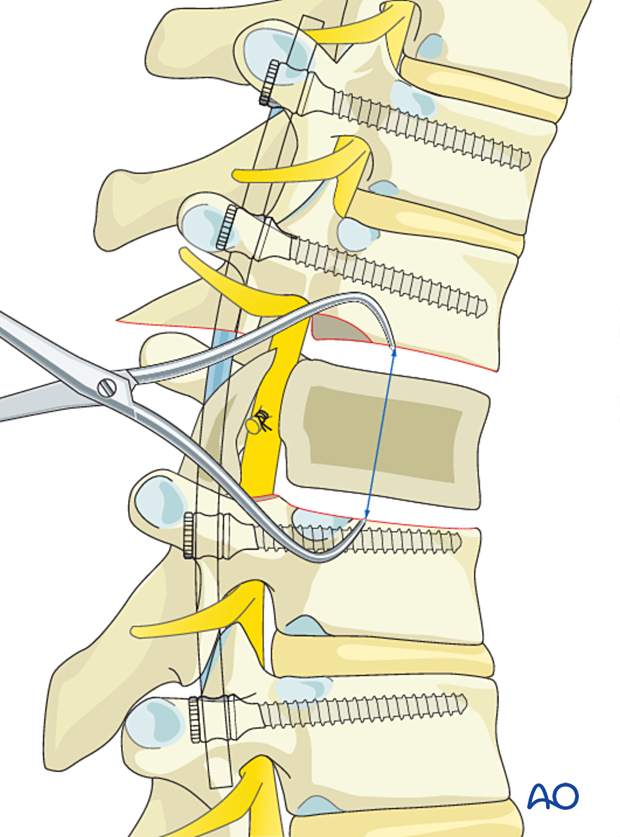
Insert an expandable prosthesis and expand it until the appropriate spinal alignment has been achieved.
Great care must be taken not to over-distract the cage. Endplate injury must also be avoided.
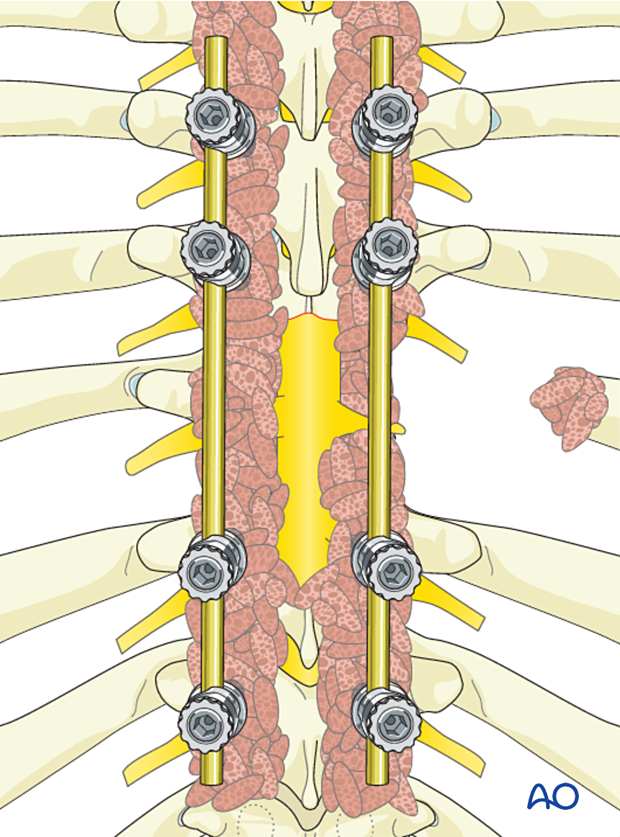
Bone grafting
Additional bone grafting can be used from the removed rib or allograft.
