Occipitocervical fusion IIC
1. Introduction
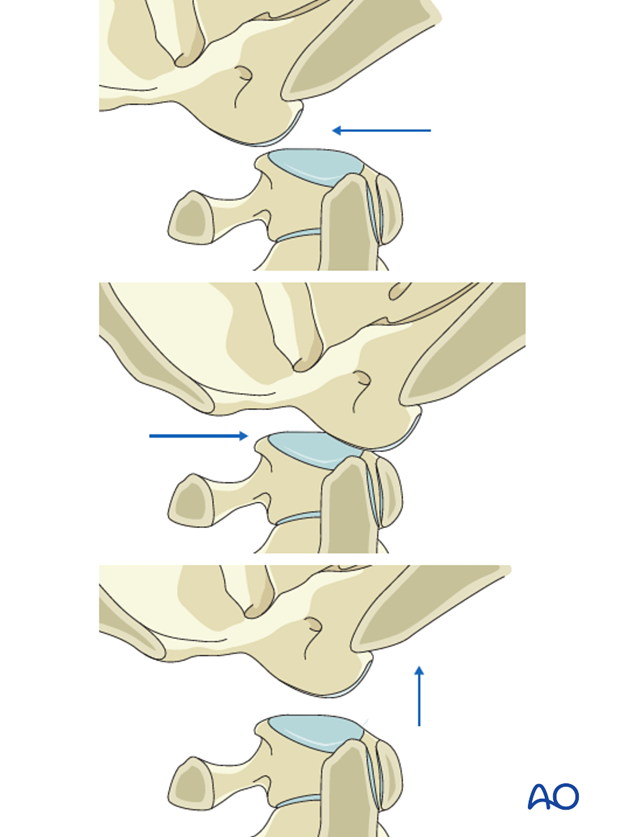
Atlanto-occipital dissociation is a highly unstable injury that is a life-threatening condition. It is produced by high-intensity trauma.
These are often polytrauma patients so this lesion may be missed during assessment. Once identified, immediate reduction and fixation are mandatory if the clinical condition allows surgery.
The following points are generally considered criteria for occipitocervical instability:
- > than 8° axial rotation to one side
- > than 1 mm Occ–C1 translation
2. Approach and positioning
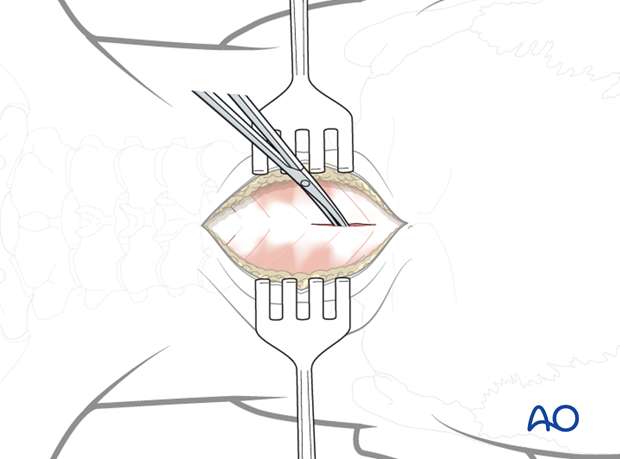
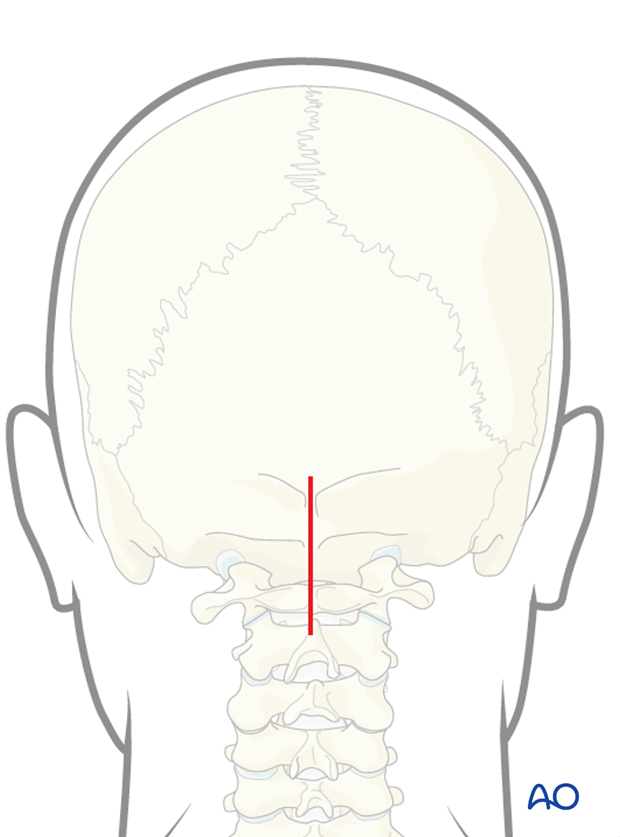
This procedure is performed through a posterior approach with the patient placed in the prone position.
