Plating principles in pediatric fracture care
1. Introduction
Indications for plate application in pediatric patients
The indications for the use of plates in pediatric fracture management are more specific than in adults. Plating is rarely indicated in children under the age of 5 years.
This is due to considerations including:
- Bone biology, eg, modeling
- Fracture biology, eg, rapid healing
- Preservation of the physis
- Alternative techniques including nonoperative management and elastic nailing
Relative indications if alternative techniques or image intensifier are not available:
- Polytrauma
- Length unstable fractures
- Metadiaphyseal fractures
The indications for management of metadiaphyseal fractures in adolescents close to skeletal maturity with closed growth plates are identical to adult patients.
Plating modalities
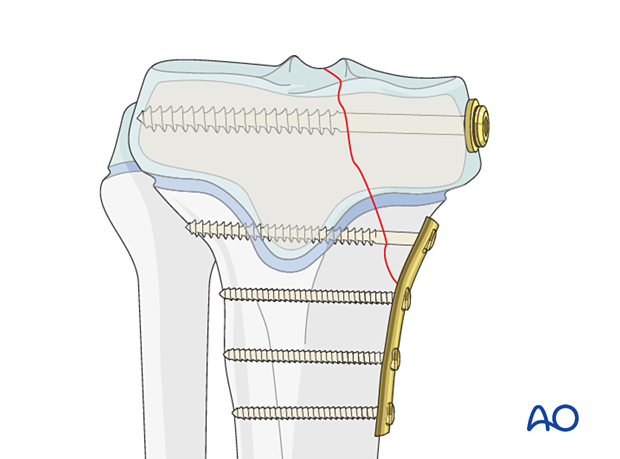
Care should be taken to preserve the growth plate when plating in the metadiaphyseal region.
Plates may be applied in various modes according to the function required. These include:
- Protection (neutralization)
- Compression
- Bridging
- Buttress (antiglide)
- MIPO
Plate designs
Anatomical plates are available for use in adolescents, and reconstruction plates can be contoured to conform to specific locations in smaller patients.
Plates ranging between 2.0 to 4.5 mm are typically used in pediatric practice.
The age and weight of the patient, the anatomical site and the load to which they will be subjected will dictate the size of the implant.
Plates are available for use with locking and/or non-locking screws and can be used to facilitate dynamic compression.
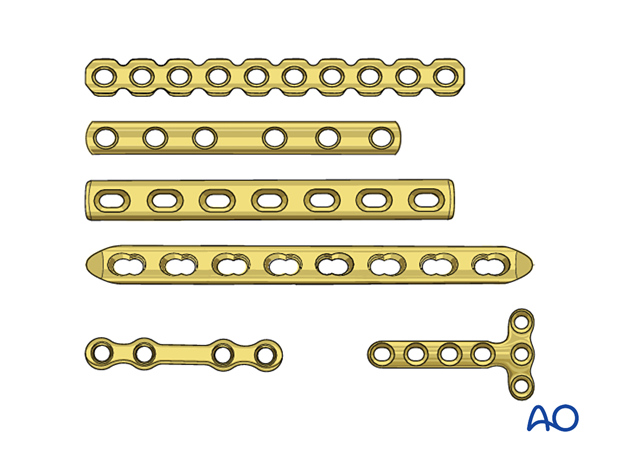
Plate contouring
The plate must conform to the shape of the bone unless locking screws are used as this construct remains stable even if the plate is not in direct contact with the bone.
Most long bones have a metaphyseal flare, and plates usually need to be contoured to reduce their offset.
The use of a flexible template can facilitate plate contouring.
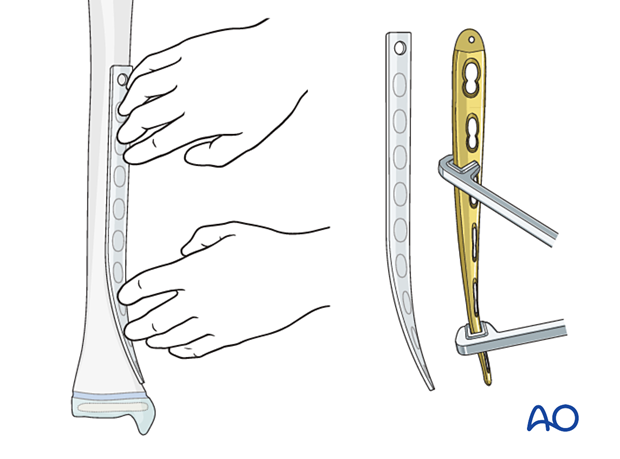
Anatomic plates are designed to conform to a specific region, but additional contouring may be required.