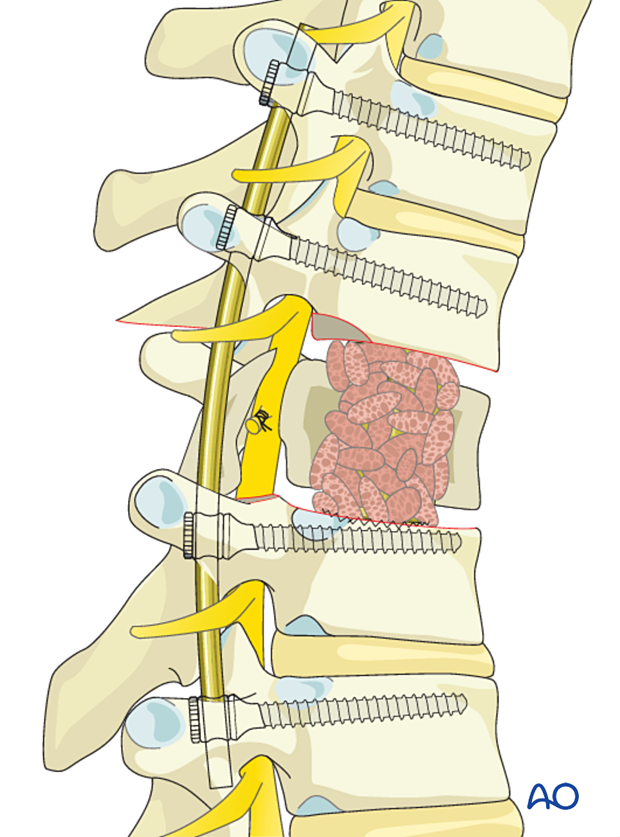
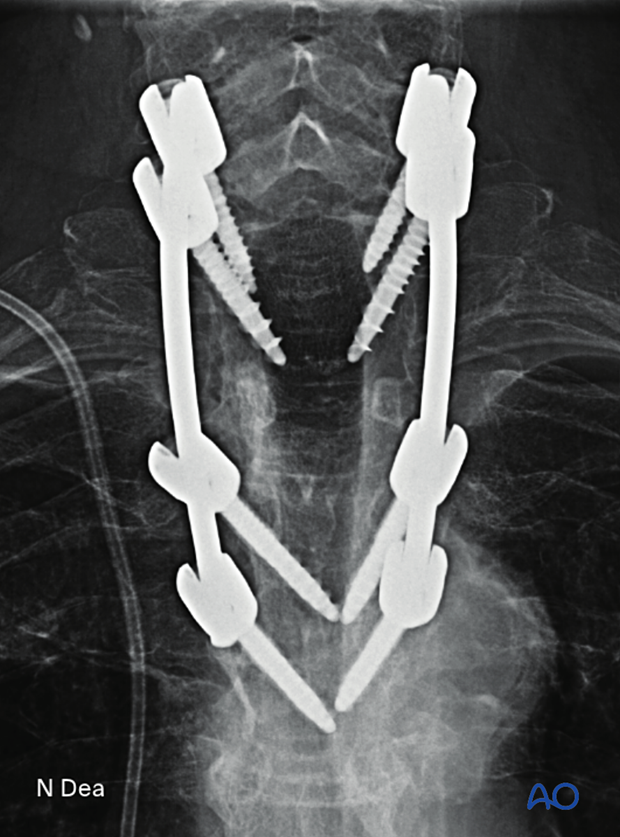
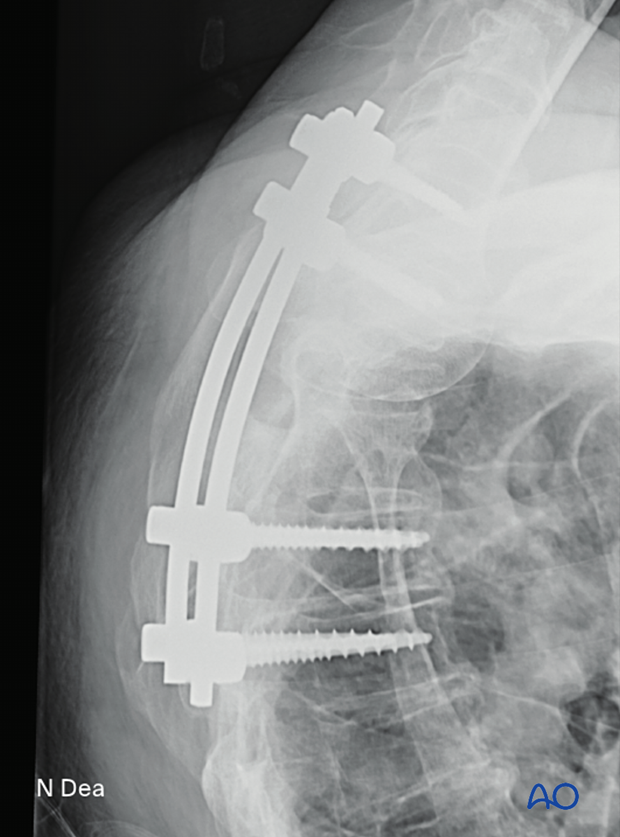
7. Posterior reconstruction
Insertion of final rod
Complete the rod insertion.
