Open reduction, screw fixation
1. Preliminary remarks
Avascular necrosis
These fractures involve acute failure of the physis, which is usually the result of high energy trauma. Accordingly, the risk of avascular necrosis is high and a gentle anatomical reduction with stable internal fixation is required to provide the best prognosis.

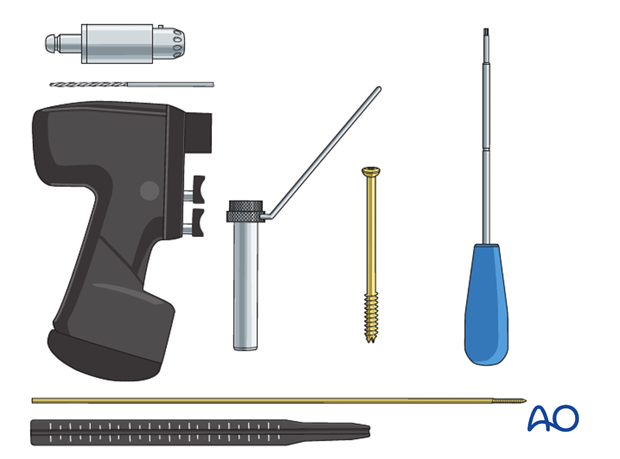
Hardware selection
6.5, 7.0, or 7.3 mm cannulated screws are used for adolescents.
4.0, or 4.5 mm cannulated screws may be selected for younger children. Be aware that these screws are considerably weaker and prone to breakage if used in too heavy a child.
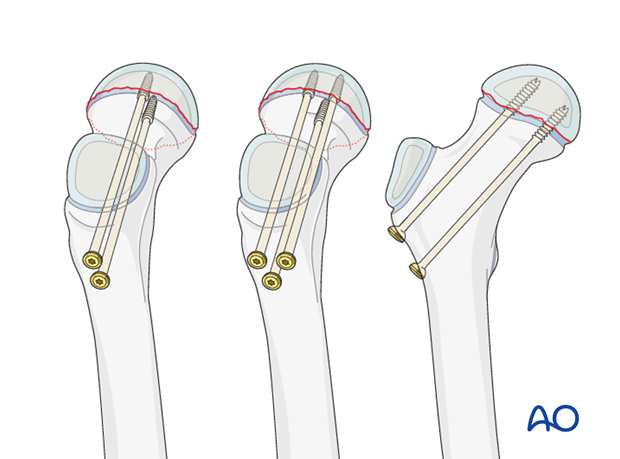
Implant insertion
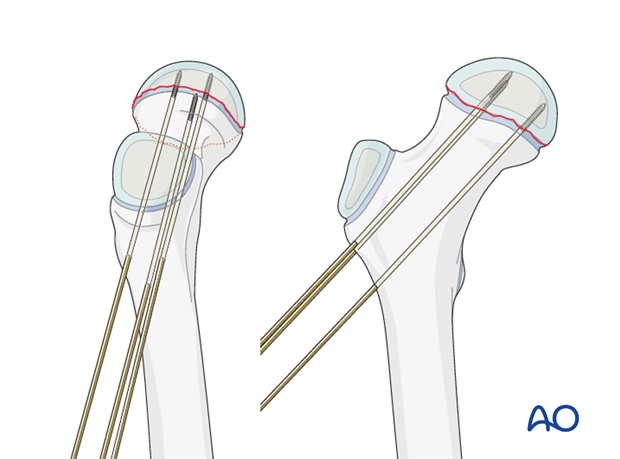
Typically, two screws separated vertically are inserted. This configuration may be more suitable in smaller bones.
An alternative is three screws used in an apex-distal, triangular configuration, with the lower central screw abutting the calcar.
Inserting a single central screw does not provide rotational stability and is, therefore, less applicable for fractures, even though it is a common choice for slipped capital femoral epiphysis (SCFE).
