ORIF - Lag screw with plate fixation
1. Principles
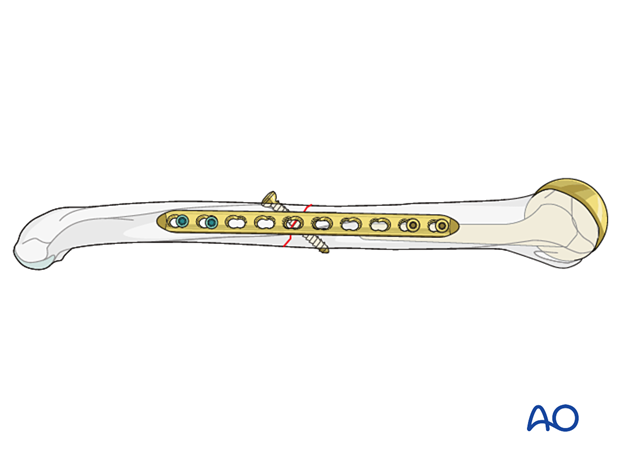
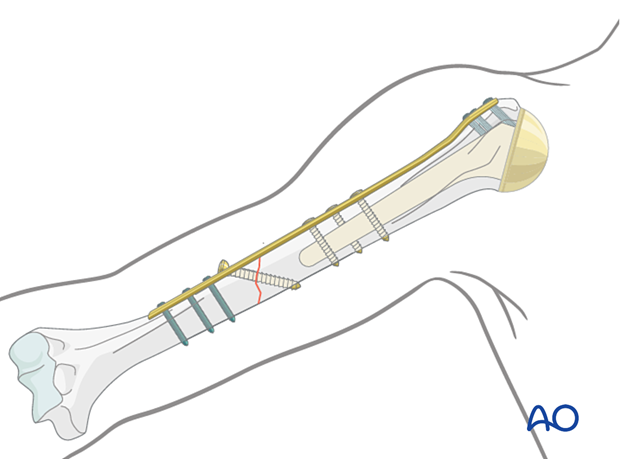
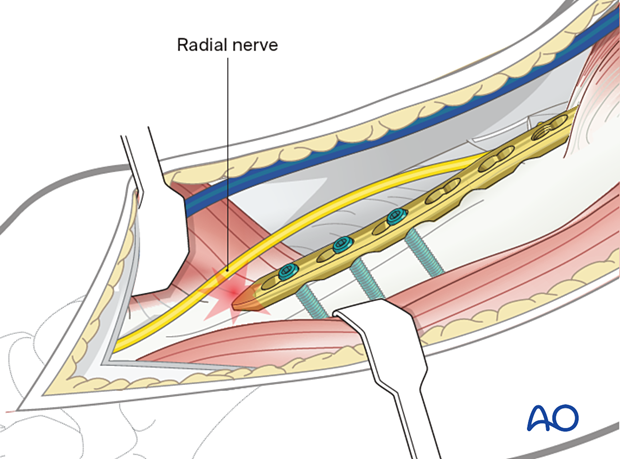
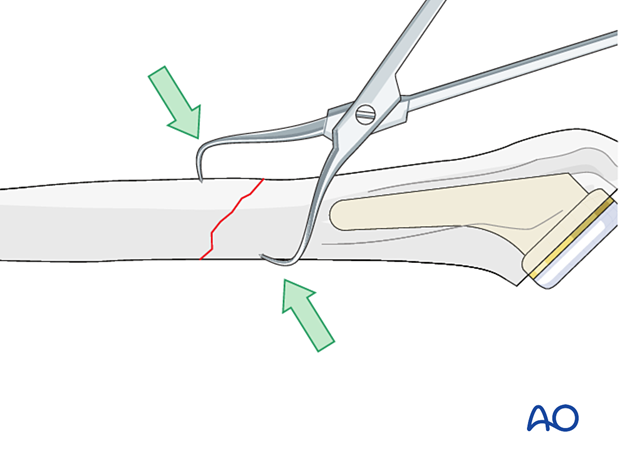
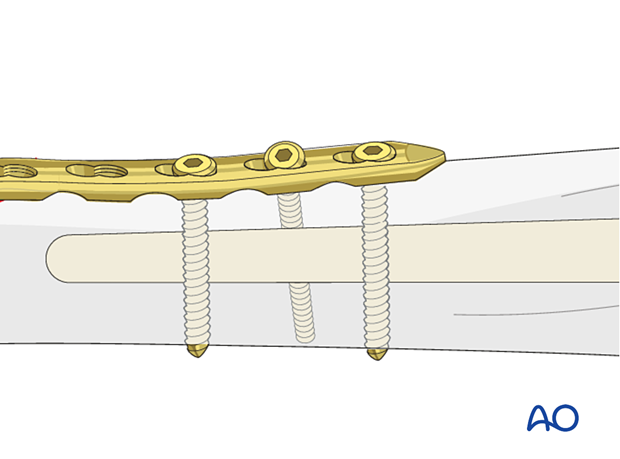
Lag screw with protection plate
A lag screw or screws is/are used to fix spiral or long oblique fractures. A plate is used in neutralization (protection) mode to protect the construct. An example of a completed construct is shown in this illustration.