2. Plating near or across the growth plate
If a plate is applied near or across the physis, pressure on the perichondral ring should be avoided. This can be achieved with locking screws or an offset plate.
In younger patients, the plate can be deliberately offset by inserting a periosteal elevator beneath the plate prior to screw tightening.
Screws should be placed as far as possible from, and should not cross, the physis.
If the plate bridges the physis, the remaining growth may be disturbed. This is only recommended if there is minimal growth remaining or severe comminution requiring additional stability.
Unless there is negligible residual growth, plate removal is advisable as soon as there is radiological evidence of stable fracture healing. This is to prevent growth disturbance either by direct compression of the perichondral ring or indirect compression of the physis.
3. Protection (neutralization) plates
Function
A protection plate neutralizes bending and rotational forces to protect a lag screw.
This applies to plates with locking or nonlocking screws.
Application
The fracture is reduced and stabilized with one or more lag screws.
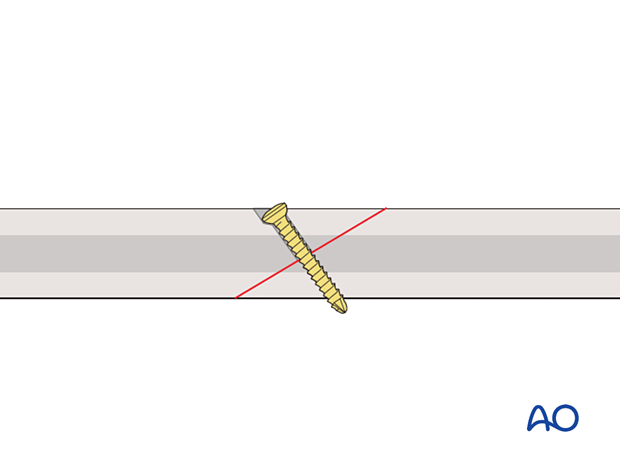
This 3D model shows application of a lag screw.
A lag screw placed perpendicular to the fracture plane is used to achieve optimal compression of fracture surfaces in a simple fracture. If this optimal orientation is not achieved, then a malreduction will be induced. Lag screws can provide useful compression to enhance fracture plane contact and hence healing, but the fracture plane is not stable when a bending or torsional force is applied. Resistance to bending or torsional forces is provided by a neutralization (protection) plate.
An appropriately contoured plate is applied to the bone, and the screws are inserted in a neutral mode.
Depending on the plate design, bone quality, implant availability, and surgeon’s preference, fixed-angle locking head screws, variable angle locking head screws, or nonlocking screws may be inserted.
Screws are inserted to obtain sufficient hold to maintain reduction until the fracture heals. It is not necessary to fill every plate hole.
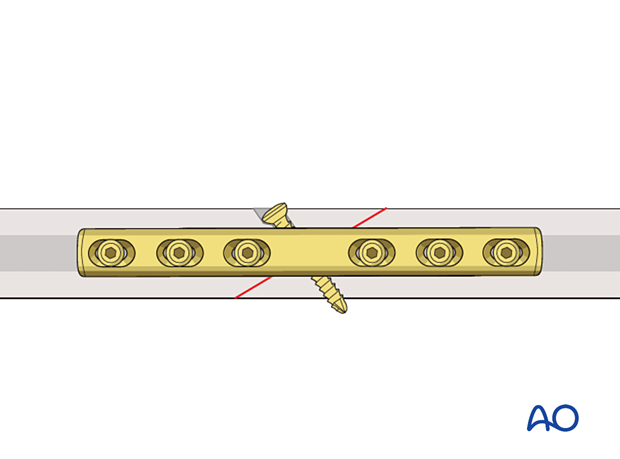
This 3D model shows a lag screw with a neutralization plate fixed in an orthogonal orientation to the screw.
By placing the neutralization plate in a plane rotated 90° to the plane of the lag screw, torsion and bending forces acting on the screw are reduced. The overall stability of the construct is increased.
4. Compression plating
Function
The plate produces compression at the fracture site to provide absolute stability.