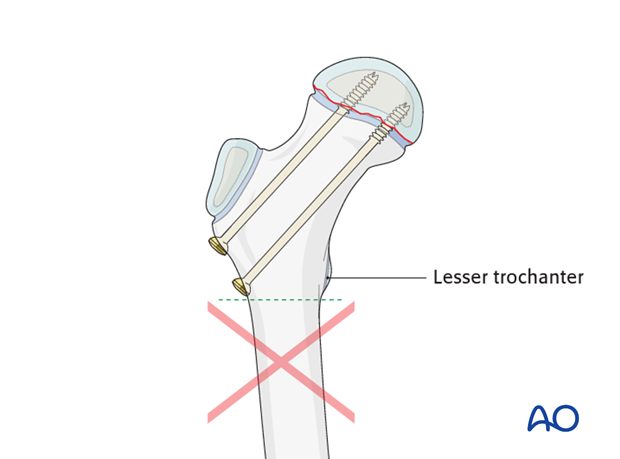
Pitfall: Secondary subtrochanteric fractures may occur if screws are inserted below the level of the lesser trochanter.
2. Patient preparation and approaches
Approaches
For this procedure the following approaches may be used:
3. Reduction
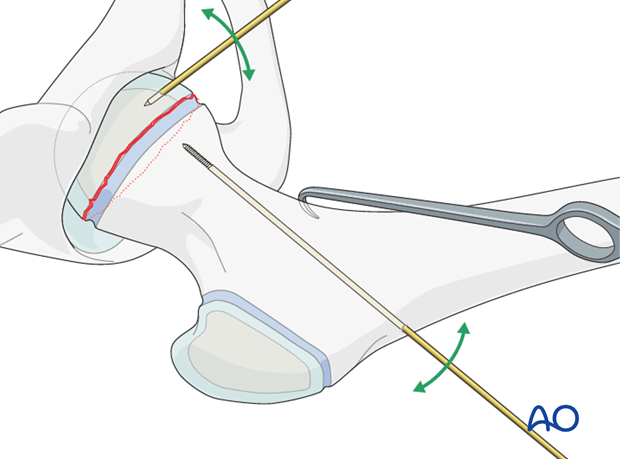
A K-wire is inserted through the lateral cortex of the femur just above the level of the lesser trochanter and advanced to the fracture line.
Pitfall: Secondary subtrochanteric fractures may occur if K-wires are inserted with an entry point distal to the level of the lesser trochanter.

The femoral neck is manipulated gently into position, usually by traction in the line of the femoral neck using a bone hook.
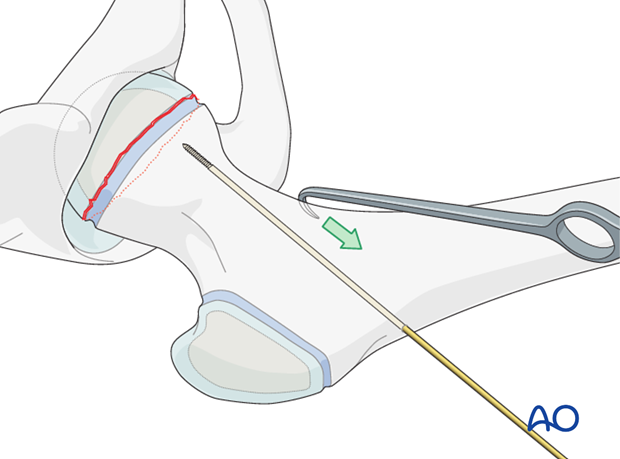
If necessary, manipulation of the femoral head is achieved using a small K-wire inserted into the epiphysis, as a joystick.
Gentle reduction maneuvers are emphasized in order to prevent secondary damage to the femoral head blood supply.
4. Fixation
Guide wire insertion
When anatomical reduction is obtained, the first wire is advanced across the fracture and into the femoral head. Penetration into the hip joint should be avoided.