3. Occipital fixation
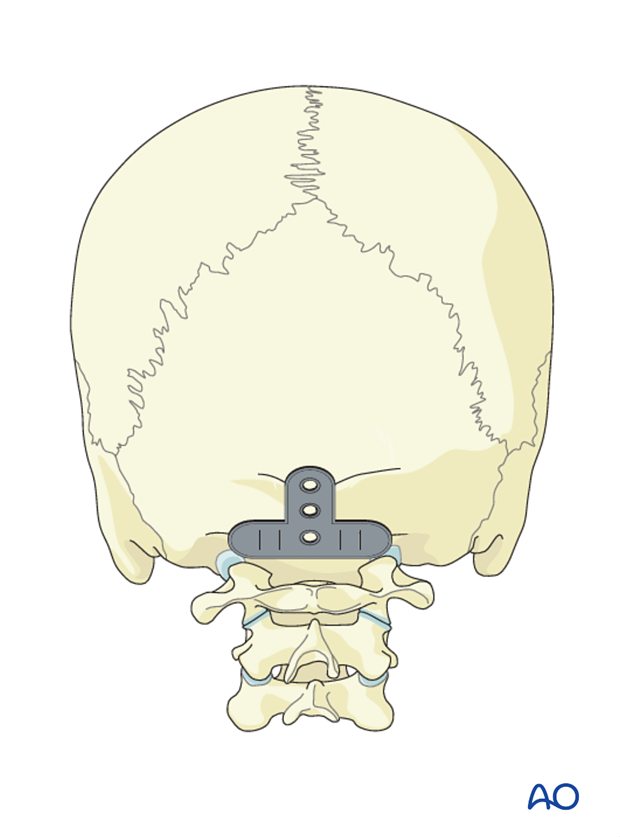
Occipital plate
There are several plate systems available for the occiput (an example is shown on the left). Their application is based on the same principles and to illustrate these concepts, we will show the use of a plate placed in the midline which allows for modularity and rotation when connecting to the rods.
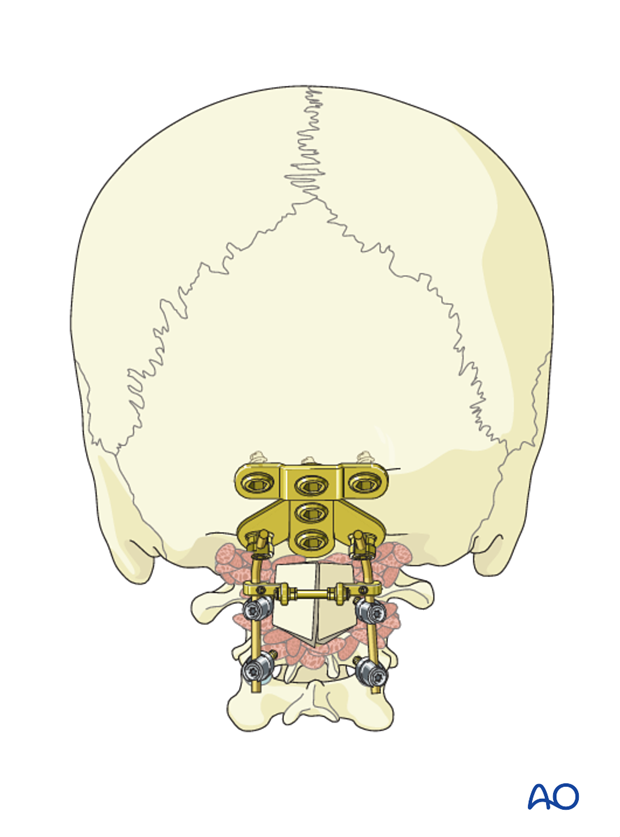
Plate placement
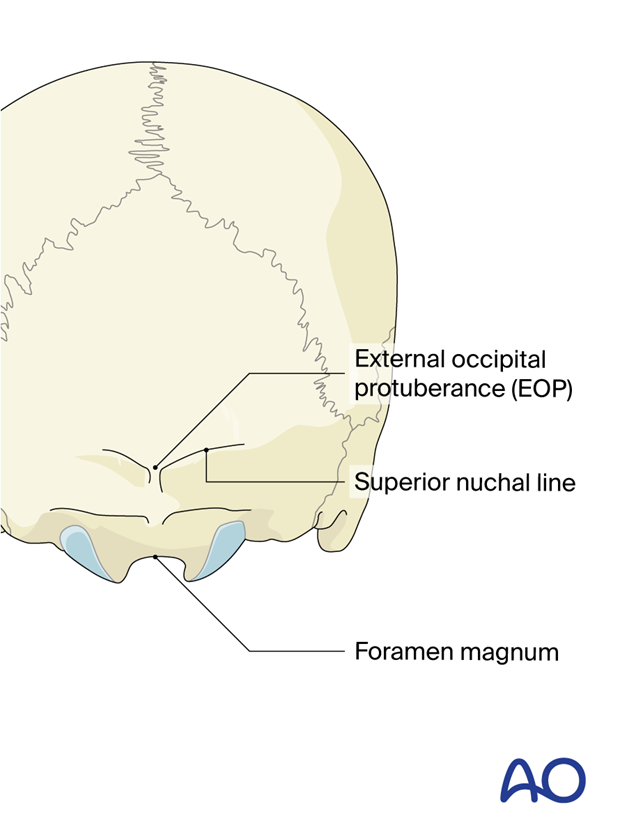
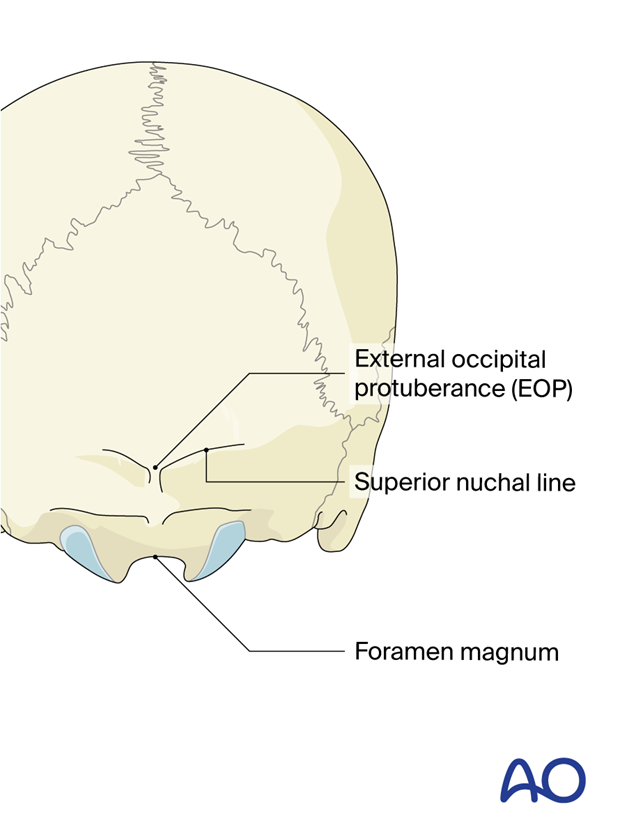
