Open reduction - Compression plating
1. General considerations
Introduction
Humeral shaft fractures may be treated with compression plating under the following conditions:
- Reduction and stability not achieved with other techniques, particularly in older children
- Open fractures
- Neurovascular injuries
- Polytrauma
The principles of fixation are identical to adult fracture management.
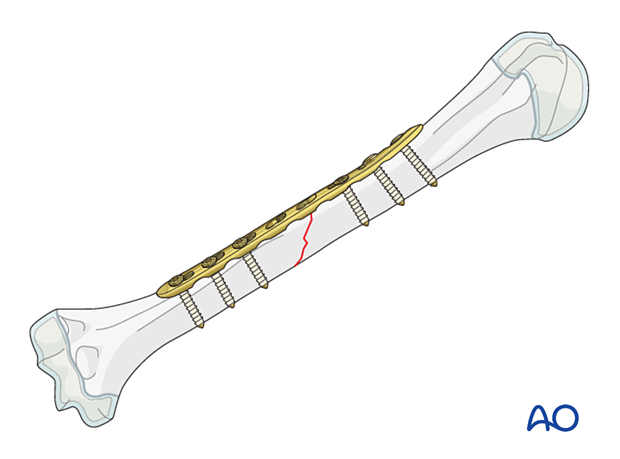
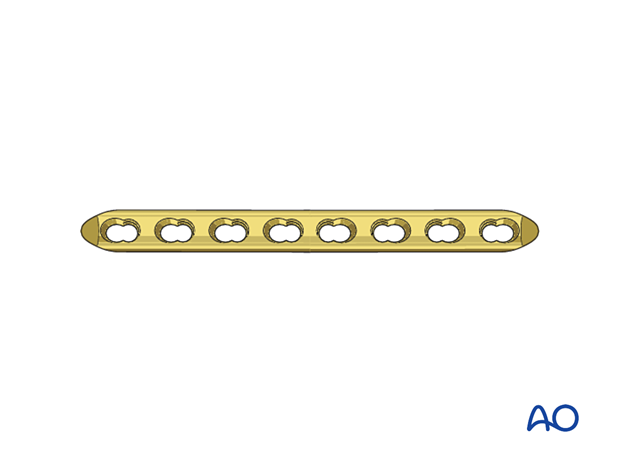
Plate selection
The plate should allow for insertion of a sufficient number of screws on either side of the fracture.
Plates that accommodate the smaller pediatric humerus are available. A 3.5 or 4.5 mm LCP or DCP is recommended depending on the bone size.
An additional lag screw through the plate perpendicular to the fracture plane may be planned.
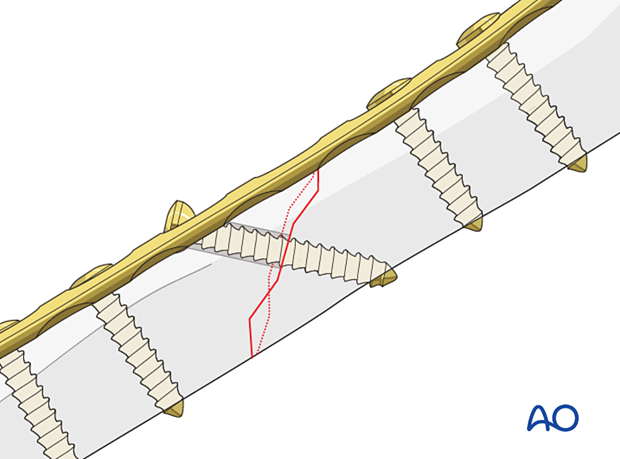
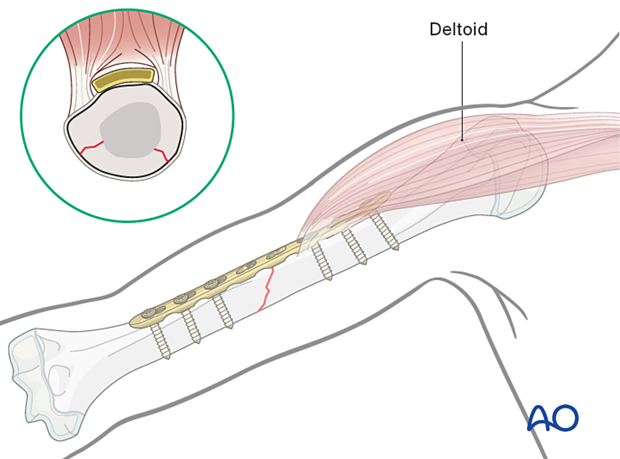
Plate position
Open fractures may dictate the surgical approach and the plate position.
The position and contouring of the plate are dictated by the location of the fracture in relation to the soft-tissue attachment and its proximity to the axillary and radial nerves.
The course of the radial nerve in relation to the plate holes should be documented to reduce the risk of nerve injury associated with plate removal.
