Plating
1. Introduction
Plating modalities
Plates may be applied in various modes according to the function required. These include:
- Protection (neutralization)
- Compression
- Bridging
- Buttress (antiglide)
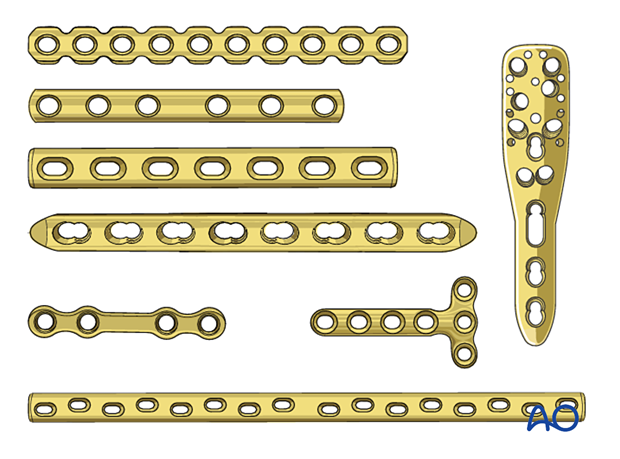
Plate designs
Various plate designs are available. These may be larger or smaller, thicker or thinner, as appropriate to various anatomic sites and the loads to which they will be subjected.
The holes in the plate may be designed for locking screws, non-locking screws, or either, and designed to facilitate dynamic compression.
Some plates are designed to have reduced contact area on the bone.
Reconstruction plates are designed to be easier to contour in complex anatomic locations.
There are plates designed for many specific anatomic locations.
These 3D models show the effect of different plate designs on bending stiffness.
Increased width is shown in the top panel, a normal plate is shown in the center panel, and increased thickness is shown in the bottom panel. Out of these, the thickness of the plate is the most influential parameter for bending strength.
Plate contouring
The plate must fit the shape of the bone. The midshaft of many long bones is straight so plates applied to these regions may not need to be contoured.
Most bones show a flare towards the metaphysis, so plates applied in these regions usually need to be contoured.
The use of a flexible template can facilitate plate contouring.
Where locking screws are used, the bone-plate construct remains stable even if the plate is not in direct contact with the bone. Therefore, contouring does not need to be so accurate.
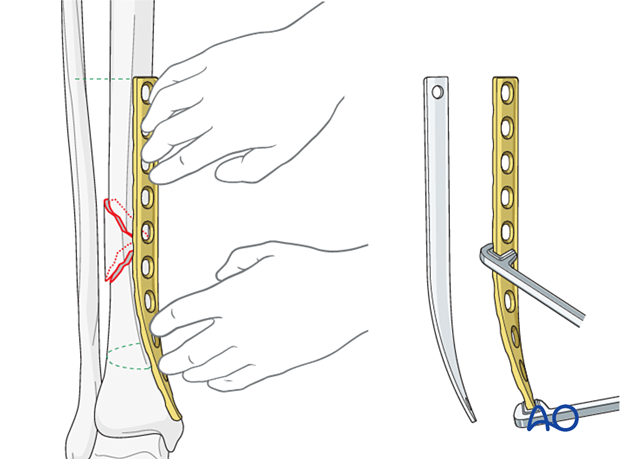
Anatomic plates are pre-contoured to fit the region they are designed for. Be aware that plates are designed from data taken from a normally-distributed population of subjects, and they may need to be adjusted to fit individual patients.
2. Protection (neutralization) plates
Function
A protection plate neutralizes bending and rotational forces to protect a lag screw fixation.
This is equally true of plates with locking or non-locking screws.
Application
Reduce the fracture and fix it with one or more lag screws.
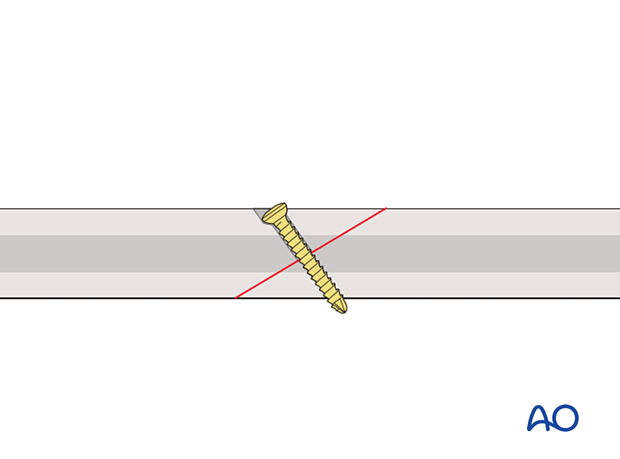
This 3D model shows application of a lag screw.
A lag screw placed perpendicular to the fracture plane is used to achieve optimal compression of fracture surfaces in a simple fracture. If this optimal orientation is not achieved, then a malreduction will be induced. Lag screws can provide useful compression to enhance fracture plane contact and hence healing, but the fracture plane is not stable when a bending or torsional force is applied. Resistance to bending or torsional forces is provided by a neutralization (protection) plate.