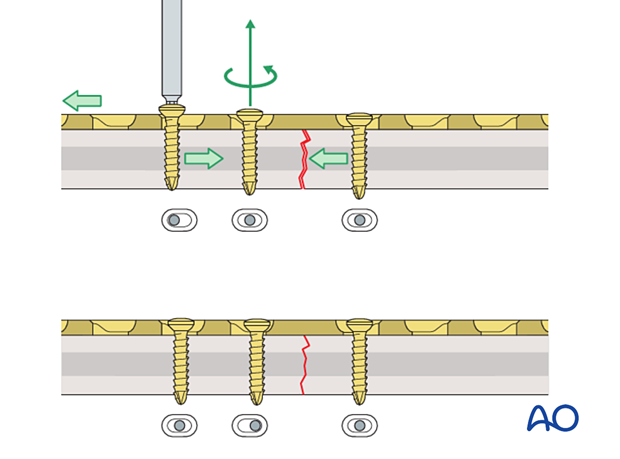
Plate application to transverse fractures
ReductionIf possible, the fracture is reduced and temporarily fixed with reduction forceps. Place the forceps such that they will not interfere with the planned plate position.
If the plate is exactly contoured to the anatomically reduced fracture surface, there will be some gapping of the far cortex when the plate is tensioned by tightening the load screw.
This 3D model shows a screw inserted in compression mode with an unbent plate.
When a transverse fracture is compressed with a plate that is not overbent but exactly pre-contoured to the reduced fracture surface (bottom panel), compression will first be exerted at the cortex under the plate (near cortex). The cortex opposite the plate (far cortex) will open resulting in a fracture gap. This may lead to delayed union of the far cortex.
The solution to this problem is to contour the plate so that its center is elevated 1–2 mm from the anatomically reduced fracture surface.
The apex should lie directly over the fracture line.
When the first screw is inserted, slight gapping of the cortex will occur directly underneath the plate. After the fixation is complete, the plate will be in contact with the bone throughout its length, but it is acting as a spring, providing compression at the far cortex.
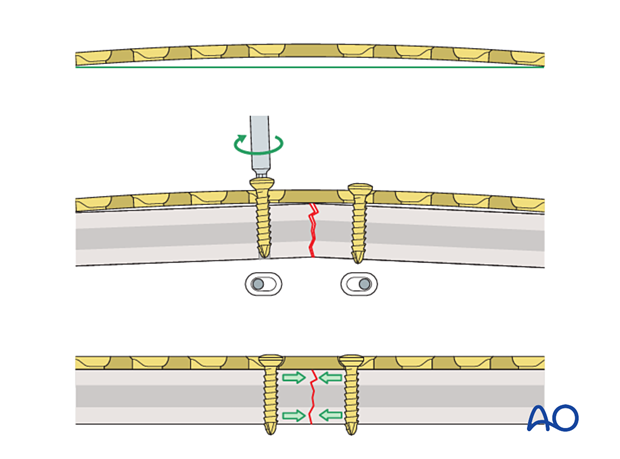
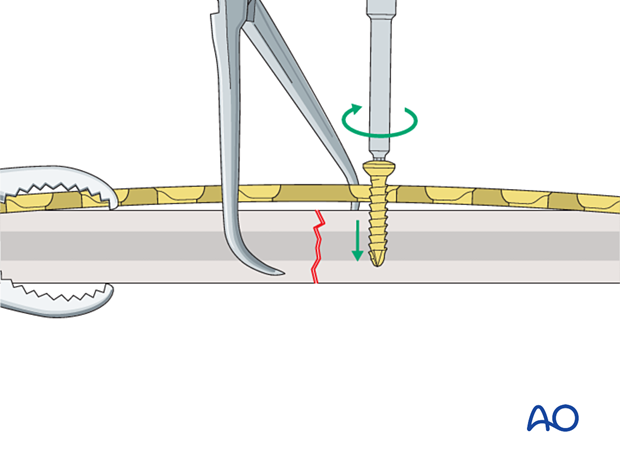
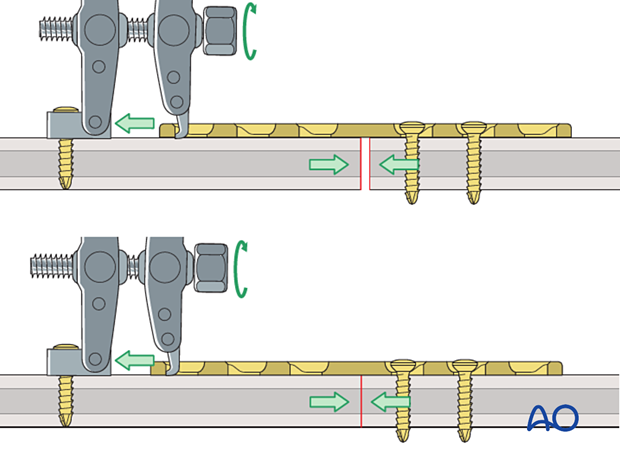
The prebent plate is fixed to one of the main fragments with a screw inserted in compression mode. Reduction forceps are placed on the opposite fragment to hold it in the reduced position against the plate. The screw is not fully tightened.
