Occipitocervical fusion
1. Introduction
Preoperative planning
Based on CT and MRI imaging, a plan should be prepared to determine:
- The size and optimal location of implants used
- Whether spinal cord decompression is necessary and if so, the amount of tissue to remove in order to achieve sufficient spinal cord decompression
Every case will be unique, and we will here illustrate just one example.

2. Patient positioning and approach
This procedure is performed with the patient placed prone through a posterior approach.
3. Occipital fixation
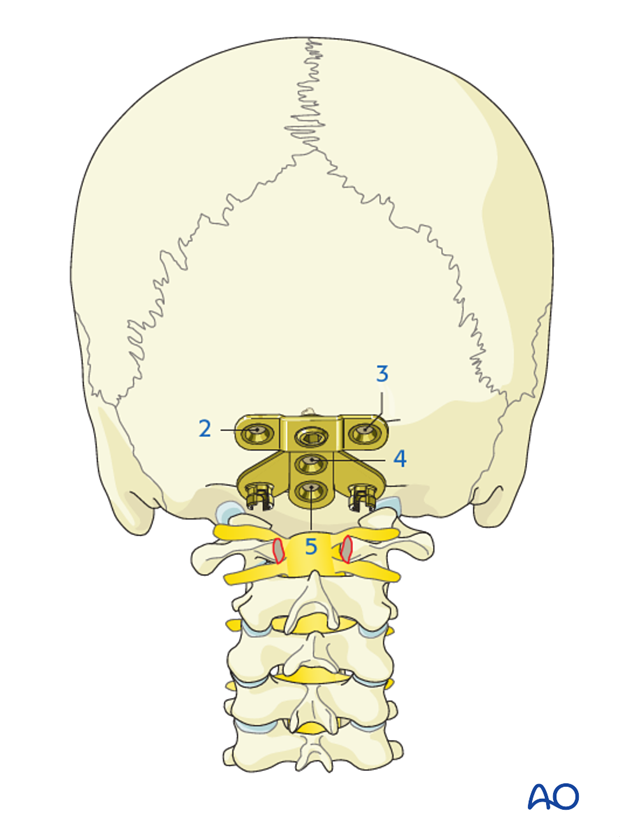
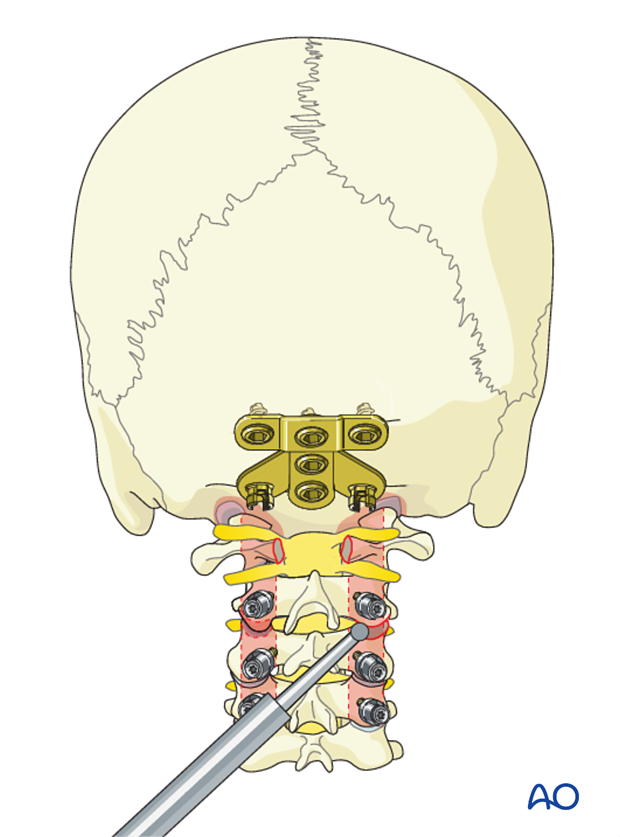
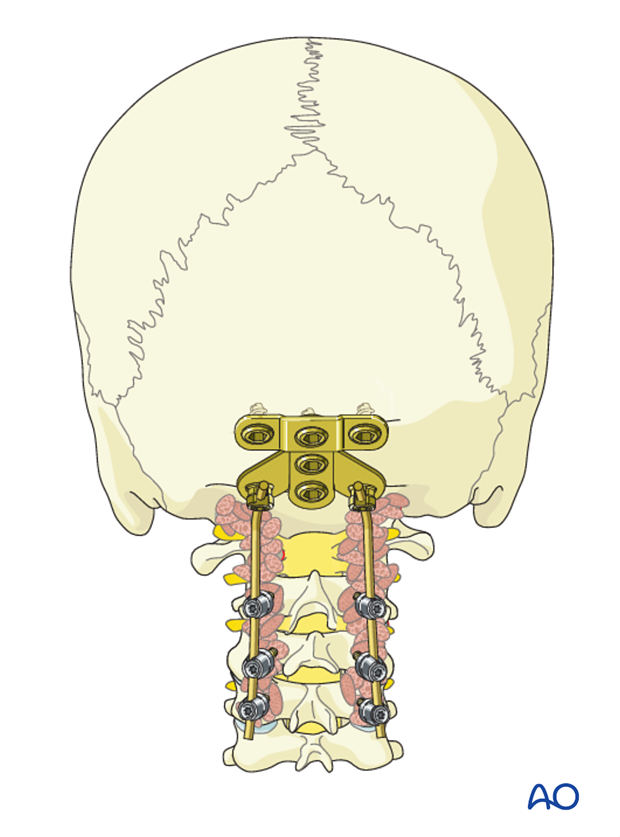
Occipital plate
There are several plate systems available for the occiput. Their application is based on the same principles and to illustrate these concepts, we will show the use of plate placed in the midline which allows for modularity and rotation when connecting to the rods.