The appropriately contoured plate is applied to the bone, and screws inserted in a neutral mode.
Depending on plate design, bone quality, implant availability, and surgeon’s preference, fixed angle locking head screws, variable angle locking head screws, or non-locking screws may be inserted.
It is not necessary to fill every hole in the plate with screws, as long as enough screws are inserted to obtain sufficient hold and maintain the reduction until the fracture heals.
This 3D model shows a lag screw with a neutralization plate fixed in an orthogonal orientation to the screw.
By placing the neutralization plate in a plane rotated 90° to the plane of the lag screw, torsion and bending forces acting on the screw are reduced. The overall stability of the construct is increased.
3. Compression plates
Function
The plate produces compression at the fracture site to provide absolute stability.
Application (transverse fractures)
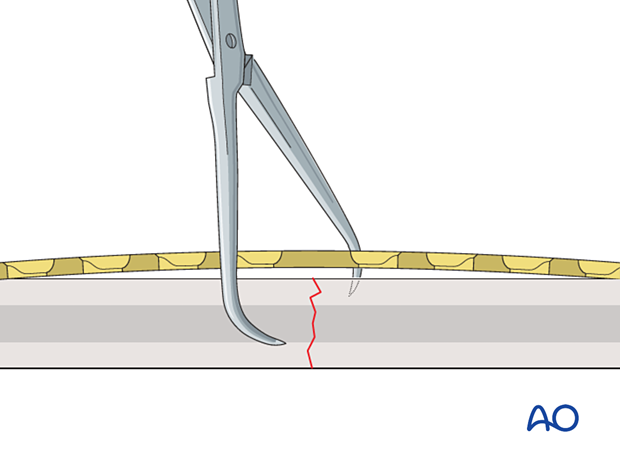
ReductionIf possible, the fracture is reduced and temporarily fixed with forceps. Place the forceps so they will not interfere with the planned plate position.
If the plate is exactly contoured to the anatomically reduced fracture surface, there will be some gapping of the far cortex when the plate is tensioned by tightening the load screw.
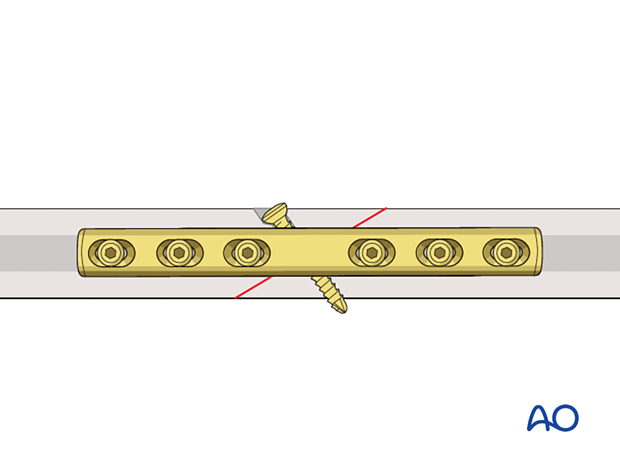
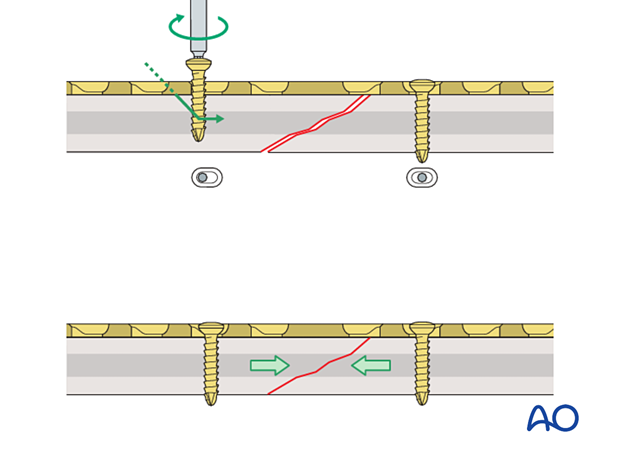
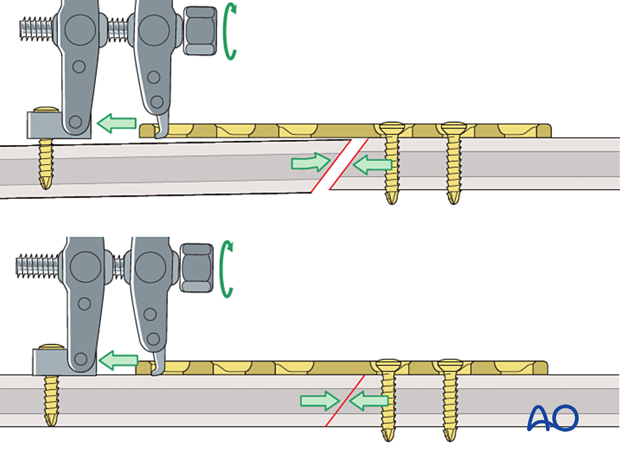
This 3D model shows a screw inserted in compression mode with an unbent plate.