More information about screw insertion in compression mode is provided here.
This 3D model shows screw insertion in compression mode with an overbent plate (Step 1).
To compress both the near and opposite (far) cortices, the plate should be slightly overbent before application, resulting in a convex shape, so there is a small gap between plate and bone at the fracture. Before the screws are inserted, the fracture is reduced. With the insertion of the first screw eccentrically in the screw hole, the overbent plate is pressed onto one bone fragment which causes slight displacement of the reduced fracture. The displaced fragment will be relocated with the insertion of the second screw in compression mode.
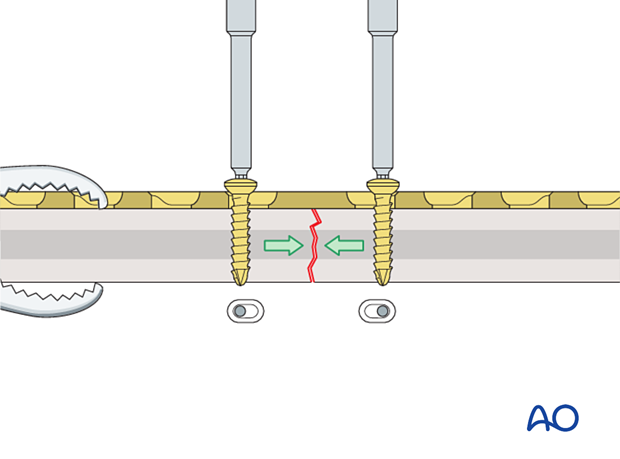
A screw is inserted in compression mode in the opposite fragment. To maintain reduction, it is recommended that the screws are gradually tightened by alternating between the two sides.
This 3D model shows screw insertion in compression mode with an overbent plate (Step 2).
The displaced fragment is reduced with the insertion of the second screw eccentrically in compression mode, straightening the plate and closing the gap at both the near and far cortices.
These 3D models show that locking head screws cannot be used for compression. The bottom panel shows that locking head screws cannot be inserted eccentrically in compression mode, unlike conventional screws (top panel).
If a fracture gap remains after insertion of the two compression screws, a third screw can be inserted in compression mode on either side. Before this screw is tightened, the compression screw already placed in the same fragment needs to be loosened. After the third screw is fully tightened, the first screw is retightened, and additional screws are inserted in neutral mode.
Application of dynamic compression plate to transverse fractures
Plate application to oblique fractures
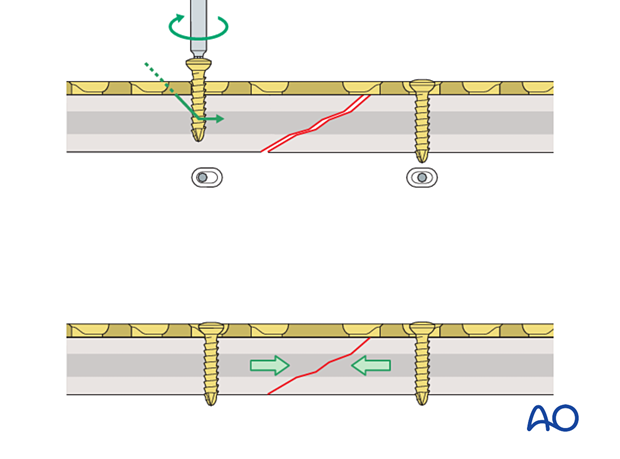
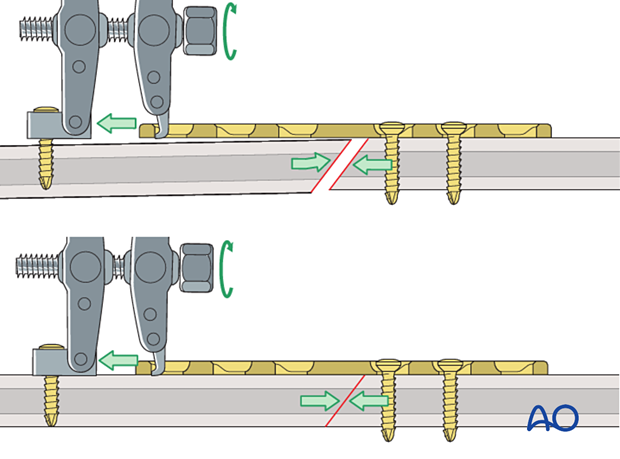
In oblique fractures, the plate is placed with one or more screws inserted in neutral mode to create an axilla with one of the bone segments.