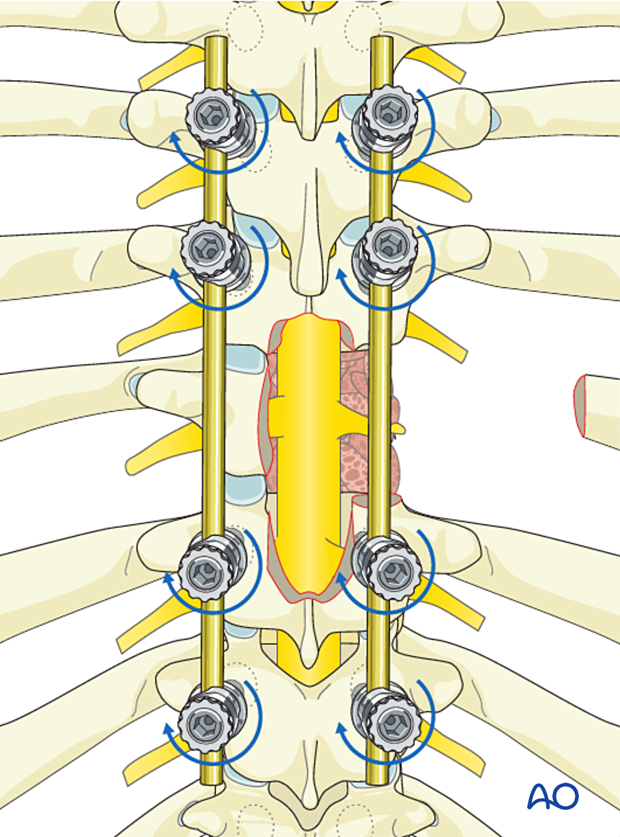
The final construct is shown from a lateral view.
8. Fusion
Preparation for fusion
Excise the facet capsule and denude/curette the joint surface cartilage surfaces and the posterior cortex.
Grafting
Insert pieces of bone graft (autograft, allograft) into the decorticated facet joint for fusion.
9. Intraoperative imaging
Before wound closure, intraoperative imaging is performed to check the adequacy of reduction, position, and length of screws and the overall coronal and sagittal spinal alignment.
Lateral view of the above case
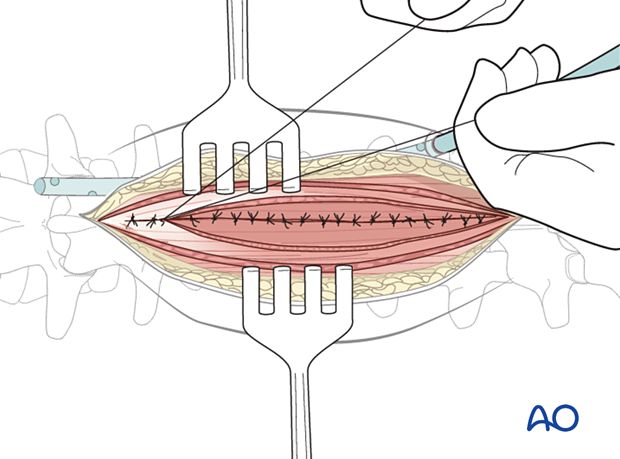
10. Posterior closure
Perform a multilayer closure as described in the approach.
For patients undergoing tumor surgery and/or with a history of radiation:
- Plastic surgery should perform soft-tissue reconstruction to decrease the risk of wound complications.
- Intrawound vancomycin can be applied to decrease the risk of postoperative wound complications.
11. Aftercare
Patients are made to sit up in bed on the first day after surgery. Patients with intact neurological status are made to stand and walk on the first day after surgery.
Patients can be discharged when medically stable or sent to a rehabilitation center if further care is necessary.
Throughout the hospital stay, adequate caloric intake of a high-quality diet should be monitored.
Patients are generally followed with periodical x-rays at 6 weeks, 3 months, 6 months, and 1 year to monitor for hardware failure and with an MRI every 6 months for tumor surveillance.
Some primary benign tumors of the spine can recur years after surgery, and long-term tumor surveillance is important.