Irrespective of the plate system used, its placement should be close to but still caudal to the external occipital protuberance (EOP).
Placement of the plate at the EOP will increase the risk of erosion of the skin.
A too caudal position may compromise the foramen magnum.
Screw placement
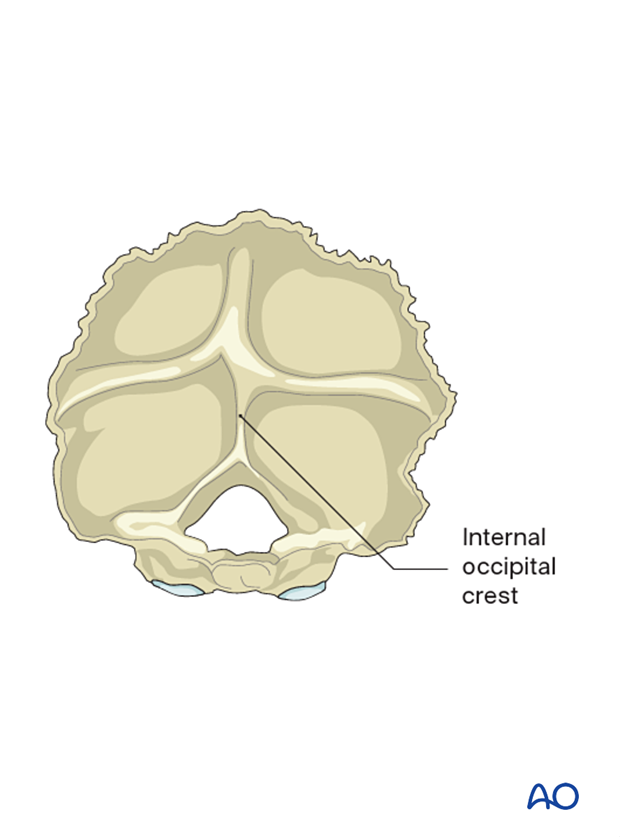
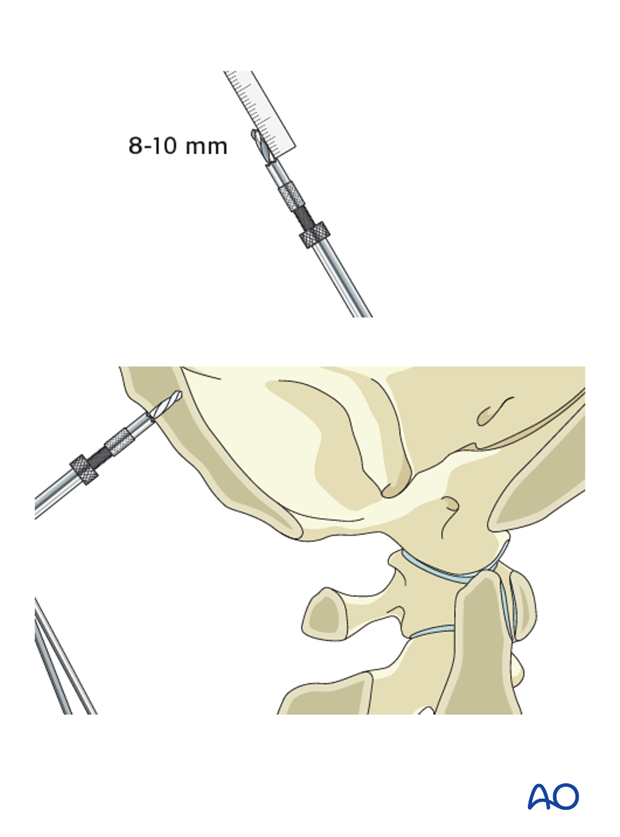
The thickest part of the cranium is the dense ridge which runs vertically in line with the internal occipital crest.