When a transverse fracture is compressed with a plate that is not overbent but exactly pre-contoured to the reduced fracture surface (bottom panel), compression will first be exerted at the cortex under the plate (near cortex). The cortex opposite the plate (far cortex) will open resulting in a fracture gap. This may lead to delayed union of the far cortex.
The solution to this problem is to “overbend” the plate so that its center stands off 1–2 mm from the anatomically reduced fracture surface.
The overbend should lie directly over the fracture line.
When the first screw is inserted, slight gapping of the cortex will occur directly underneath the plate. After fixation is complete, the plate will be in contact with the bone throughout its length, but will act as a spring, providing compression at the far cortex.
The prebent plate is fixed to one of the main fragments with a screw inserted in compression mode. Reduction forceps are placed on the opposite fragment to hold it in the reduced position against the plate. The screw is not fully tightened.
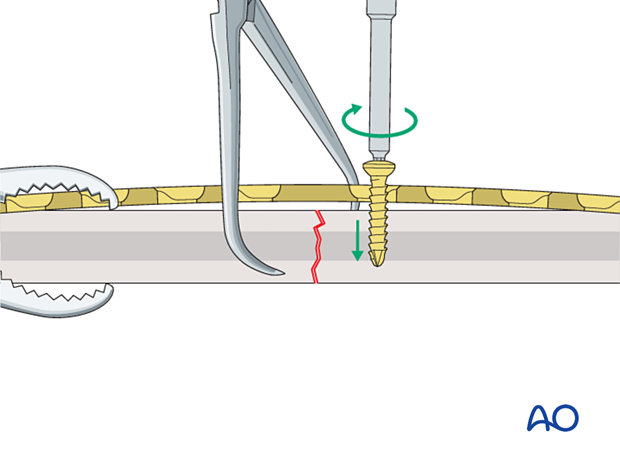
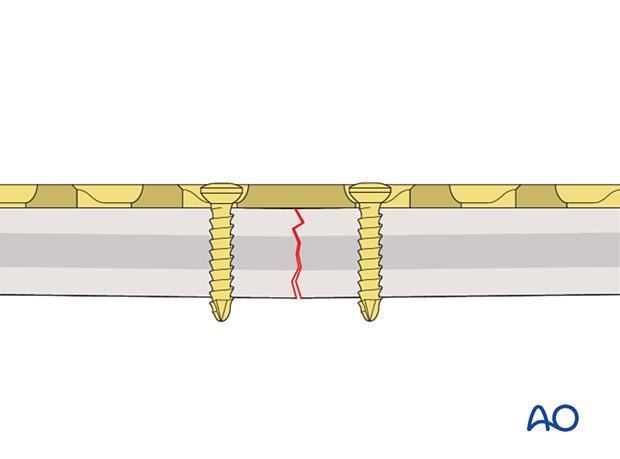
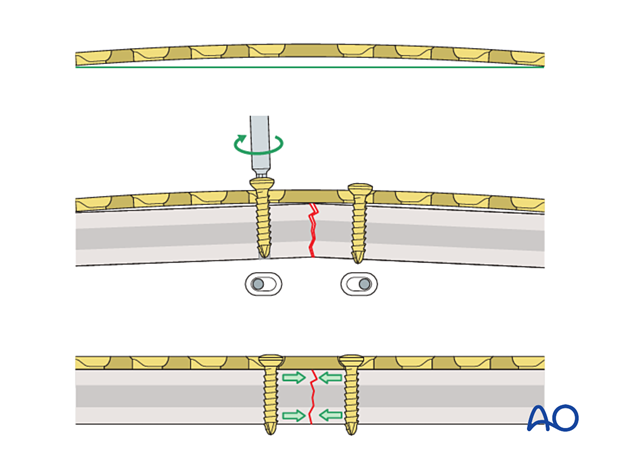
This 3D model shows screw insertion in compression mode with an overbent plate (Step 1).
To compress both the near and opposite (far) cortices, the plate should be slightly overbent before application, resulting in a convex shape, so there is a small gap between plate and bone at the fracture. Before the screws are inserted, the fracture is reduced. With the insertion of the first screw eccentrically in the screw hole, the overbent plate is pressed onto one bone fragment which causes slight displacement of the reduced fracture. The displaced fragment will be relocated with the insertion of the second screw in compression mode.
A screw is inserted in compression mode in the opposite fragment. To maintain reduction, it is recommended to tighten the screws gradually by alternating between the two sides.
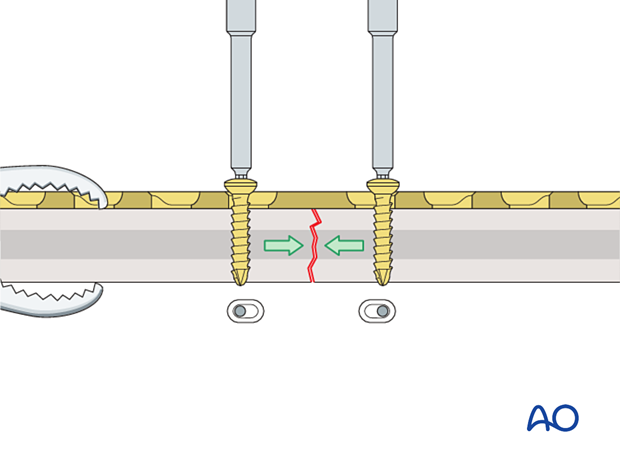
This 3D model shows screw insertion in compression mode with an overbent plate (Step 2).