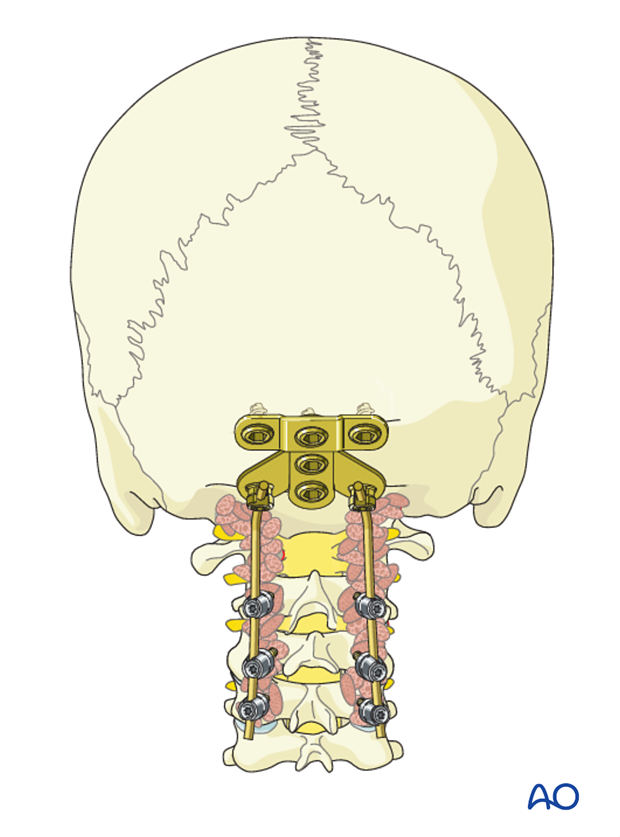
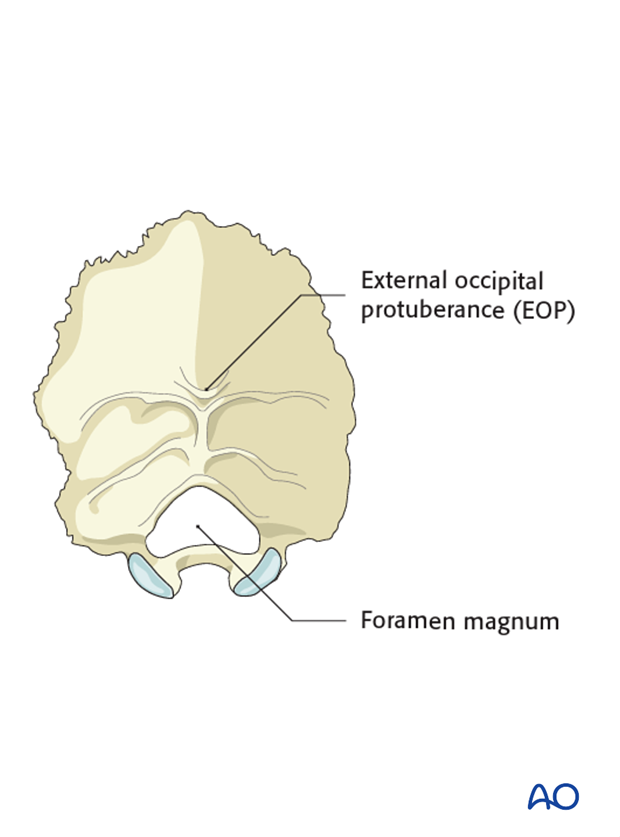
Plate placement
Independently of the plate system used, its placement should be close to but still caudal to the external occipital protuberance (EOP).
Placement of the plate at the EOP will increase the risk of erosion of the skin.
A too caudal position may compromise the foramen magnum.
Screw placement
The thickest part of the cranium is the dense ridge which runs vertically in line with the internal occipital crest.
The thickness of this crest is 11.5-15 mm in males and 10-12 mm in females and provides the best bone stock for screw purchase.
As you move laterally this crest becomes thinner and around 7-8 laterally to the midline, the bone thins out to a thickness of only 5-6 mm.