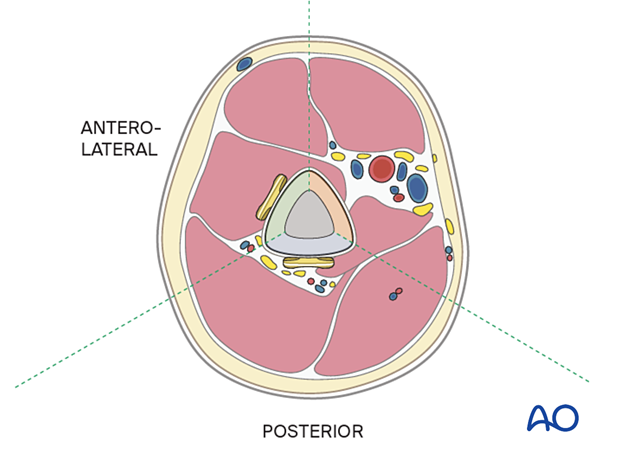
A posterior plate is preferred for middle and distal third fractures.
An anterolateral plate may be selected for proximal and middle third fractures.
2. Patient preparation
Place the patient in a supine position or, alternatively, a beach chair position for an anterolateral plate.
Place the patient prone or in a lateral decubitus position for a posterior plate.
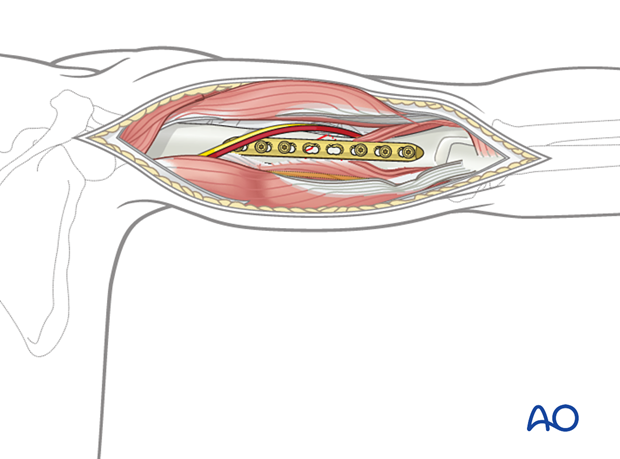
3. Approaches
The approach depends on the plate position.
For an anterolateral plate, the anterolateral approach is used.
The posterior surface is accessed with a posterior approach.
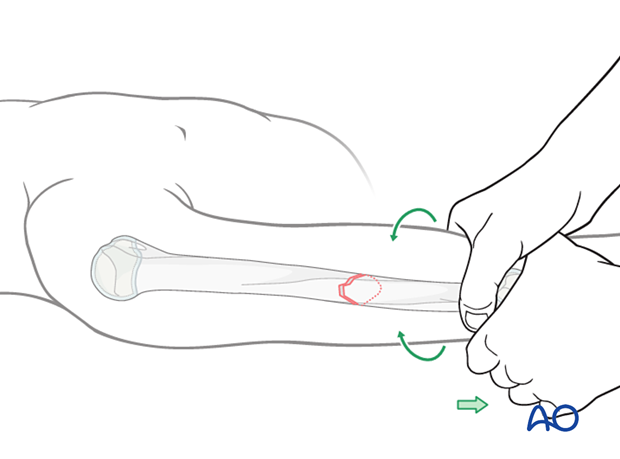
4. Reduction
Reduce the fracture with traction and manipulation and hold it with reduction forceps, placed to accommodate subsequent plate application.
The plate can be used as a reduction aid.
5. Plate fixation
Plate contouring
If a DCP is used, the plate should be contoured to match the anatomy of the bone and some overbending is required for compression.
This is not required if an LCP is used.
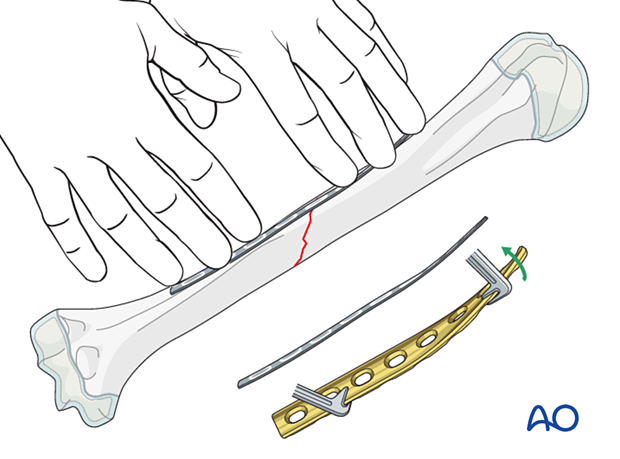
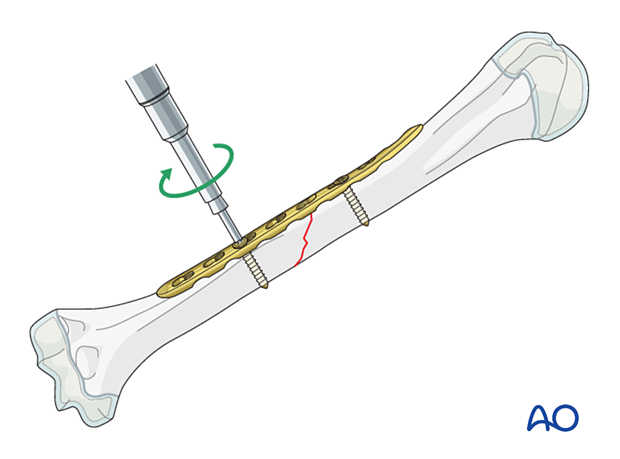
Plate application
Apply the plate in a standard manner, avoiding periosteal stripping.