The displaced fragment is reduced with the insertion of the second screw eccentrically in compression mode, straightening the plate and closing the gap at both the near and far cortices.
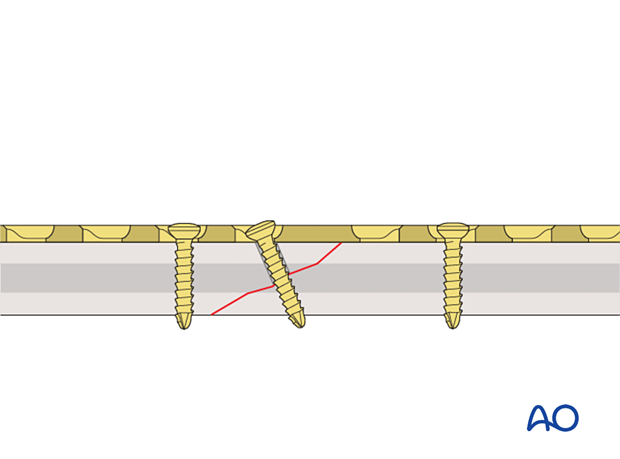
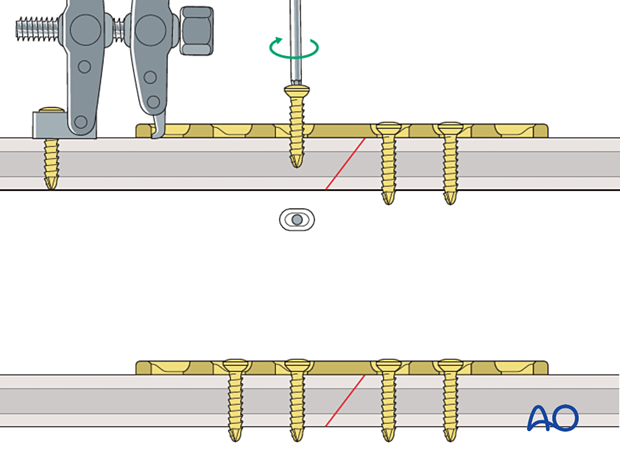
These 3D models show that locking head screws cannot be used for compression. The bottom panel shows that locking head screws cannot be inserted eccentrically in compression mode, unlike conventional screws (top panel).
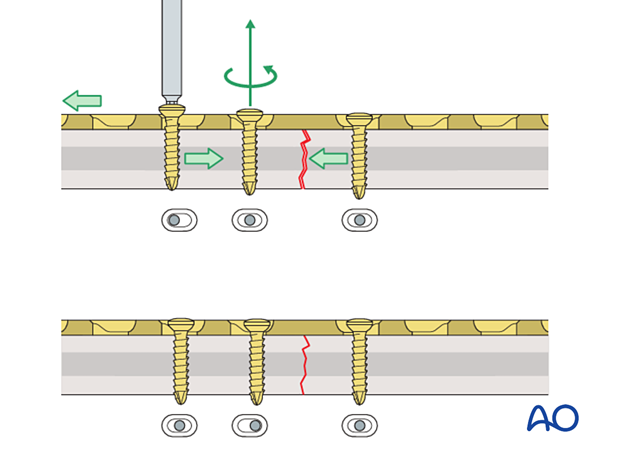
If a fracture gap remains after insertion of the two compression screws, a third screw can be inserted in compression mode. This can be located on either side of the fracture. Before this screw is tightened, the compression screw already placed in the same fragment needs to be loosened. Once the third screw is fully tightened, the loosened screw is re-tightened. Additional screws are then inserted in neutral mode.
Application of dynamic compression plate to transverse fractures.
Application (oblique fractures)
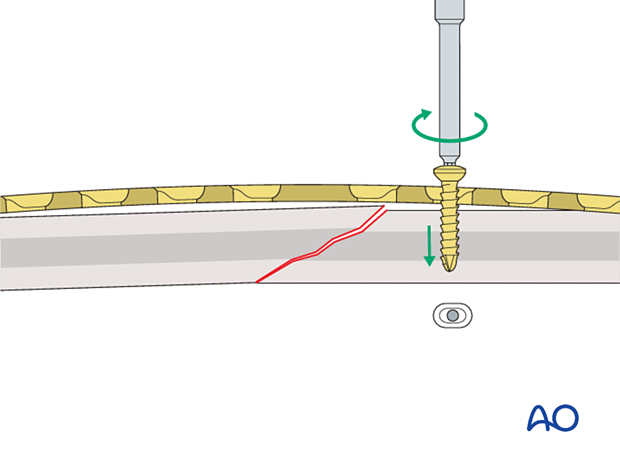
In oblique fractures, place the plate and fix it with one or more screws inserted in neutral mode to create an axilla with one of the bone fragments.