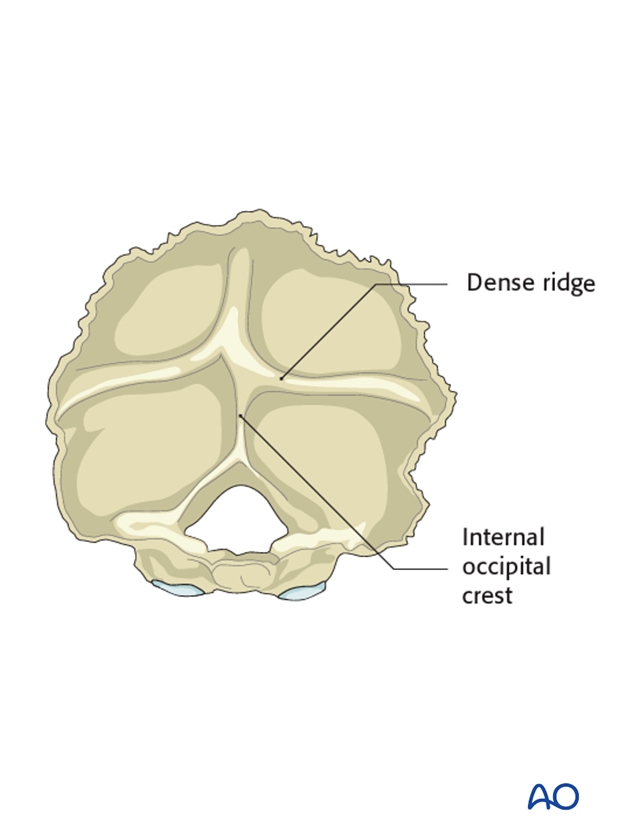
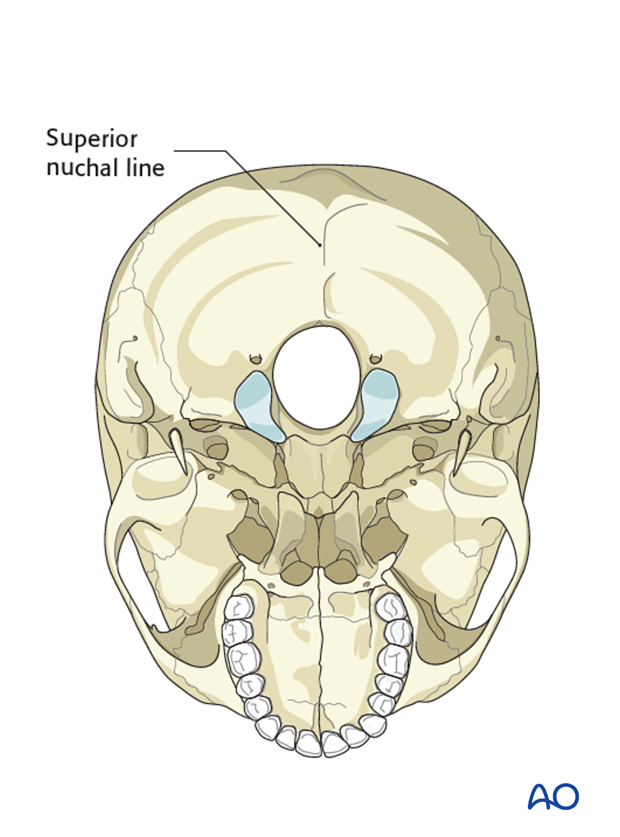
Another landmark with thicker bone is the superior nuchal line which runs horizontally.
4. Decompression
Timing of decompression
A patient who is experiencing neurologic deficit from solid tumor ESCC resulting in loss in ability to ambulate, in the absence of medical and oncological contraindications, requires urgent surgical decompression.
Expeditious diagnosis and prompt surgery are recommended to improve the probability of neurological recovery.
Use of dexamethasone
Administration of dexamethasone (10 mg bolus, 4 mg every 6 hours) is recommended as soon as ESCC causing neurologic deficit is diagnosed. Dexamethasone should be stopped or tapered as soon as spinal cord decompression is completed.
Neurological evaluation
The preoperative neurological assessment must be carried out as described in the Neurological Evaluation.
