Deltopectoral approach
1. Introduction
The deltopectoral approach and its extensions can be used to access almost any humeral periprosthetic shaft fracture.
This approach is also highly recommended for revision surgery.

2. Anatomy of the upper arm
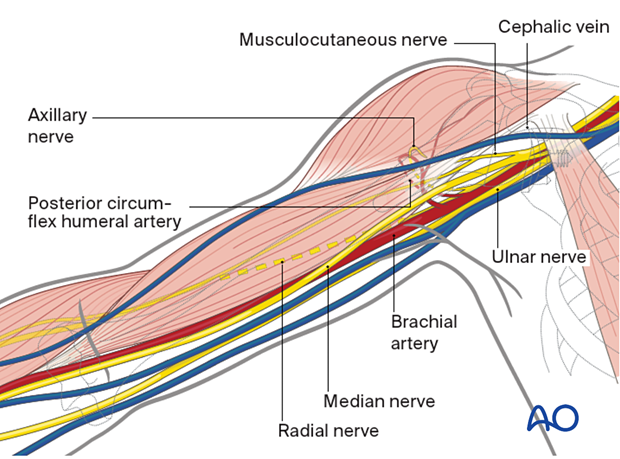
Surgical exposure of a periprosthetic fracture is made more complicated and carries greater risk to neurovascular structures due to scarring, adhesions, and contractures, particularly around the brachial plexus and its branches.
The course of the following neurovascular structures should be kept in mind:
- Cephalic vein
- Anterior circumflex humeral artery
- Axillary nerve
- Posterior circumflex humeral artery and vein
- Musculocutaneous nerve
- Radial nerve
Neurovascular structures, eg, the brachial plexus, are at risk if retraction is too forceful.
3. Skin incision
If the previous deltopectoral approach fits well with the planned revision surgery, it can be used and extended distally. However, do not hesitate to make a new incision that facilitates the identification of a necessary landmark.
Palpable anatomical landmarks for the deltopectoral approach are:
- Coracoid process
- Proximal humeral shaft (at the level of the axilla)
- Lateral epicondyle of the distal humerus
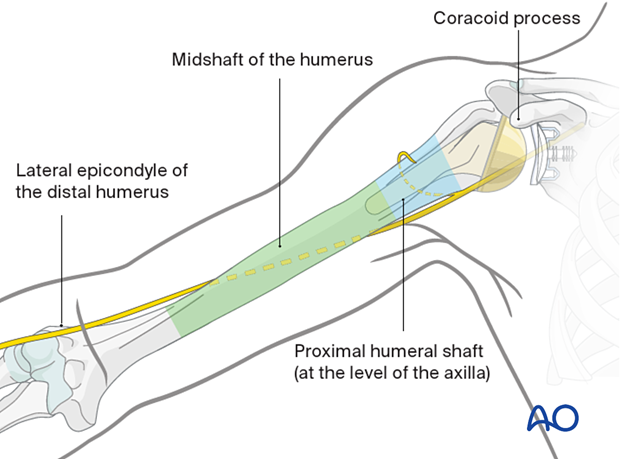
The skin incision starts at the coracoid process and follows the humeral shaft distally towards the lateral epicondyle. The length of the skin incision depends on the planned plate length.