Information about screw insertion in neutral mode is provided here.
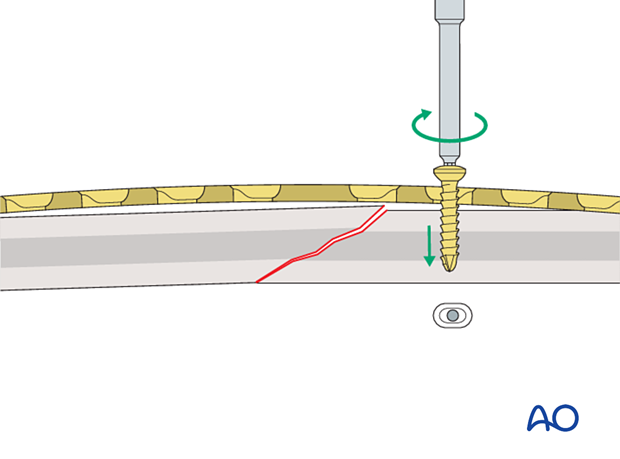
This 3D model shows screw insertion in neutral mode.
In oblique fractures, first the plate is placed and fixed with one or more screws inserted in neutral mode into the first fragment.
Application of dynamic compression plate to oblique fractures
A screw is inserted in compression mode into the second fragment. This drives the second fragment into the axilla and compresses the fracture.
This 3D model shows screw insertion in compression mode.
When inserting a screw in compression mode into the second (mobile) fragment, the fragment is driven into the angle formed by the fracture plane of the fixed (static) fragment and the undersurface of the plate (this is known as the axilla, highlighted in green) and the fracture is compressed.
If the plate is applied in an oblique fracture without creating an axilla, as the fracture is compressed, the fracture may displace.
If the plate is applied to an oblique fracture without creating an axilla then, when a screw is applied in compression mode, the fracture may displace. The apex of the mobile fragment is not “captured” by an axilla.
For the axilla concept to be applied:
- the plate must be orientated so that the direction of applied (compressive) force is co-aligned with the neutral axis of the bone
- the plane of the fracture must be close to perpendicular to the applied force
- the plate should be placed over the apex of the mobile fracture fragment
If the fracture pattern and location do not allow the plate to be applied to create an axilla, applying a lag screw and a neutralization plate may be better.
An interfragmentary lag screw can, in some cases, be inserted through the plate for additional compression.
Information about lag screw insertion is provided here.
These 3D models show a lag screw with a neutralization plate rotated 90° and aligned with it.
A neutralization plate can reduce the stresses on the lag screw. However, the positioning of the plate has only a minor influence on the screw, as demonstrated by the models.
Here compressive stress is shown in red and tensile stress is shown in blue.
Articulated tension device
As an alternative, the articulated tension device may be used to provide mechanical compression prior to fixation of simple fractures.
The device may also be used to create distraction as part of a reduction maneuver.