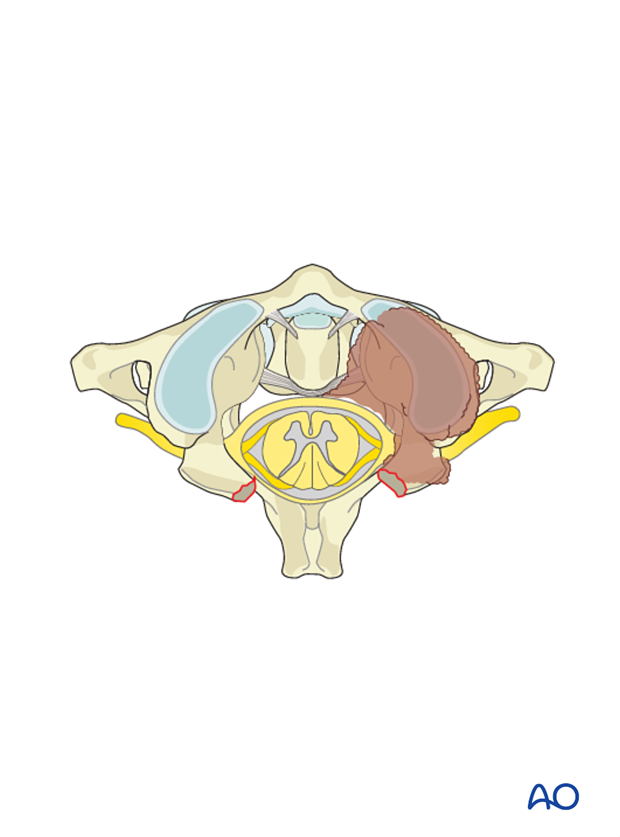
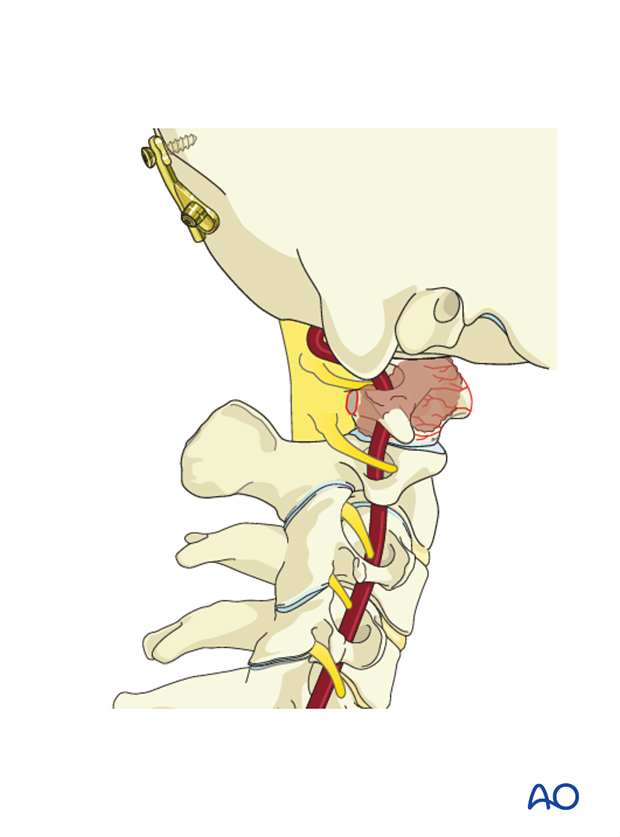
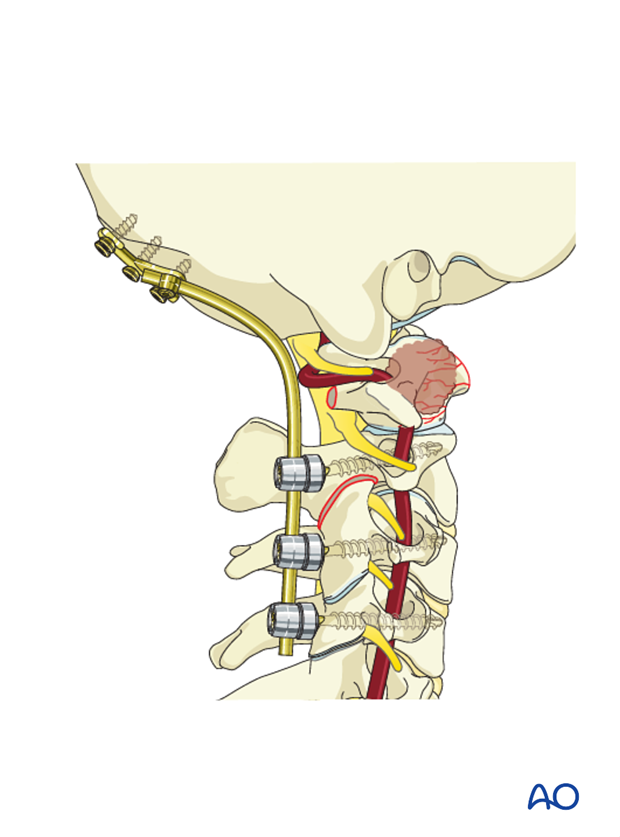
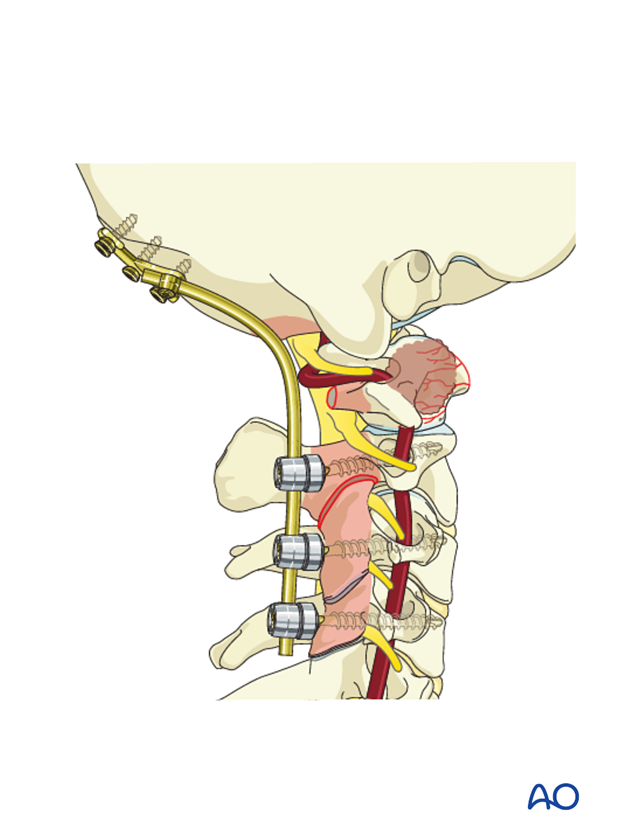
The posterior arch of C1 is removed together with the epidural tumor.