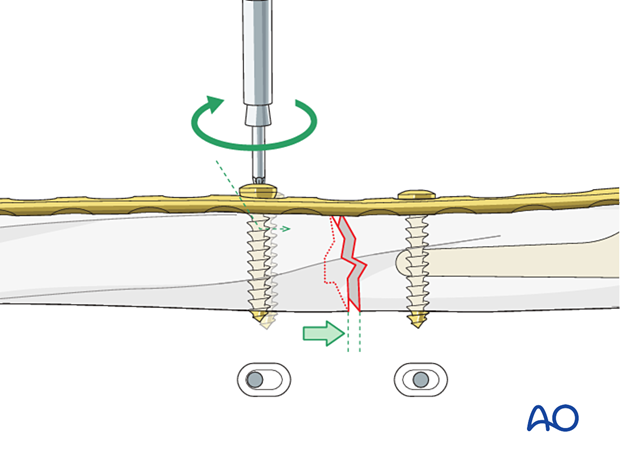
Compression plate
A lag screw cannot be inserted in transverse or short oblique fractures. Interfragmentary compression can be achieved by:
- Eccentric screw positioning in a locking compression plate (LCP)
- Using a dynamic compression plate (DCP)
Further details about the general principles of compression plating can be found in the Plating basic technique.
2. Choice of implant
Plate types
The following plate types may be used depending on the fracture location or configuration:
- Standard plate 3.5 mm or 4.5 mm system
- Plate with locking head screws (LCP)
- Anatomically pre-contoured plate
- Extraarticular distal humerus plate
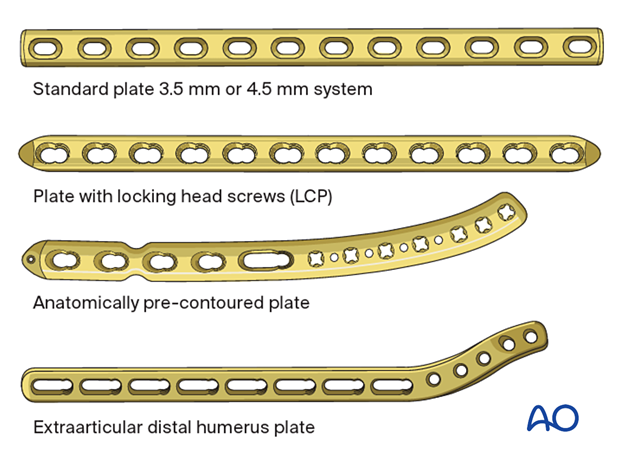
Plate length
A plate that is long enough to achieve balanced fixation is used.
The technique of fixation proximal to the fracture is determined by the humeral prosthetic stem. Screw fixation proximal to the fracture may be relatively less secure than distal to the fracture. Supplementary fixation proximal to the fracture, for example with cerclage wires, may be required. The plate should be long enough to accommodate multiple points of fixation proximal to the fracture to balance the likely better screw fixation in bone distal to the fracture.
Important factors for fixation stability include:
- Plate length
- Distribution of screws or fixation points
- Number of screws or fixation points
- Bone quality
Sometimes using a longer plate that reaches the greater tuberosity region can aid insertion of proximal screws as more bone stock for screw fixation is available there.