The thickness of this crest is 11.5–15 mm in males and 10–12 mm in females and provides the best bone stock for screw purchase.
As you move laterally this crest becomes thinner and around 7–8 mm lateral to the midline, the bone thins out to a thickness of only 5–6 mm.
The illustration shows the internal part of the occipital bone.
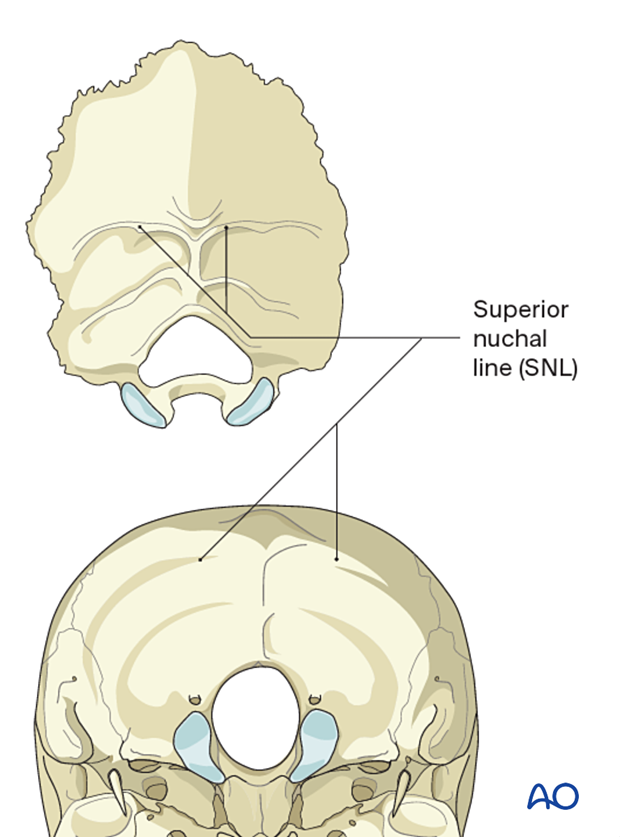
Another landmark with thicker bone is the superior nuchal line which runs horizontally.
An occipital condyle screw may provide added stability in cases where additional occipital or skull fixation is needed (skull fracture).

4. Plate application
Preparation of plating site
The occiput bone is dissected up to the external EOP and laterally as far as needed to accommodate the plate.
Landmarks
The following landmarks are identified:
- EOP
- Superior nuchal line
- Caudal aspect of the occiput (foramen magnum)
The midline of the posterior aspect of the skull which is in line with the EOP is identified.
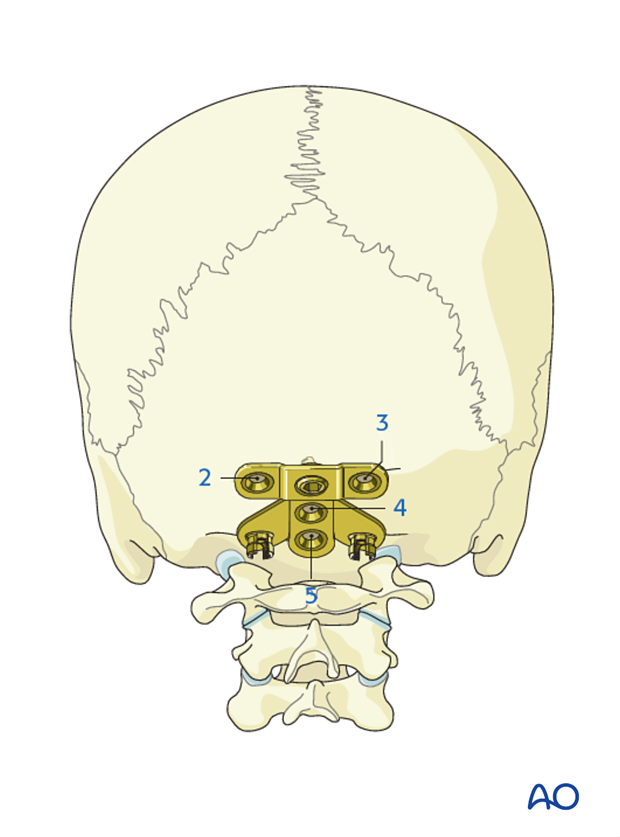
The plate is placed centered in the midline on the posterior aspect of the occiput.
Once the optimal plate is chosen, the location of the central cranial screw entry point is marked with the plate in place.