This 3D model shows screw insertion in neutral mode.
In oblique fractures, first the plate is placed and fixed with one or more screws inserted in neutral mode into the first fragment.
Application of dynamic compression plate to oblique fractures.
Insert a screw into the second fragment in compression mode. This drives the second fragment into the axilla and compresses the fracture.
This 3D model shows screw insertion in compression mode.
When inserting a screw in compression mode into the second (mobile) fragment, the fragment is driven into the angle formed by the fracture plane of the fixed (static) fragment and the undersurface of the plate (this is known as the axilla, highlighted in green) and the fracture is compressed.
If the plate is applied to an oblique fracture without creating an axilla, the fracture may displace as it is compressed.
If the fracture pattern and location do not allow an axilla to be created when applying the plate, it may be better to apply a lag screw and a neutralization plate.
If the plate is applied to an oblique fracture without creating an axilla then, when a screw is applied in compression mode, the fracture may displace. The apex of the mobile fragment is not “captured” by an axilla.
For the axilla concept to be applied:
- the plate must be orientated so that the direction of applied (compressive) force is co-aligned with the neutral axis of the bone
- the plane of the fracture must be close to perpendicular to the applied force
- the plate should be placed over the apex of the mobile fracture fragment
If the fracture pattern and location do not allow an axilla to be created when applying the plate, it may be better to apply a lag screw and a neutralization plate.
A lag screw can, in some cases, be inserted through the plate to provide additional compression.
These 3D models show a lag screw with a neutralization plate rotated 90° and aligned with it.
A neutralization plate can reduce the stresses on the lag screw. However, the positioning of the plate has only a minor influence on the screw, as demonstrated by the models.
Here compressive stress is shown in red and tensile stress is shown in blue.
Articulated tension device
For axial compression over a distance greater than 2 mm, the use of an articulated tension device is recommended.
This device may also be used to create distraction.
Reduce the fracture approximately, and securely attach the plate to one fragment.
Anchor the articulated tension device to the bone with a screw inserted through the articulated footplate and insert the hook on the device into the hole at the end of the plate.
As the tensioning screw is tightened, the two limbs of the device are pulled together, and compression is achieved at the fracture site.
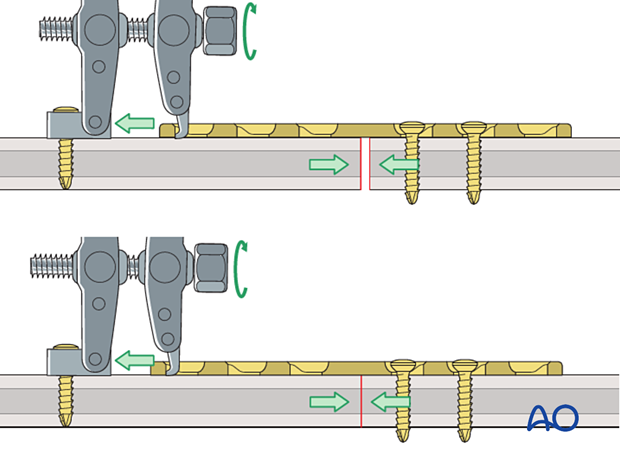
To distract the fracture, the hook of the device is placed against the plate end, and the tensioning screw on the device is turned anti-clockwise.
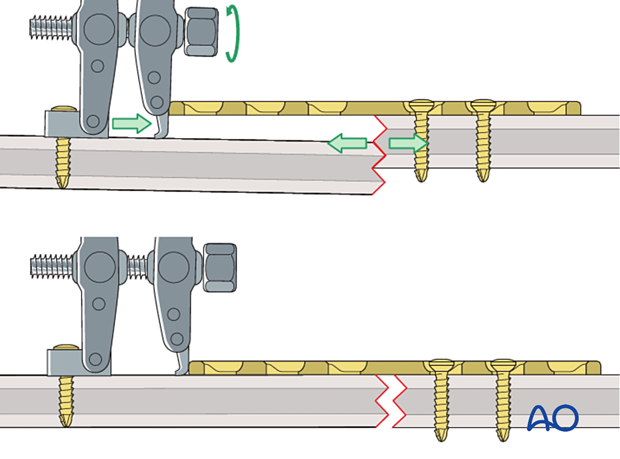
In oblique fractures, the plate should be applied to create an axilla following the principle described above for dynamic compression plates.
Screws are inserted into the second segment in neutral mode and the device is removed.
4. Bridge plates
Function
Bridge plating techniques are used for multifragmentary long bone fractures where intramedullary nailing or conventional plate fixation is not suitable.
The plate produces relative interfragmental stability by providing fixation of the two main fragments achieving correct length, and transverse and rotational alignment. The fracture site is left undisturbed, and fracture healing by callus formation is promoted.