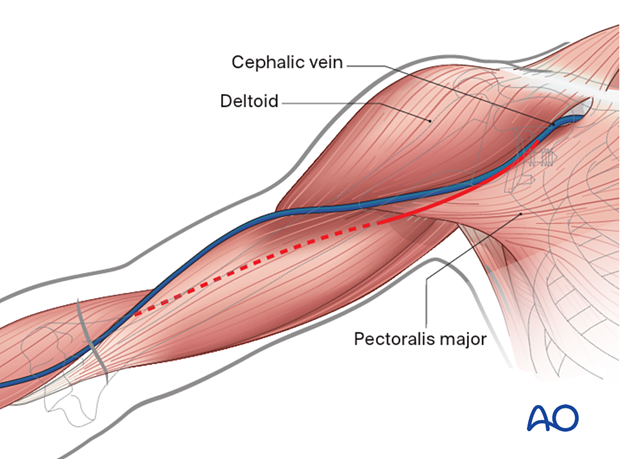
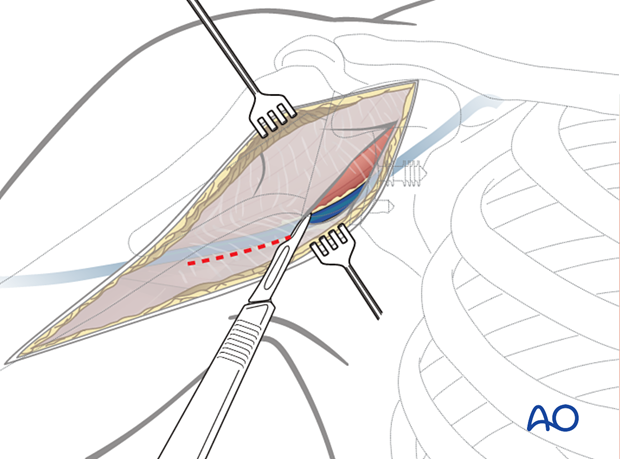
4. Exposure of the superficial fascia
Expose the deltopectoral groove with the cephalic vein (if still present). These structures can be identified by:
- The course of the muscle fibers
- The cephalic vein itself
- Fat tissue surrounding the vein (In revision cases, the fat tissue is often replaced by scar tissue that can be used for guidance)
For better exposure, it is recommended to dissect at the lateral border of the pectoralis major.
If in doubt, extend exposure proximally and distally to undisturbed tissue to identify the groove.
5. Exposure of the deep layers
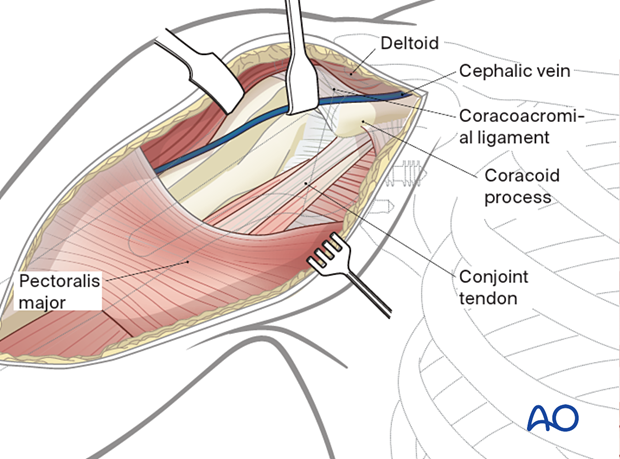
Identify the coracoid process and the conjoint tendon.
Incise the clavipectoral fascia lateral to the conjoint tendon and inferior to the coracoacromial ligament.
The conjoint tendon is often scarred to the surface of the subscapularis muscle, leading to difficulty in identifying the axillary nerve.
The subdeltoid space is usually adherent with scar tissue and careful dissection within the bursa space is required to protect the nerve.
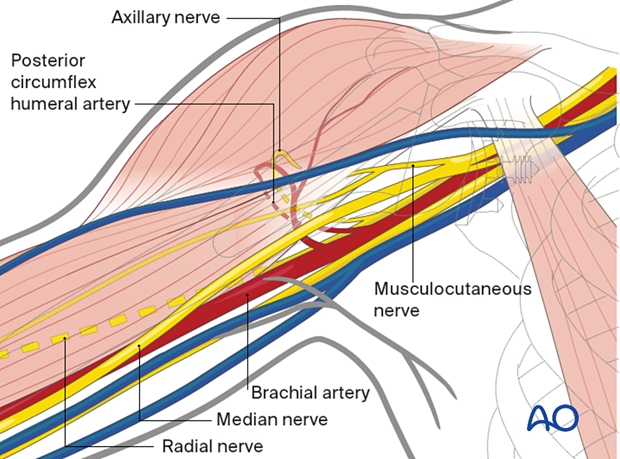
6. Exposure of the brachial plexus
It is frequently necessary to identify the axillary nerve medial to a prosthesis during revision surgery.
If the axillary nerve cannot be readily identified because of scar tissue, a safe surgical tactic to expose the nerve includes:
- The use of a peripheral nerve stimulator to identify nerve trunks
- Identification of the lateral cord and musculocutaneous nerve (which enters the coracobrachialis at a variable distance from the coracoid process)
- Identification and protection of the axillary artery and vein behind the lateral cord
- Identification of the posterior cord behind the axillary artery
- The first lateral branch of the posterior cord is the axillary nerve
- This accompanies the posterior circumflex artery through the axilla
- Bleeding from the posterior circumflex vein can be profuse. It is advisable to control this by ligating the vein, if necessary before identifying the axillary nerve.