The intervening ligamentum flavum is excised.
Based on preoperative planning, the amount of posterior arch to be removed to achieve enough decompression can be determined beforehand.
The nerve root should be decompressed as well in order to avoid occipital neuralgia.
The spinal cord, dura and tumor should otherwise be manipulated as little as possible.
5. Plate application
The midline of the posterior aspect of the skull which is in line with the EOP is identified.
The plate is placed centered in the midline on the posterior aspect of the occiput. This allows for optimal placement, sizing and shape of the plate.
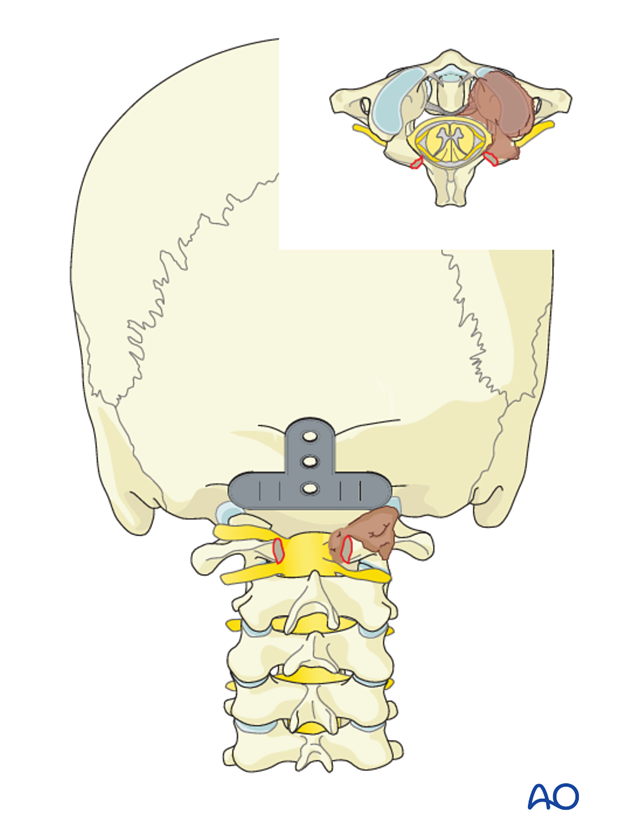
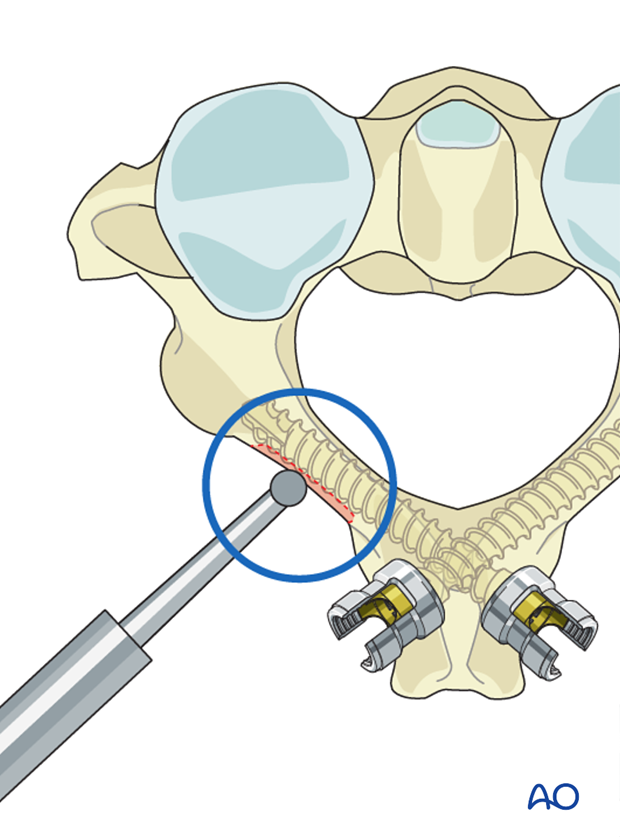
Once the optimal plate is chosen, the location of the central cranial screw entry point is marked with the plate in place.