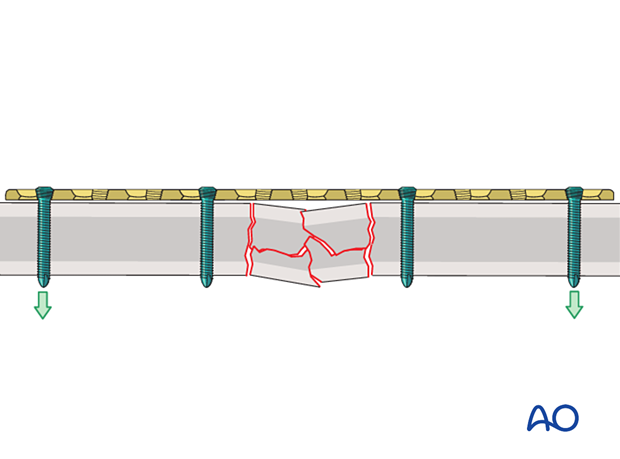
This 3D model shows a locked internal fixator.
The applied external force is transduced from one bone segment to the other via the plate and screw construct (primarily the inner screws). The plate has the function of a locked internal fixator, splinting the fracture. If the fracture gap closes (shown in the bottom panel), load sharing occurs and the force transmission is distributed between implant construct and the bone itself.
Compressive stress is shown in red and tensile stress is shown in blue.
Conventional vs locking head screws
Either conventional or locking head screws may be used.
These 3D models show the insertion of a locking head screw (top panel) and a conventional screw in neutral mode (bottom panel).
The conventional screw is inserted in neutral mode and pulls the plate against the bone. Locking head screws engage in the plate using the threads and therefore the plate is not pressed against the bone.
These 3D models show the difference between inserting locking head screws (top panel) and inserting conventional screws eccentrically (bottom panel).
The eccentric insertion of the conventional screw creates relative movement between the bone and the plate in addition to pressing the plate against the bone.
Locking head screws have the following advantages when compared to conventional screws:
- They provide more stability in osteoporotic bone by reducing the risk of screw pullout and over-tightening of the screws
- Well reduced fractures stay reduced
- Unicortical screws may be used
- The plate does not need to be perfectly contoured to the bone
- As the plate is not pressed against the bone, periosteal perfusion is not compromised
These 3D models allow bending of locking head screws and conventional screws to be simulated.
The fixed angle locking construct (bottom panel) provides considerable stability and there is bending of both the screw and the plate. In contrast, the conventional screw (top panel) can freely rotate in its plate hole without causing deformation.
High stress is shown in red and low stress is shown in green.
Extent of surgical approach
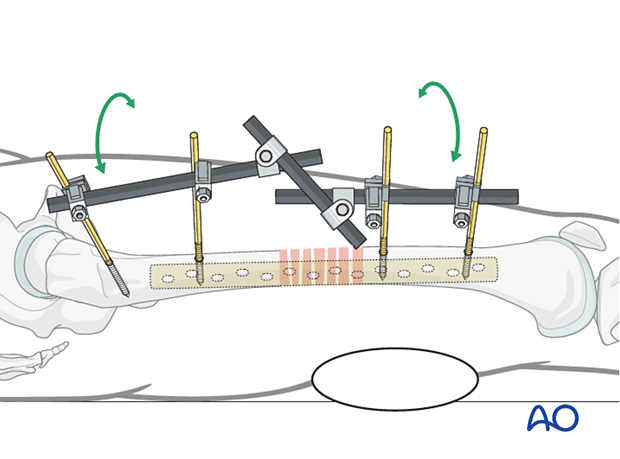
To disturb the fracture site as little as possible, bridge plates are often inserted through a minimally invasive approach.
Screws are either inserted through a limited approach, only exposing the plate sufficiently for screw insertion, or through small stab incisions.
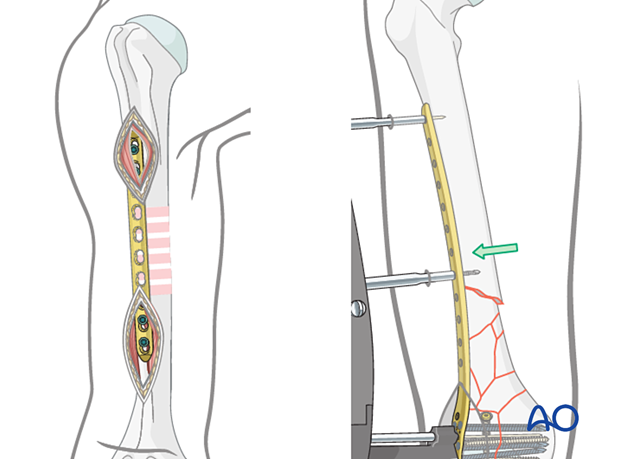
The least surgical disturbance to the fracture site occurs when a minimally invasive percutaneous technique is used for plate insertion.