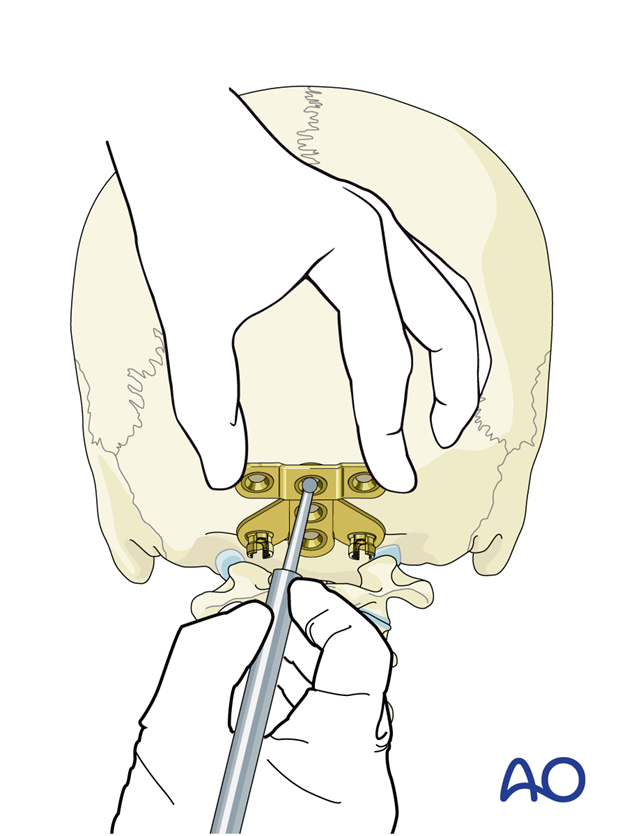
The drill guide is set to 8 mm (female), or 10 mm (male) and the central cranial screw hole is drilled.
The screw hole is palpated to verify that the anterior cortex is still intact.
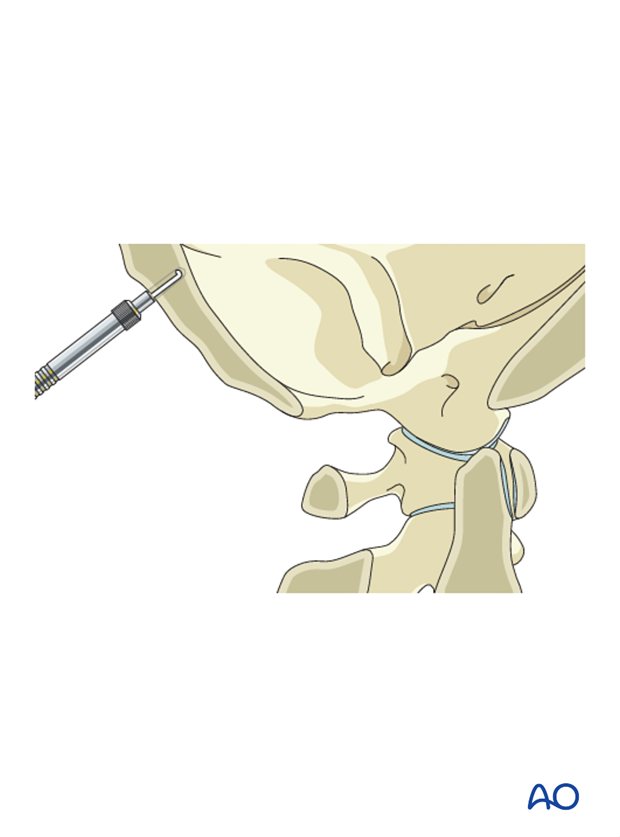
If intact, additional drilling in 2 mm increments is performed until the anterior cortex is penetrated.
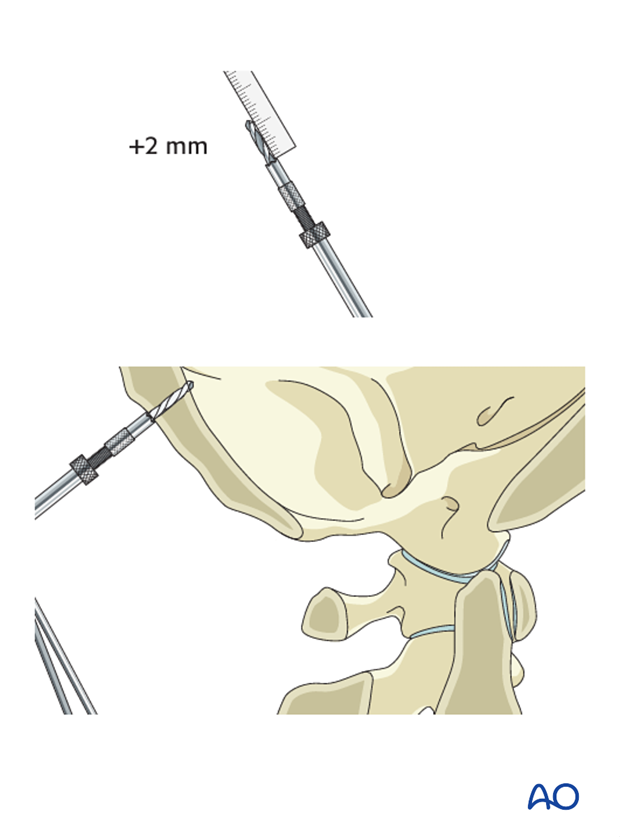
A screw of appropriate length is inserted through the plate into the predrilled hole.
After insertion of the first screw, there is enough flexibility in the system to allow for adjustments. Ensure the plate is flush with the skull and that it is level.

The remaining screws are then inserted with the same drill technique as for the first screw, ensuring bicortical purchase in the order 2–5.
However, care is taken during drilling of the lateral holes (2 and 3) as the bone will be thinner than in the midline (4 and 5).
