Postoperative infection in children
1. Infection after osteosynthesis in children
This section does not address hematogenous osteomyelitis in children, which is a separate pediatric orthopedic pathological consideration.
The management of infection after osteosynthesis in children follows the same basic principles as those in adults with similar complications.
2. Diagnosis
This is a dynamic process, and incremental observations are necessary to make a confident diagnosis of wound infection.
The characteristics are:
- Increasing wound pain
- Increasing swelling, redness, local temperature
- Increasing systemic temperature
- Wound discharge
- Rising hematological markers for infection, ESR, WBC, CRP, etc
This clinical picture shows an example of a ten-day surgical wound with abscess beneath.

Once the diagnosis is strongly suspected, the treatment is essentially surgical, with adjuvant pharmacological support, guided by microbiological studies of tissue samples taken from the wound.
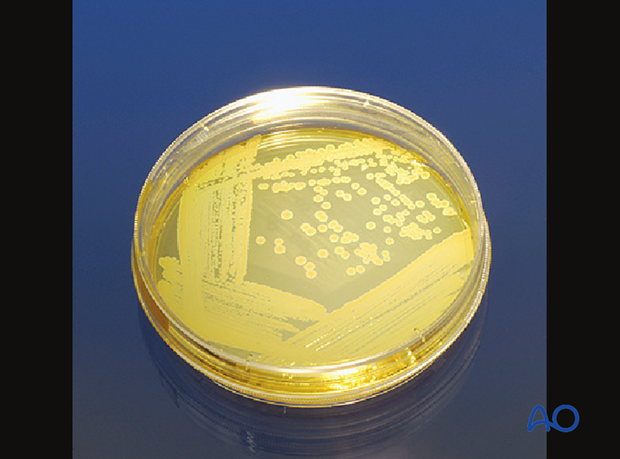
Surgery comprises opening the surgical field, taking tissue samples for microbiological study, excision of all non-viable and overtly infected tissue, thorough drainage and lavage with Ringer lactate solution (not under high pressure), and assessment of the fixation.
This clinical picture shows the above wound opened with pus coming out.

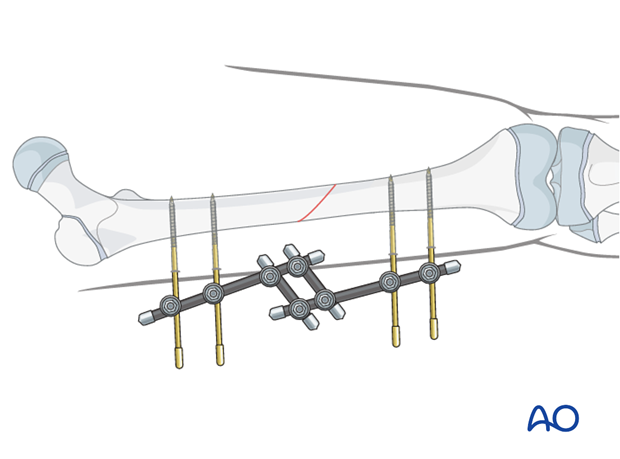
Should the fixation have failed and become unstable, then it should be removed and the fracture restabilized, usually by external fixation.
The operative wound is left open to drain freely, either with loose packing, using antiseptic-impregnated gauze, or a vacuum-assisted closure device (as illustrated).
High-dose systemic antibiotic therapy is started once microbiological results are to hand.
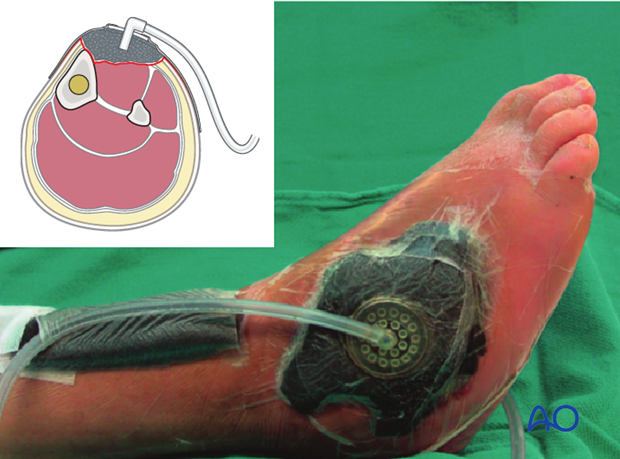
The wound is regularly cleansed and, only when the infection is well under control, should soft-tissue cover be considered.
The detailed principles are addressed in the adult AO Surgery Reference.