Reduction
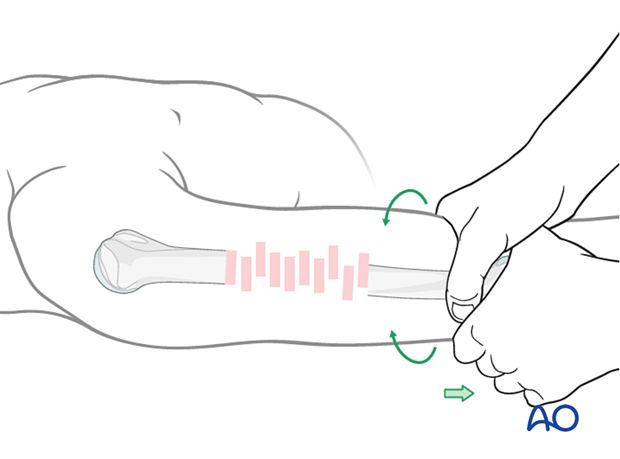
Reduce and secure the main proximal and distal fragments in correct length, alignment, and rotation.
This is typically achieved using indirect reduction tools and techniques such as:
- Temporary external fixation
- Reduction devices, eg, pointed forceps
- Traction
Indirect reduction allows manipulation of the main fragments into the correct position without opening the fracture site, thus minimizing further damage to the blood supply.
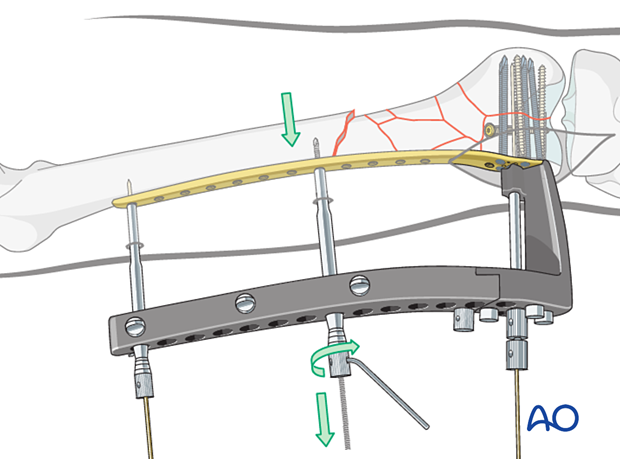
Especially with multifragmentary fractures, the use of an external fixator, or distractor, can provide alignment and temporary stability for bridge plating without disturbing the soft tissues at the fracture zone.
Pins should be located carefully in order to avoid interference with the later plating procedure.
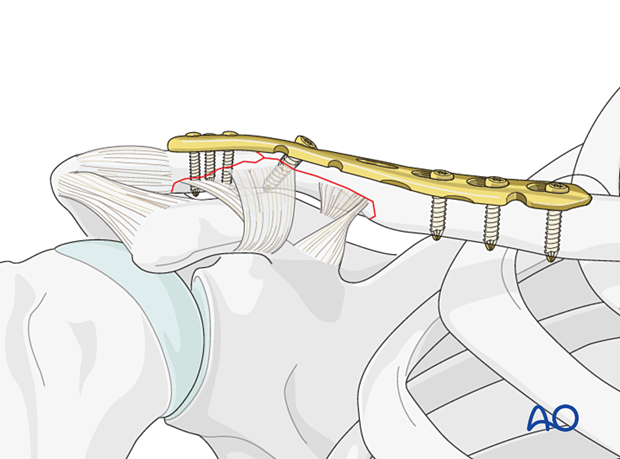
5. Buttress (antiglide) plates
Function
Buttress plates are used in managing partial articular fractures. They are used to supplement lag screw fixation of metaphyseal shear or split fractures in the metaphyseal regions. Lag screws may be inserted either through or outside the buttress plate.
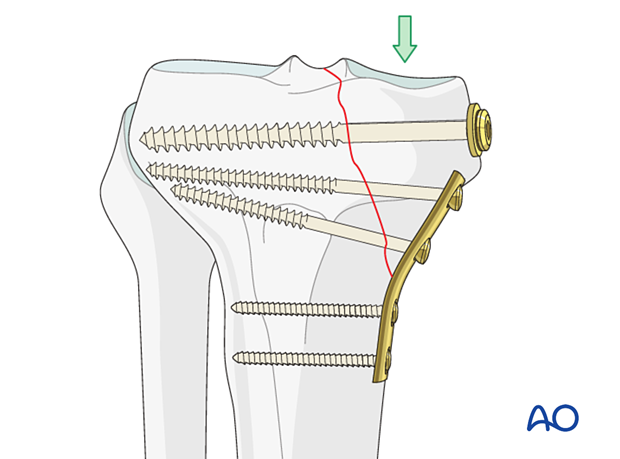
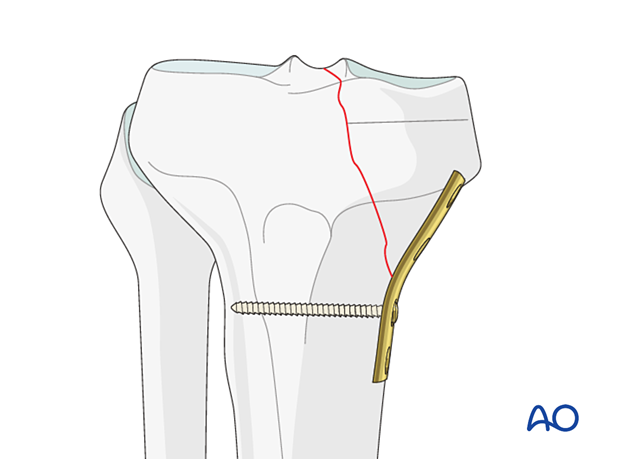
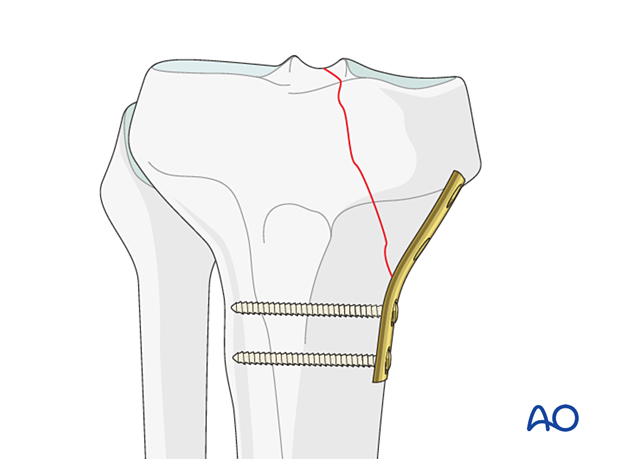
Application
After reducing the fracture with reduction forceps, contour the plate with a slight pre-bend so that it overlies the apex of the fracture and captures a sufficient amount of the proximal and distal fracture fragments.