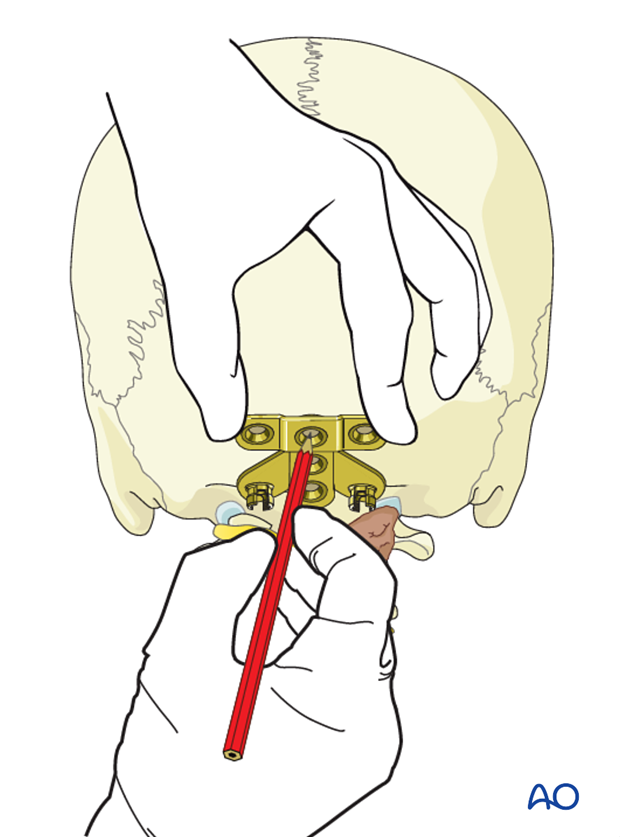
The drill guide is set to 8 mm (female) or 10 mm (male) and the central cranial screw hole drilled.

The screw hole is probed to verify that the anterior cortex is still intact.
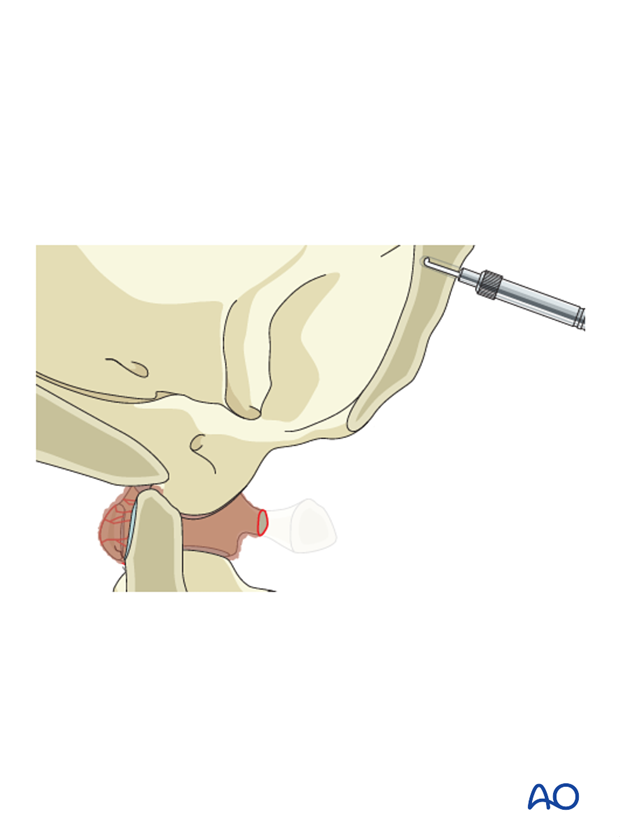
If intact, additional drilling in 2 mm increments is performed until the anterior cortex is penetrated.
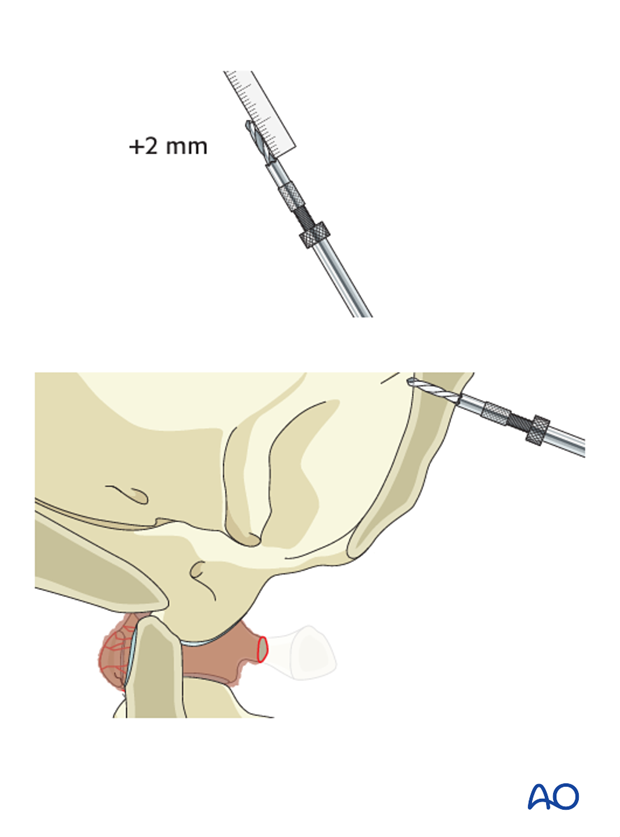
A screw of appropriate length is inserted through the plate into the predrilled hole.