- If the quadrilateral space is obscured by a scar, safe exposure of the axillary nerve can be facilitated by detachment and gentle retraction of the conjoint tendon.
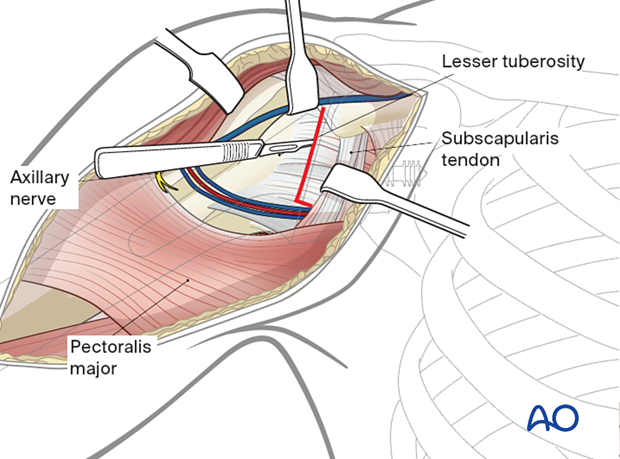
The deltoid muscle is retracted laterally and the conjoint tendon is retracted medially.
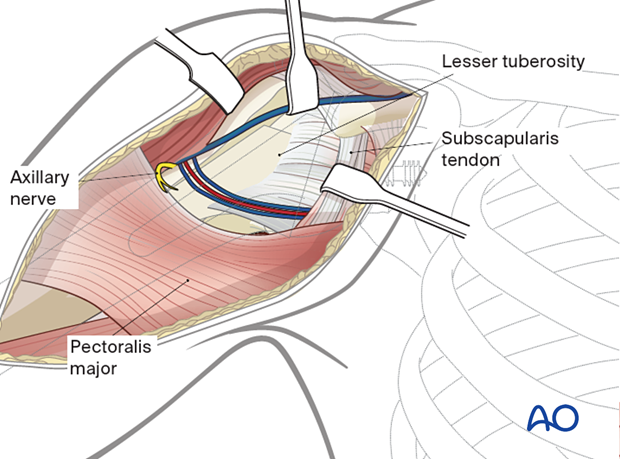
Depending on arthroplasty configuration and the expected revision tactics the subscapularis tendon is mobilized and reflected by:
- Lateral peel
- Tenotomy
- Lesser tuberosity osteotomy
The tendon is often absent when a previous reverse shoulder replacement has been performed: the usual landmarks for identification of the axillary nerve are absent.
7. Distal extension of the deltopectoral approach
The extended incision is directed towards the lateral epicondyle of the humerus to the appropriate length for planned fixation.
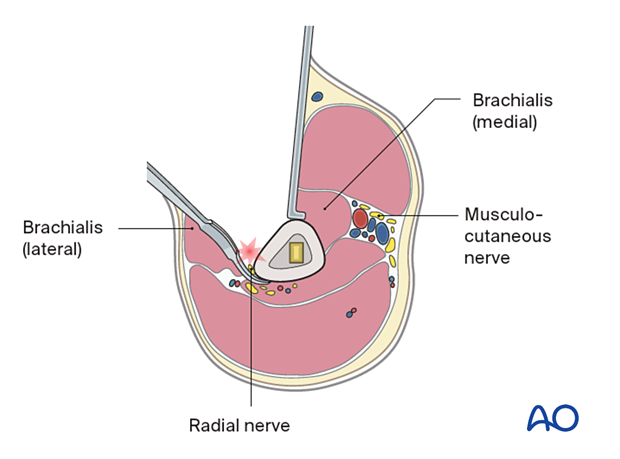
Extend the incision of the deep fascia of the upper arm carefully between the biceps and the brachialis. Further distal extension between the brachialis and the brachioradialis allows exposure of the distal humerus.