3. Plate position
Introduction
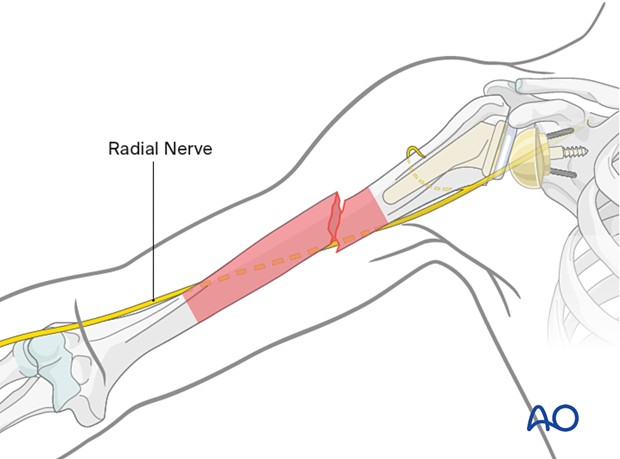
The choice of plate position depends on the fracture morphology and location and is influenced by the presence of radial nerve pathology. The anterolateral, anterior, and posterior surfaces of the humeral shaft are all possible choices.
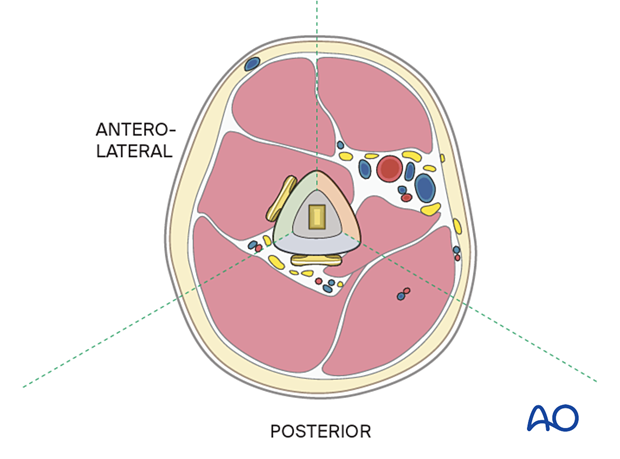
Anterolateral or anterior plate
An anterolateral plate fits well from very proximally to the distal fifth of the humerus and can be selected if proximal and middle third fractures are present.
A plate in this position should provide stable fixation of the fracture and minimal soft-tissue damage.
Proximally, the plate may interfere with the deltoid insertion if it is placed laterally. To overcome this problem the proximal end of the plate can be tunneled through the deltoid insertion.
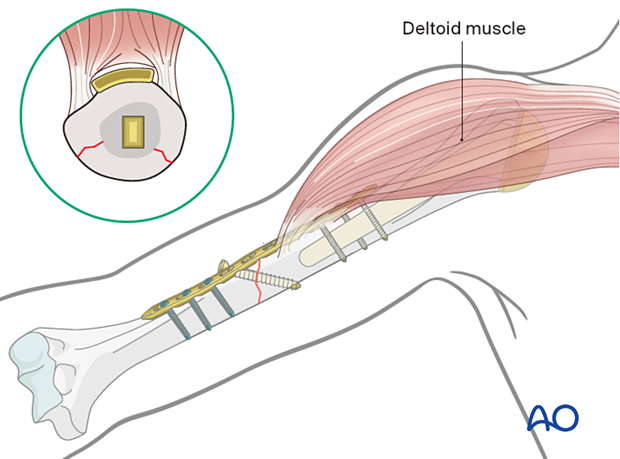
Distally the plate may be applied to the anterior or lateral surface.