After insertion of the first screw, there is enough flexibility in the system to allow for adjustments. Ensure the plate is flush with the skull and that it is level.
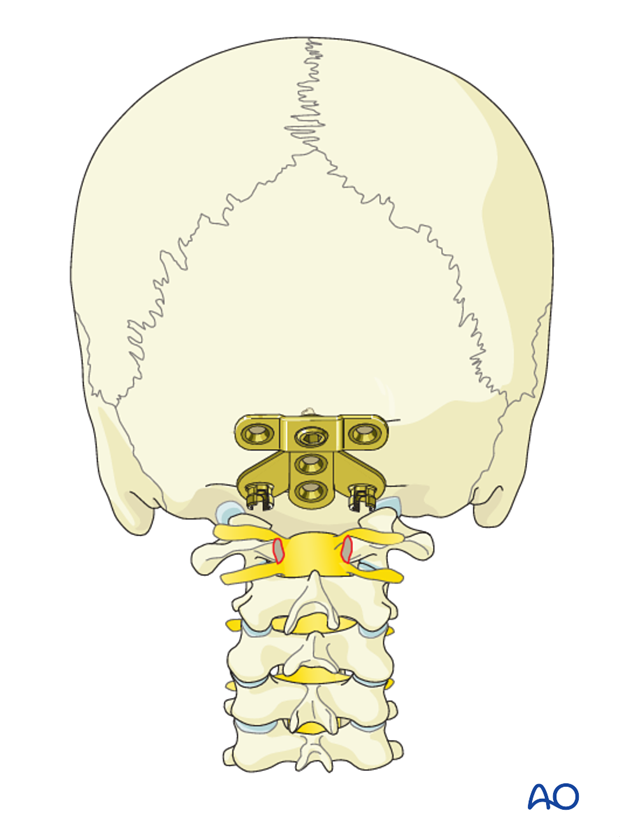
The remaining screws are then inserted with the same drill technique as for the first screw ensuring bicortical purchase in the order 2-5.
However, care is taken during drilling of the lateral holes (2 and 3) as the bone will be thinner than in the midline (4 and 5).
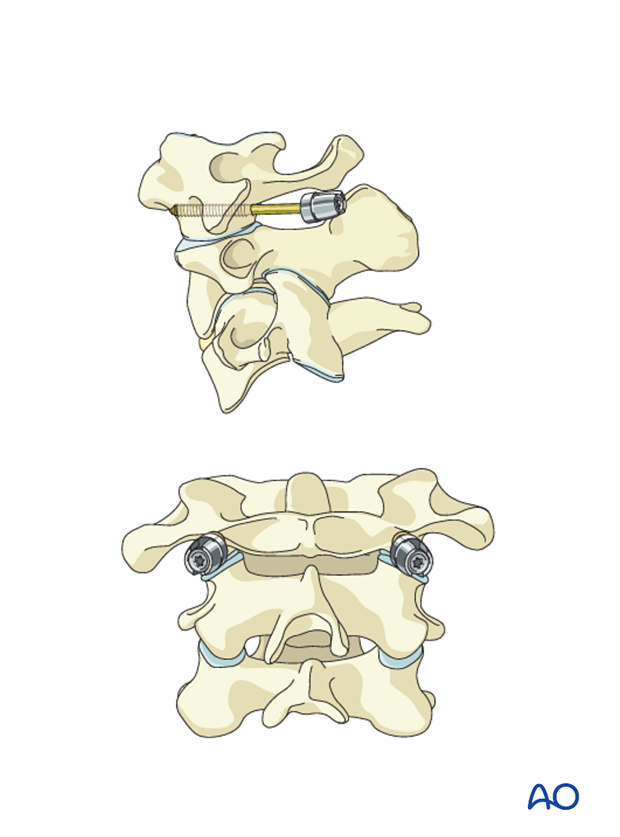
6. Cervical screw fixation
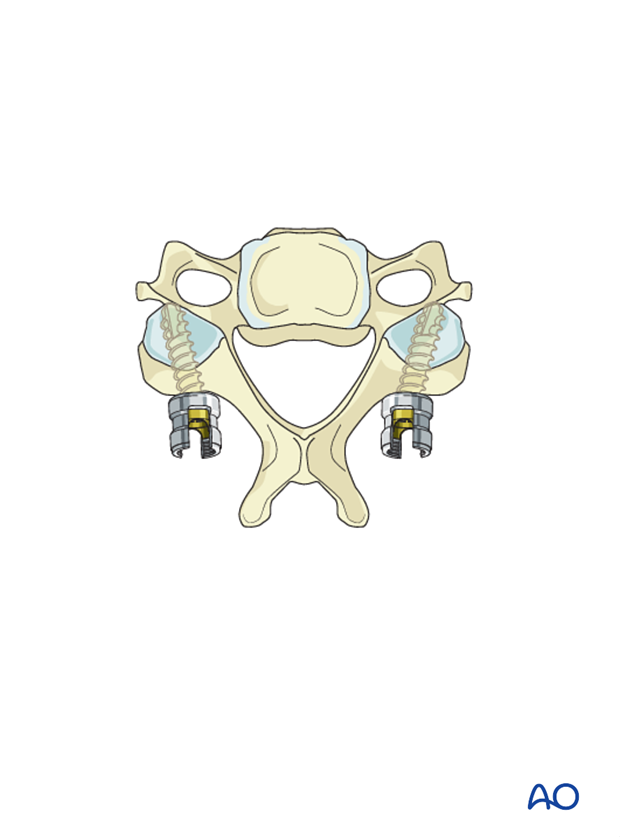
C1 fixation
The C1 level is rarely included in the instrumentation for C1 and C2 tumors.