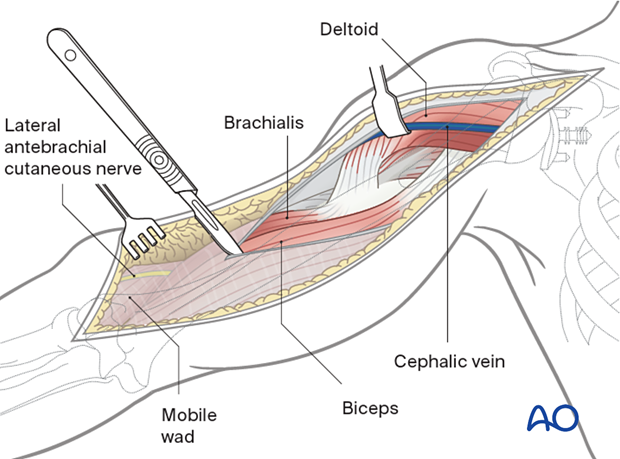
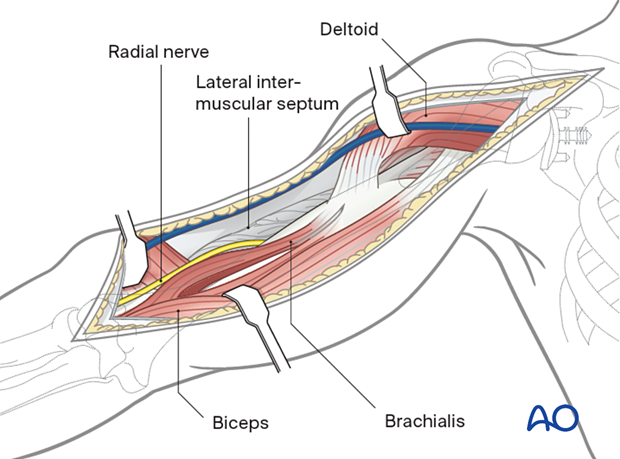
Retract the biceps medially and the brachioradialis laterally to identify the radial nerve lying between the brachioradialis and the brachialis.
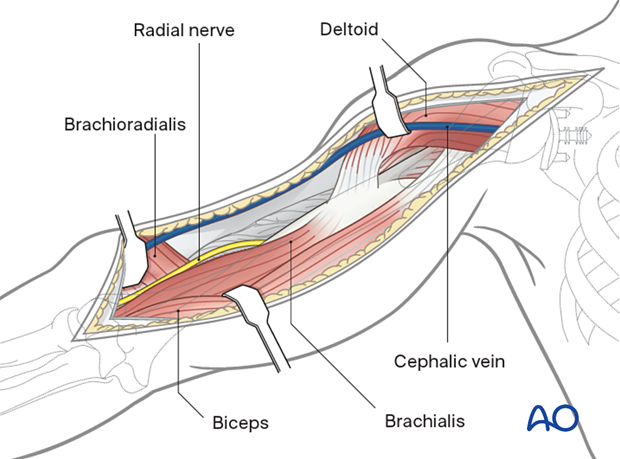
Split the brachialis between the radial third and the medial two thirds of the muscle: this preserves its innervation from the radial nerve and musculocutaneous nerve as far as possible.
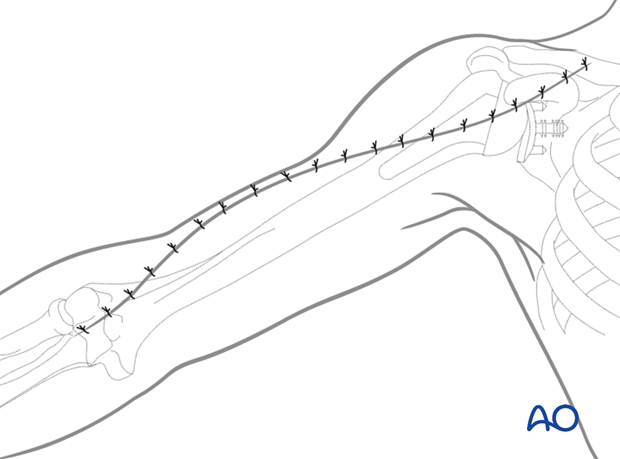
8. Wound closure
The wound should be irrigated. Placement of a drain underneath the deltoid muscle might be considered.
The subcutaneous fascia and the skin are closed in layers.