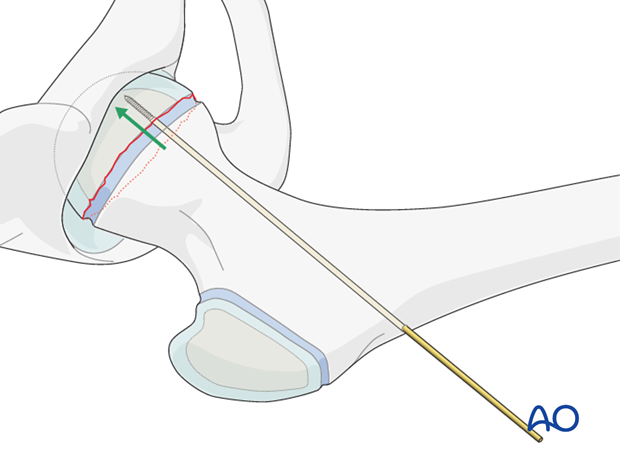
Additional wires are inserted under image intensifier control, according to the two- or three-screw configuration chosen.
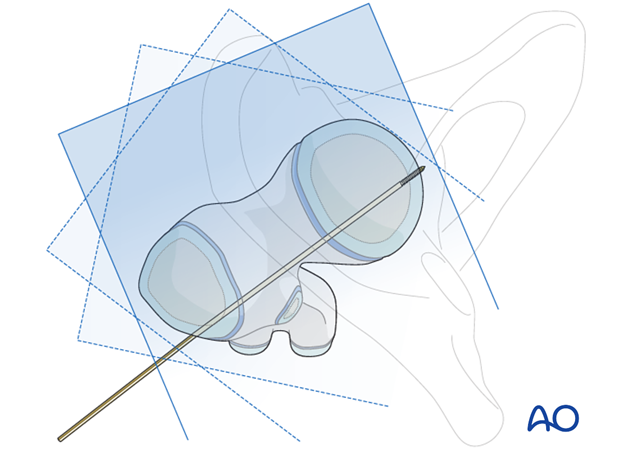
X-ray control
The guide wire positions are confirmed on AP and lateral x-rays.
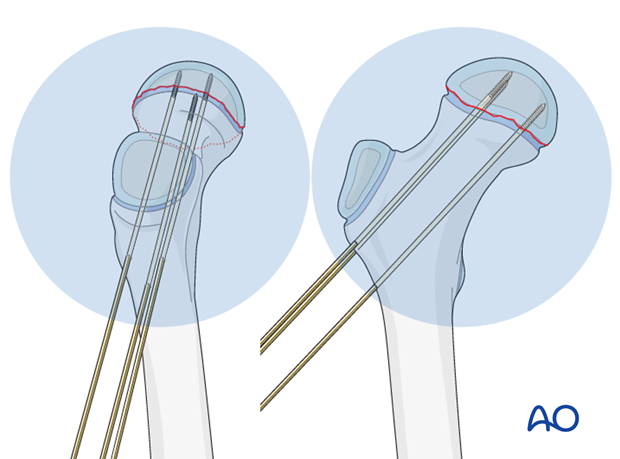
If using a standard radiolucent table, the K-wire fixation is generally stable enough to allow a “frog” lateral view.
The wires are repositioned if necessary.

Images at multiple angles are used to confirm that the guide wires do not penetrate into the hip joint.
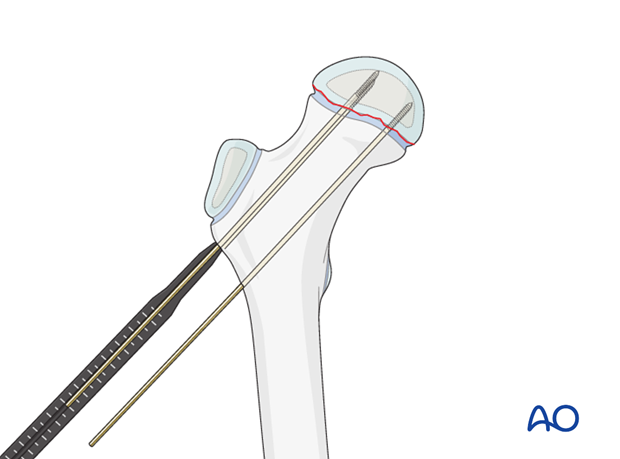
Measuring screw length
A depth gauge is used to measure screw length.
If a dedicated cannula/depth gauge set is not available, then a K-wire, of the same length as that inserted, is placed onto the lateral cortex adjacent to the inserted wire, and the difference measured to determine the screw length.