However, an uncompromised lateral mass may be instrumented upon surgeon's preference.
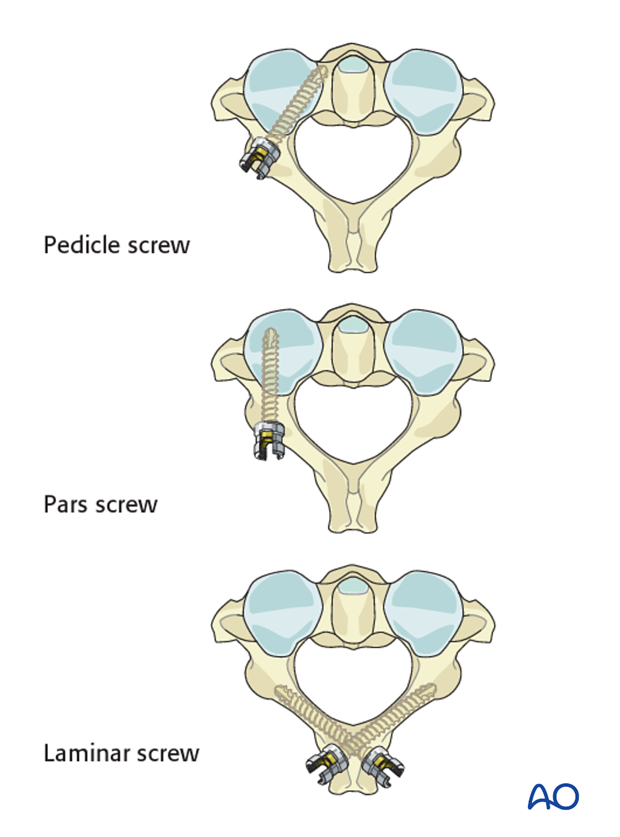
C2 fixation
For C1 tumors, C2 is instrumented bilaterally.
For C2 tumors, the C2 level is rarely included in the instrumentation. However, if the tumor is unilateral, the contralateral side may be instrumented upon surgeon's preference.
For C2 fixation the following options are available (in order of preference):
A consideration is given to use pedicle or laminar screws when doing an occiput to C2 fusion as oftentimes the starting point for the pars screws may compromise the facet joint.
C3 and C4 fixation
Two to three levels inferior to the tumor should be instrumented.
Fixation can be achieved with either lateral mass screws, pedicle screws or combination of the two.
Because lateral mass fixation is generally enough, and carries less risk, pedicle screw fixation is limited to rare cases where lateral mass fixation would be insufficient or not possible.
7. Alignment in the occipital cervical region
If there is a preoperative X-ray available, the surgeon can use this as a guide to properly align the occipito cervical junction during fusion. Ideally proper alignment allows for horizontal gaze.
8. Rod contouring
When the correct alignment is verified, the first rod is inserted. If no fusion is planned, the second rod is also inserted at this point.
9. Fusion
Indication for fusion
For patients with good prognosis and a long life-expectancy, posterior fusion may optionally be performed using allograft and/or local autograft.
Decortication
Decortication of lamina, facets, and posterior aspects of the skull is performed prior to placement of the final rod.
When using laminar screw fixation at C2, care must be taken not to decorticate deeply which might compromise screw fixation.
Second rod insertion
The second rod is inserted.
Bone grafting
Bone grafting material is placed against the decorticated elements of the spine.
10. Aftercare
Patients are made to sit up in the bed on the first day after surgery. Bracing is optional but preferably omitted for patient comfort. Patients with intact neurological status are made to stand and walk on the first day after surgery.
Patients can be discharged when medically stable or sent to a rehabilitation center if further care is necessary.
During admission adequate caloric intake of a high-quality diet should be monitored.
Patients are generally followed with periodical x-rays and (optionally) MR imaging at 6 weeks, 3 months, 6 months, and 1 year to monitor for tumor recurrence and hardware failure.
Postoperative radiation is required to avoid tumor recurrence. SBRT is usually initiated within two weeks following surgery. Conventional radiotherapy is usually initiated 2-4 weeks after surgery to reduce the risk of wound healing disturbances.
The radiation modality is selected based on tumor histology and history of prior radiation.