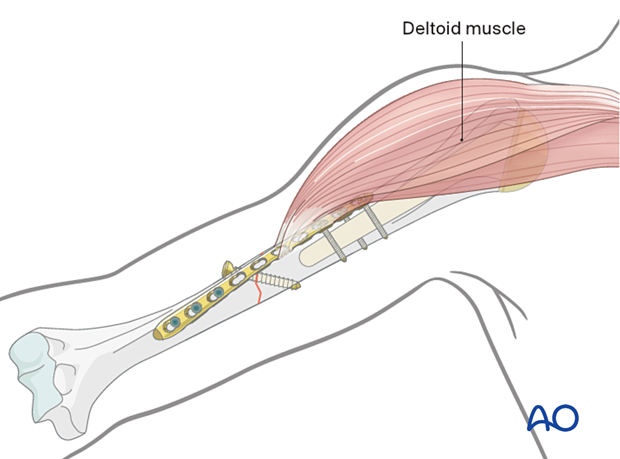
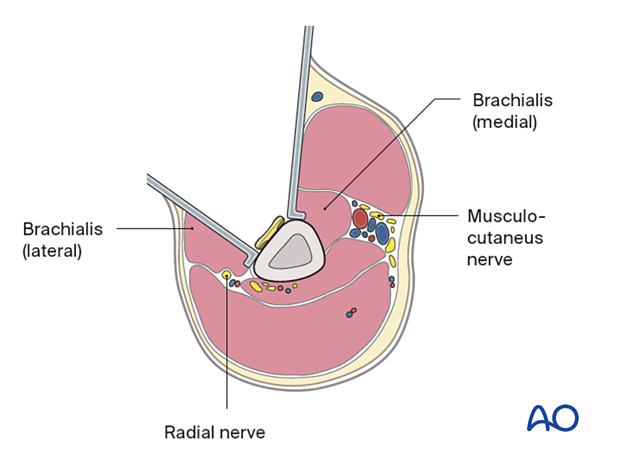
The innervation of the brachialis muscle is derived from both the radial and musculocutaneous nerves. The radial branch is at risk if the plate is applied to the anterior and anterolateral surfaces in the distal third of the humerus while retracting the entire brachialis muscle medially. To avoid this, it is safer to split the brachialis muscle.
Posterior plate
The posterior surface is difficult to access proximally and limited by the axillary nerve. Therefore, posterior plating is best suited for middle and distal third fractures of the humerus.
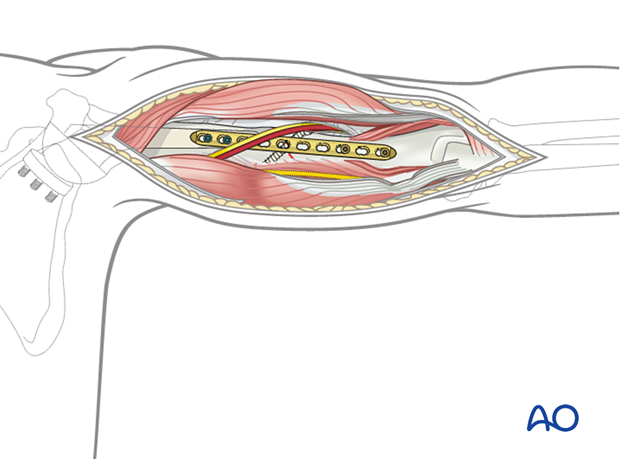
It is important to protect the radial nerve and its accompanying vessels in the spiral groove. If the plate interferes with the radial nerve, the plate must be placed underneath it.
4. Patient preparation and approaches
Patient positioning
Place the patient in a beach chair position at 30°. The arm is supported on a side table.
For more distal fractures, the patient is placed in a lateral decubitus position. A prone position can also be used.
Patient positioning should be discussed with the anesthetist.
Approaches
The approach is selected depending on the chosen plate position.
For an anterolateral plate a deltopectoral approach with extension may be used.
The posterior surface can be accessed with a posterior humeral approach.
5. Reduction
Standard reduction techniques of the humerus are provided in the Surgery Reference adult trauma Humeral shaft module.
6. Plate fixation
Where possible, standard plate and screw fixation techniques are used.
In the peri-implant area standard screw application may be jeopardized by the presence of the stem. In this situation, the following techniques may be used:
- Off-axis screws on either side of the implant
- Unicortical screws with cerclage cables/wires
- Locking attachment plate
Further details on peri-implant plate fixation are provided here.
7. Aftercare
Postoperative phases
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.