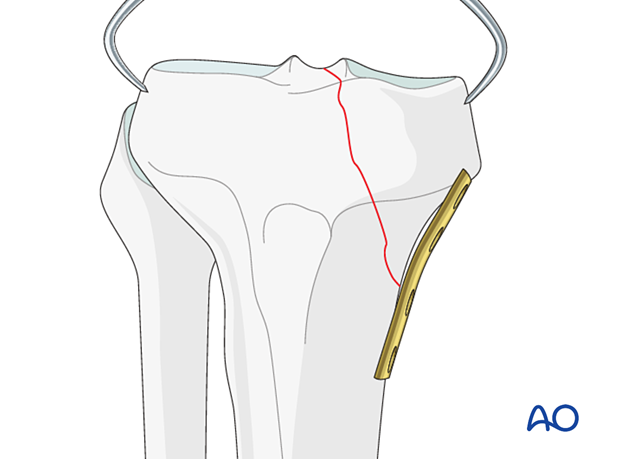
Apply the plate and press it firmly against the bone by inserting a standard bicortical screw in the hole closest to the fracture in buttress mode.
This 3D model shows the effect of improper plate contouring.
If a plate is improperly contoured (as shown in the panel on the right) then contact between the plate and bone at the apex of the fracture is not achieved, leading to an inadequate buttressing or antiglide effect. The plate should form an “axilla” (see the 3D models of the axilla concept given above in the “Application (oblique fractures)” section for further information) with the intact cortex to prevent axial displacement of the mobile fragment (as shown in the panel on the left). The plate should be only slightly undercontoured and should have good bony contact at the apex of the fracture at the axilla to optimize the antiglide effect. If the plate is undercontoured too much, then displacement of the fracture may occur when the plate is fixed in position (as shown in the panel on the right): the plate induces undesirable displacement of the mobile fragment. Also, notice that in this case there is no bony contact with the plate at the axilla so that there is almost no antiglide effect, leading to a further biomechanical disadvantage.
This 3D model shows the effect of improper screw/plate positioning.
If the plate is improperly positioned and the screw is improperly placed (as shown in the right panel), insufficient compression of the fracture fragments is achieved and the plate does not form an axilla with the intact cortex.
Secure the buttress plate with additional bicortical screws inserted in neutral mode.
Reduce and fix the fracture with one or more lag screws following standard technique either through or outside the buttress plate.
A washer may be used in osteoporotic bone if a lag screw is placed outside the plate.
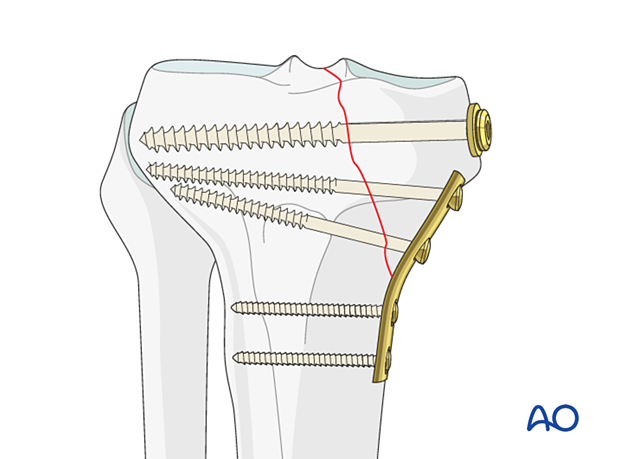
These 3D models show the effect of lag screw position.
Additional lag screws can be placed either independently of the plate (middle panel) or through the plate (right panel). This further increases the fixation stiffness and strength especially under load which is not purely in an axial direction.