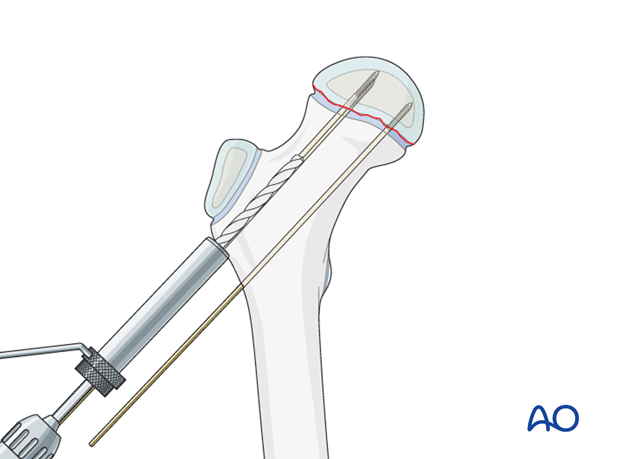
Drilling screw holes
The wires are overdrilled with the appropriately sized cannulated drill bit.
Adolescents in particular have very dense strong bone in the metaphysis near the growth plate and predrilling is recommended.
If cannulated screws are not available, then guide wires should be removed one at a time and an appropriate drill used.
Screw insertion
Two or three cannulated screws are then inserted over the guide wires.
Note: Fully-threaded cannulated screws are easier to remove later.
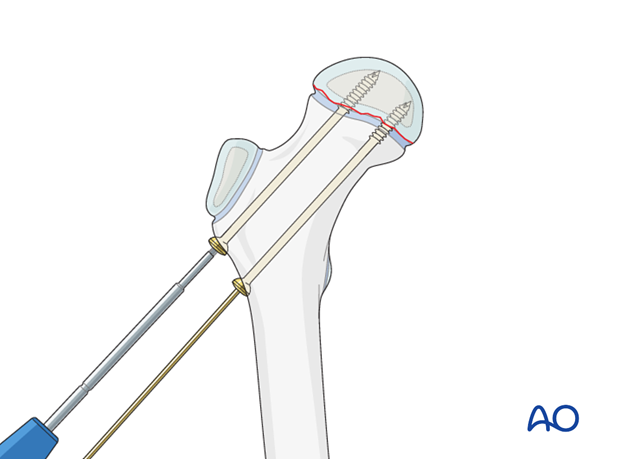
X-ray control
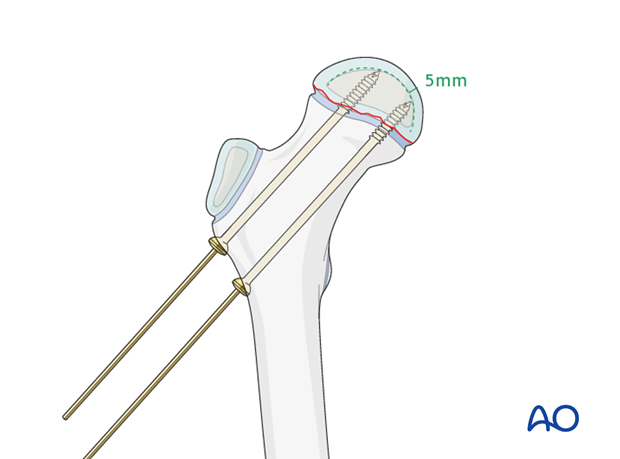
Image intensification is used to confirm that the screw tip does not penetrate into the cartilage or the joint.
Typically, 5 mm of epiphyseal bone/cartilage should remain between the screw tip and joint surface. Three or four threads crossing the physis provides adequate fixation.
Pitfall: Screw penetration can occur, especially with eccentrically placed screws, even if not apparent on standard AP or lateral x-rays.
Real-time, dynamic image intensification, through a full range of internal and external rotation, and at different degrees of flexion, is useful to confirm the distance between the screw tip and the joint space.
Observing an approach/withdrawal of the screw tip helps in judging its position. Some surgeons supplement this examination with 3-D image intensification for confirmation.