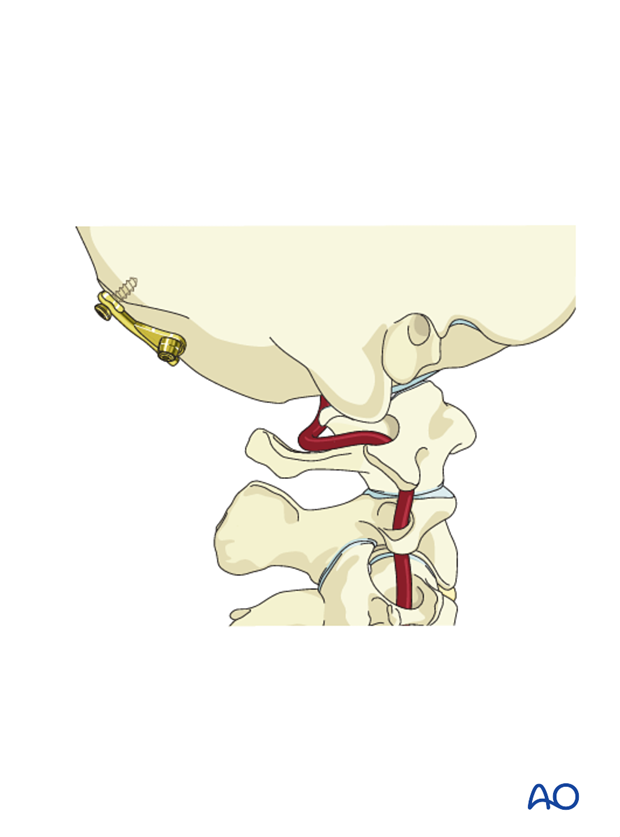
When additional occipital or skull fixation is needed, an occipital condyle screw is now inserted.
5. Cervical screw fixation
C1 fixation
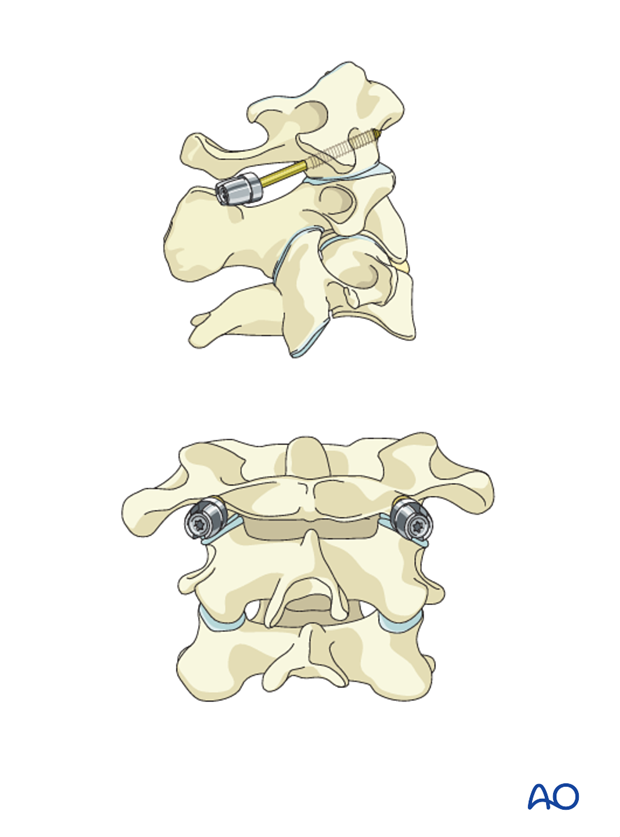
For C1 fixation, C1 lateral mass screws can be used.
C2 fixation
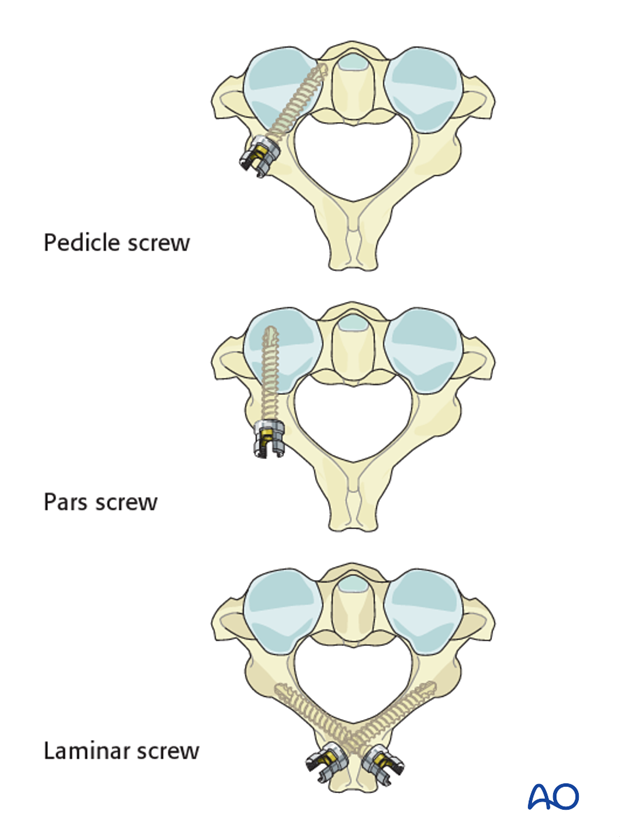
For C2 fixation the following options are available:
Consideration is given to using pedicle or interlaminar screws when doing an occiput to C2 fusion as often the starting point for the pars screws may compromise the facet joint.