For more details on compression plating, see the following basic technique:
Additional lag screw
An additional lag screw may be inserted through the plate if the obliquity of the fracture allows. The plate should be positioned to allow for optimal lag screw fixation.
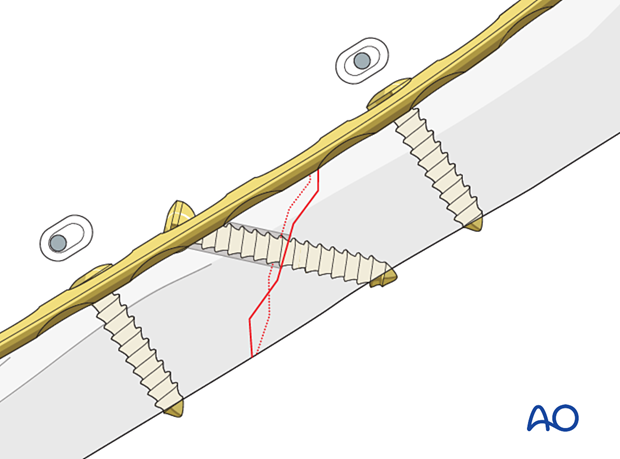
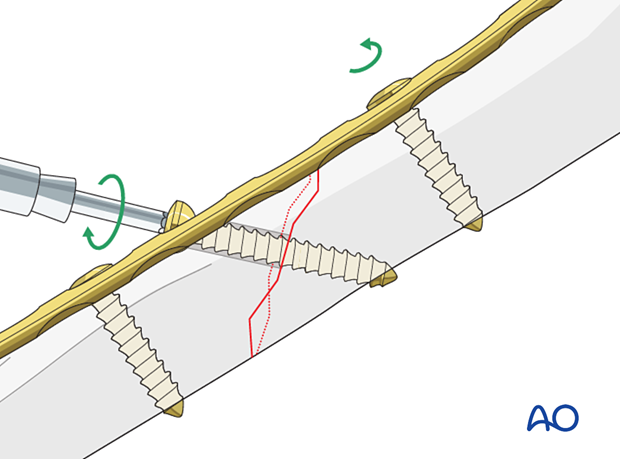
The insertion follows the principles of lag screw fixation:
- Drilling a pilot hole through both cortices
- Overdrilling the near cortex for gliding hole
- Tapping the far cortex for non-self-tapping screws
Retighten the loosened screw after tightening of the lag screw.
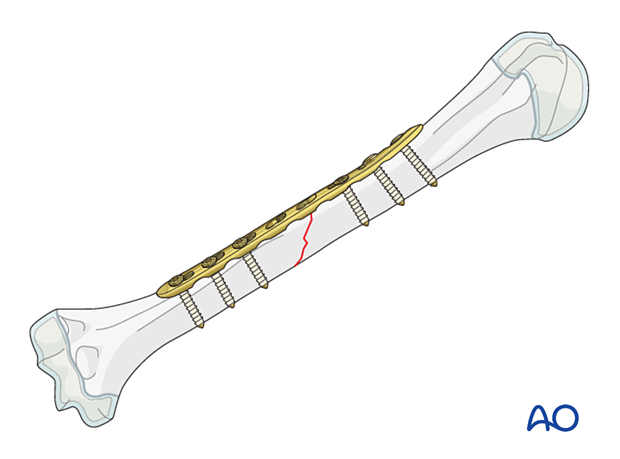
Finalizing the fixation
Insert the remaining screws.
6. Aftercare
Initial postoperative treatment
A sling may be used initially, but early mobilization is recommended.
Follow-up
The first clinical and radiological follow-up is usually undertaken within 2 weeks.
X-rays are repeated after 6 weeks.
Implant removal
Implant removal is not mandatory and is associated with a high risk of radial nerve injury.













