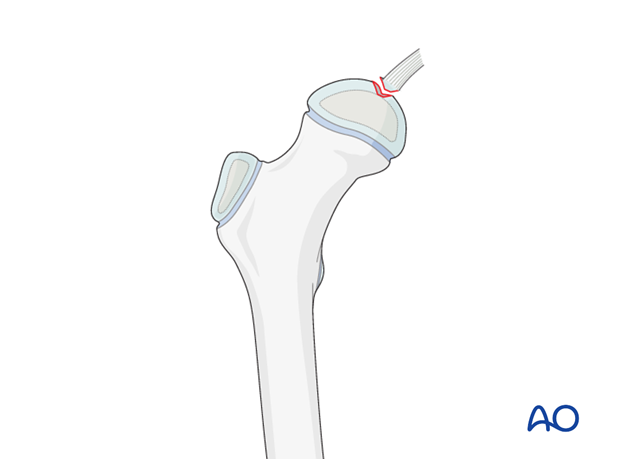
Removal of osteochondral fragment
1. Introduction
Open capsulotomy vs arthroscopy
Small osteochondral fragments, as determined by MRI, can be removed either through a capsulotomy, or arthroscopically.
The indication for arthroscopic removal depends on the surgeon's skill with hip arthroscopy.
The advantages of hip arthroscopy are:
- Minimally invasive capsulotomy
- Enhanced visualization of the joint
- Visualization of the osteochondral defect in the head
The limitation of an arthroscopic approach is the size of the fragment. Larger fragments will require conversion to an open approach.
Note: Flake fractures are mostly the result of traumatic hip dislocation.
Incongruency after dislocation is very often overlooked on conventional x-rays.
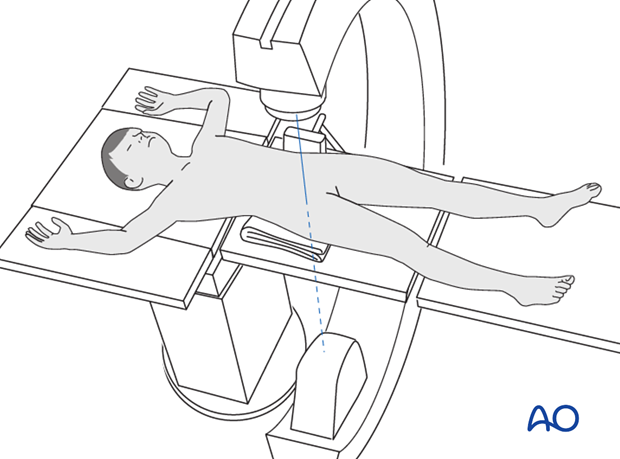
Joint distraction
Gentle distraction of the joint may facilitate irrigation and visualization.
For arthroscopic removal, a fracture table is always used.
Note: For a detailed description, the reader is referred to the corresponding textbooks, or literature.
In an open procedure, "free-hand" distraction, or distraction using the fracture traction table is at the discretion of the surgeon.
The advantage of free-hand distraction is the ability to rotate the femoral head. However, the amount of distraction possible is less than when using a traction table.
2. Patient preparation and approaches
Approaches
For this procedure the following approaches may be used:
In some specific cases (eg, large fragments, or a bigger defect on the femoral head), surgical hip dislocation can become necessary for removal of the fragment. Surgical hip dislocation also facilitates reattachment of the fragment, or corrective osteotomy to reorientate the intact part of the femoral head into a good loading position.
3. Open capsulotomy
Removal of fragments
After the capsulotomy, the joint is irrigated and large fragments are picked out using forceps, pituitary rongeurs etc.
All fragments identified on the preoperative MRI should be accounted for.
Subluxation by traction, with internal and external rotation, is useful for visualization of the joint and to free trapped fragments.
Irrigation of the subluxed joint will often flush out hidden fragments.
For larger fragments, complete hip dislocation may be necessary.
Image intensification should be used to confirm concentric reduction.
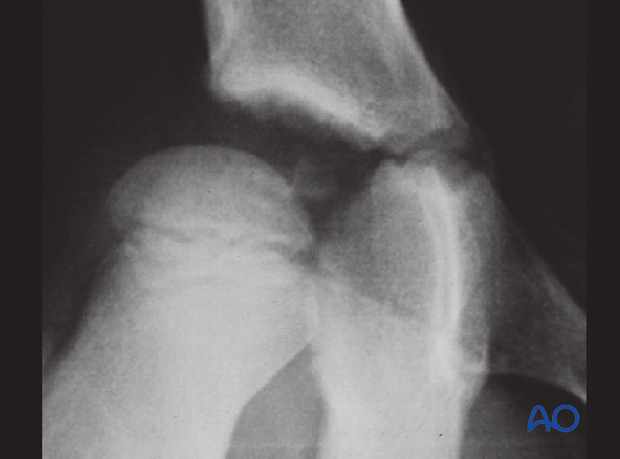
Case example
History: A 7-year-old boy sustained a ski injury while jumping over a bump and landing directly on the hip.
The right hip was dislocated.

After reduction, the joint space was asymmetric and a fragment was seen in the joint space.
This is an absolute indication for removal of the fragment.
4. Aftercare
Introduction
After surgical stabilization, the construct should be sufficiently robust to allow protected weight bearing. Smaller children may not be able to comply with this and may need immobilization.

Infection
See the additional material on postoperative infection.
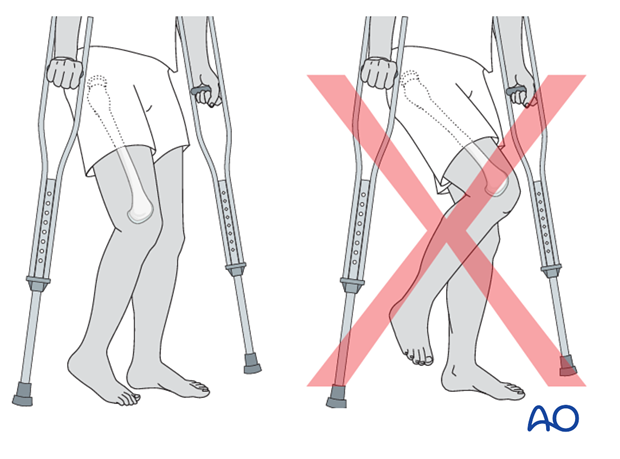
Mechanics
Forces through the hip are less with toe-touch weight bearing than with non-weight bearing. Therefore, toe-touch is normally recommended for initial mobilization. This needs to be taught to children by a physiotherapist.
Range of movement
Range-of-movement exercises should start in the immediate postoperative period to prevent stiffness. Surgeons should indicate if any extremes of movement are forbidden.
Weight bearing
Having started with toe-touch weight bearing, children progress to partial weight bearing and then to full weight bearing according to their age and the predicted rate of healing of their fracture.
Even older adolescents should be fully weight bearing without aids at three months.
Sports
Swimming can be allowed as soon as partial weight bearing is permitted.
Contact sports should be avoided for at least six months.
Follow-up x-rays
X-rays are generally taken immediately after the surgery and at 6 and 12 weeks.
Implant removal
Implants that cross the physis should be removed if there is significant growth remaining. The fracture should be healed and consolidated prior to removal (see Healing times).
Implants in young children should always be removed to prevent them from being covered by bony overgrowth.
Implant removal is not compulsory in adolescents.