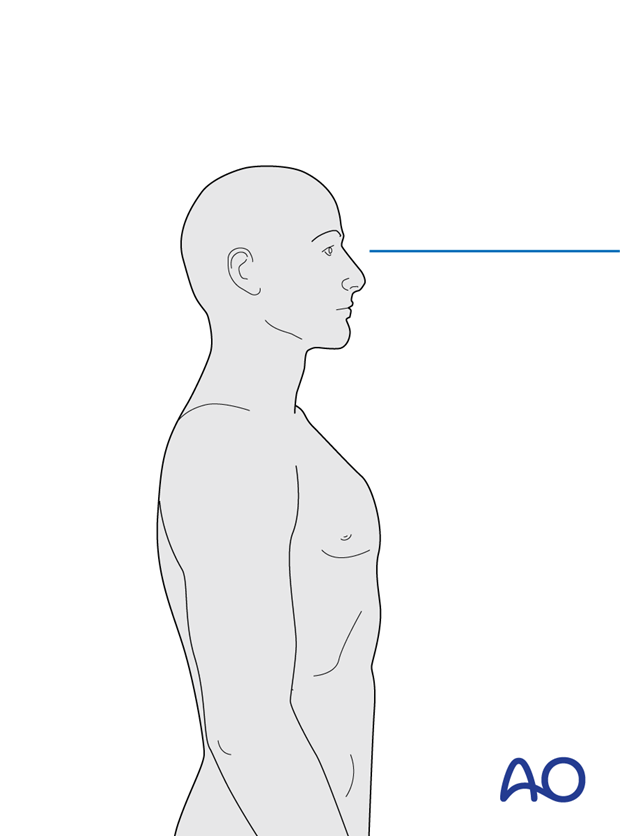
6. Alignment in the occipitocervical region
The preoperative x-ray should be used by the surgeon as a guide to properly align the occipitocervical junction during fusion. Align the head to allow for a horizontal gaze once the fusion is complete. Bend the rod accordingly.
Use the preoperative x-ray as a guide to properly align the occipitocervical junction during fusion.
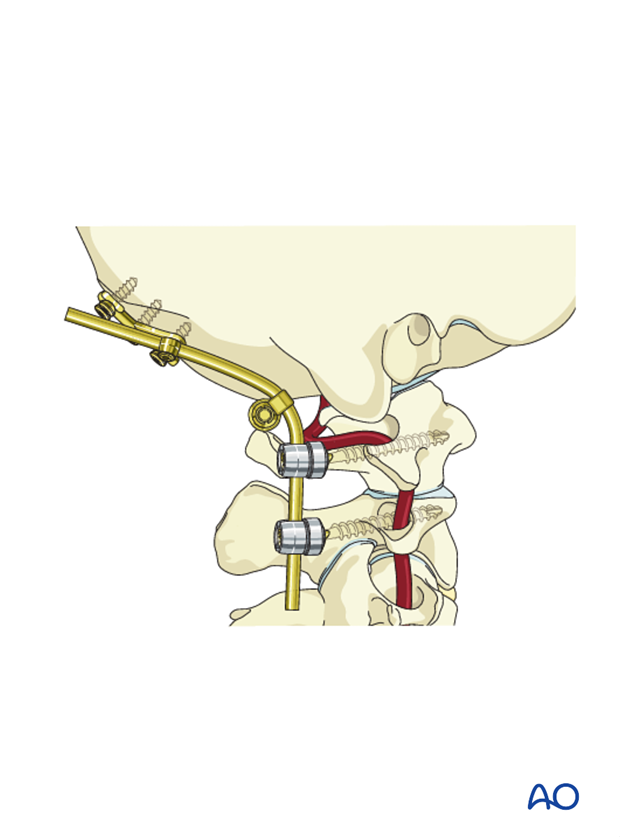
7. Rod contouring
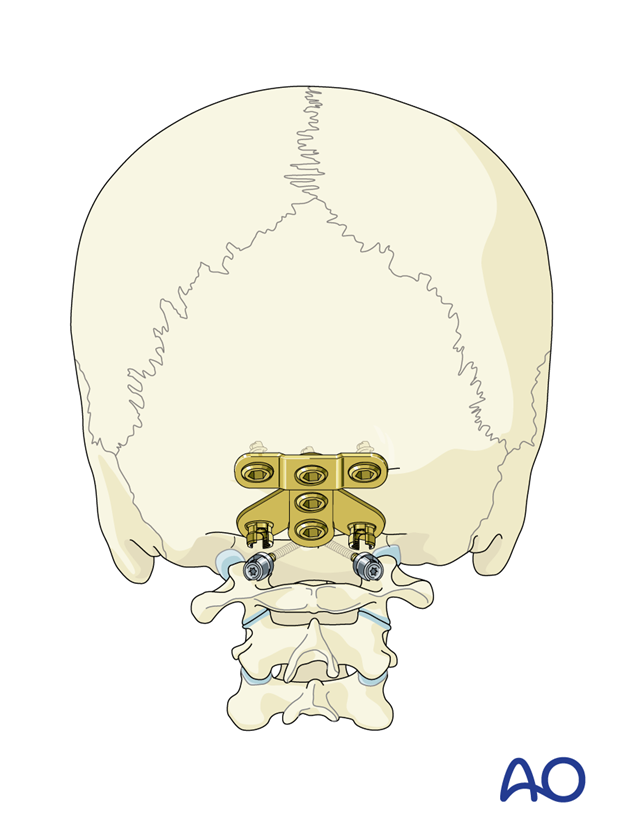
When the correct alignment is verified, rods are temporarily placed.