Arthrography is useful to confirm correct wire and screw placement in the younger patient.
Guide wire removal
Guide wires are removed.

5. Hip spica
If solid fixation has been obtained with screws, and the patient/family can reliably comply with toe-touch weigh bearing, then a cast is not necessary.
For patients below 5 years of age, a hip spica cast can be used if desired.
Click here for details of hip spica application.
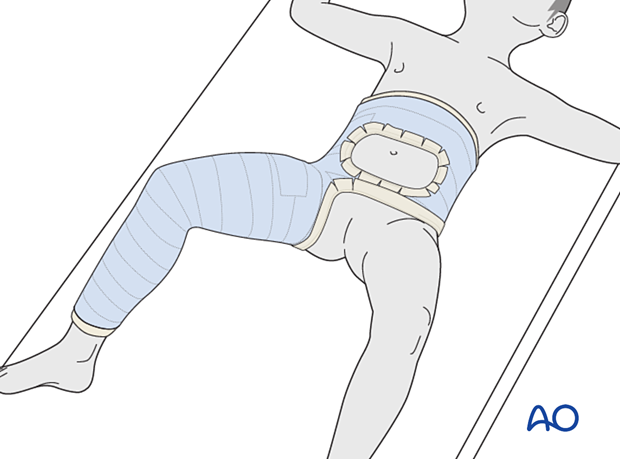
Aftercare following hip spica application
After application, the spica should be trimmed to allow adequate space for bodily functions. The edges of the spica should be padded and waterproofed.
Generally, a hip spica should allow space for a small diaper inside the plaster and a large one outside the plaster. The diapers should be positioned to prevent soiling of the spica.
The spica is not waterproof. Bathing and showering should not be attempted. Hair washing should be done very carefully.
No skin products should be put inside the spica. Only skin that can be seen should be moisturized.
6. Aftercare
Introduction
After surgical stabilization, the construct should be sufficiently robust to allow protected weight bearing. Smaller children may not be able to comply with this and may need immobilization.

Infection
See the additional material on postoperative infection.
Mechanics
Forces through the hip are less with toe-touch weight bearing than with non-weight bearing. Therefore, toe-touch is normally recommended for initial mobilization. This needs to be taught to children by a physiotherapist.
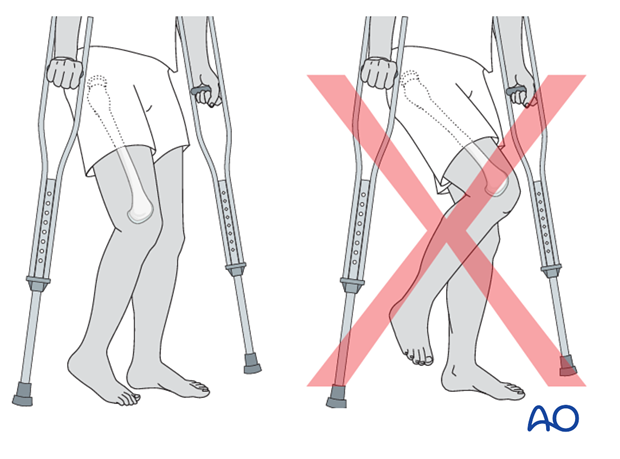
Range of movement
Range-of-movement exercises should start in the immediate postoperative period to prevent stiffness. Surgeons should indicate if any extremes of movement are forbidden.
Weight bearing
Having started with toe-touch weight bearing, children progress to partial weight bearing and then to full weight bearing according to their age and the predicted rate of healing of their fracture.
Even older adolescents should be fully weight bearing without aids at three months.
Sports
Swimming can be allowed as soon as partial weight bearing is permitted.
Contact sports should be avoided for at least six months.
Follow-up x-rays
X-rays are generally taken immediately after the surgery and at 6 and 12 weeks.
Implant removal
Implants that cross the physis should be removed if there is significant growth remaining. The fracture should be healed and consolidated prior to removal (see Healing times).
Implants in young children should always be removed to prevent them from being covered by bony overgrowth.
Implant removal is not compulsory in adolescents.