Some systems have the advantage of rods with a ball point which allow for easier placement and contouring of the occipitocervical region (which can be relatively difficult when bending straight rods to the proper shape). If these rod-screw systems are not available a standard rod can be bent.
8. Decortication
Prior to final placement of the rods, decortication of lamina, facets, and posterior aspects of the skull is performed.
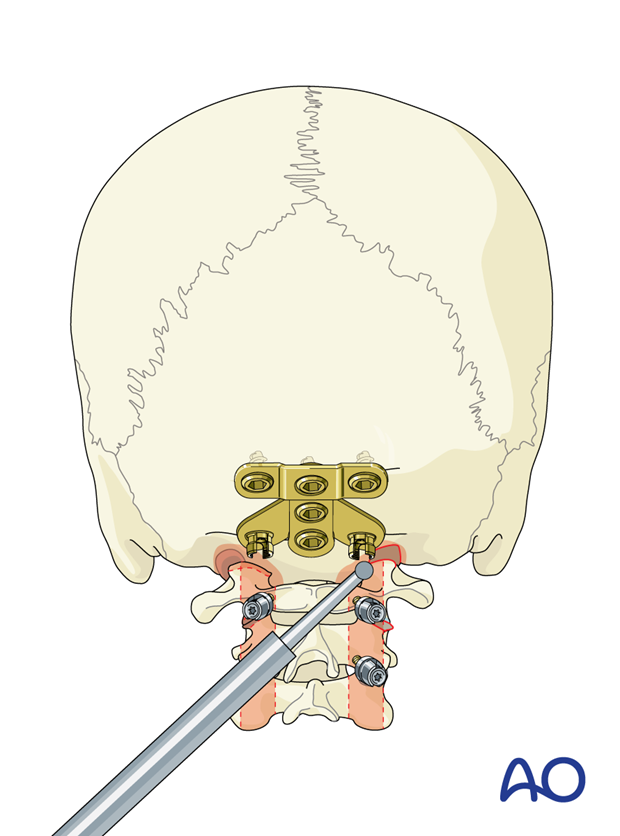
When using intralaminar screw fixation at C2, care must be taken not to decorticate deeply, as this may compromise screw fixation.

9. Fusion
Rod insertion
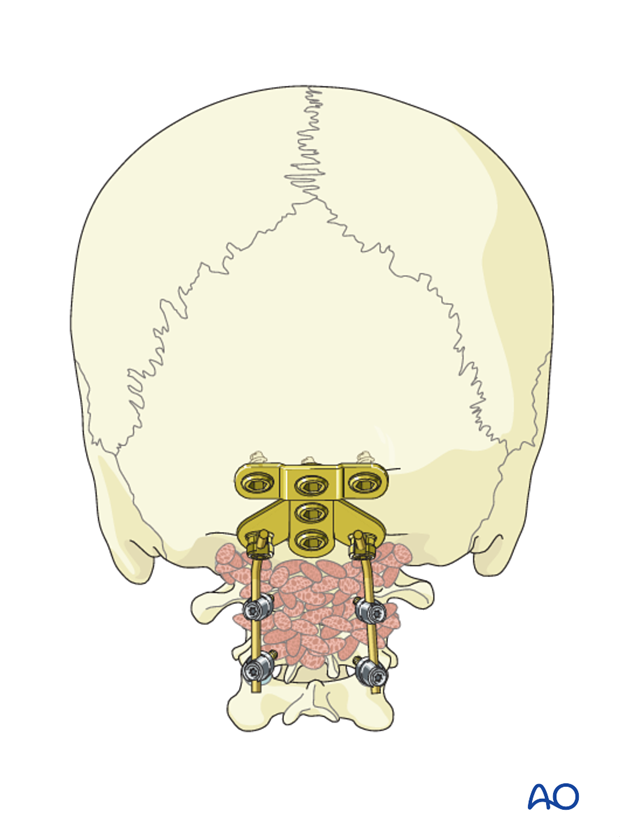
Ensure that alignment is correct. Then insert the rods.

Bone grafting
There are several options for bone grafting material including:
- Autograft (iliac crest cancellous bone)
- Allograft (cortico-cancellous or cortical onlay graft)
- Local bone
- Various biomaterials
The grafting material is placed against the decorticated bone.
10. Aftercare
Patients are made to sit up in bed on the evening following the operation.
A collar may be used following surgical stabilization to moderate patient activity.
Patients with intact neurological status are made to stand and walk on the first day after surgery. Patients can be discharged when medically stable or sent to a rehabilitation center if further care is necessary. This depends on the comfort levels and presence of other associated injuries.
Patients are generally followed with periodical x-rays at 6 weeks, 3 months, 6 months, and 1 year.