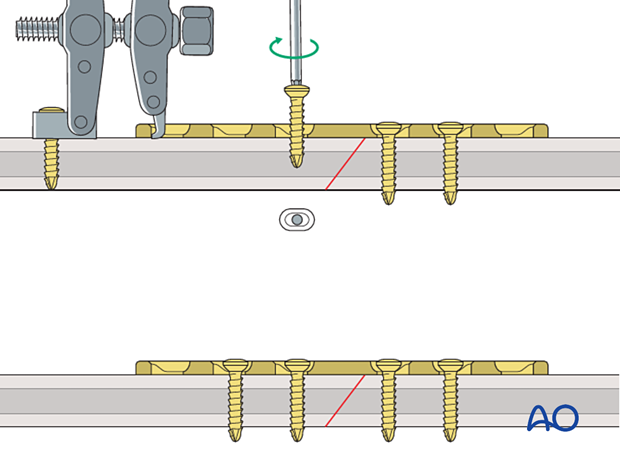
The fracture is approximately reduced, and a plate is securely attached to one fragment.
The device is anchored to the bone with a screw inserted through the articulated footplate and the hook on the device inserted into the hole at the end of the plate.
As the tensioning screw is tightened, the two limbs of the device are pulled together, and compression is achieved at the fracture site.
In oblique fractures, the plate should be applied to create an axilla following the same principle described above for dynamic compression plates.
Screws are inserted into the second segment in neutral mode and the device removed.
To distract the fracture, the hook of the device is placed against the plate end, and the tensioning screw on the device is turned counterclockwise.
The device is then used to compress the fracture as described above.
5. Bridge plate
Function
Bridge plating techniques are used for multifragmentary long bone fractures where intramedullary nailing or conventional plate fixation is not suitable. Bridge plates are often inserted through a minimally invasive approach (see below) to avoid disruption of the fracture site. An open approach may be necessary for irreducible fractures.
The plate provides relative stability by fixation of the two main fragments, achieving correct length, alignment, and rotation. The fracture site is left undisturbed, promoting fracture healing by callus formation.
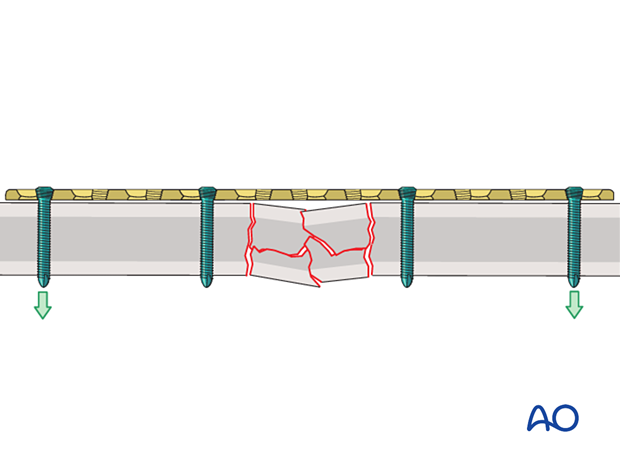
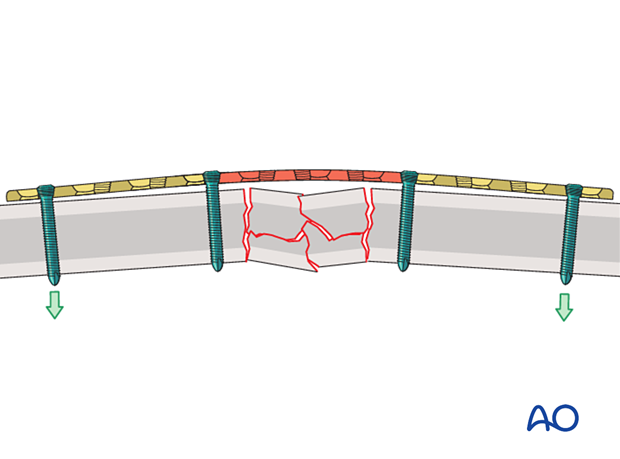
Working length
Plates with a long working length distribute bending stresses over a long segment, and the stress per unit area is correspondingly low. This prevents high stress over the fracture site and reduces the risk of plate failure.
Long plates also produce a long lever arm, which reduces the risk of screw pullout.
Conventional vs locking head screws
The plate is fixed to the bone using either conventional screws inserted in neutral mode or locking head screws.
The advantages of locking head screws compared to conventional screws are:
- The plate does not need to be perfectly contoured to the bone
- The periosteum is not compressed by the plate
- The risk of screw pullout and over-tightening is reduced
- The construct provides angular stability
- Unicortical screws may be used
These 3D models show the insertion of a locking head screw (top panel) and a conventional screw in neutral mode (bottom panel).
The conventional screw is inserted in neutral mode and pulls the plate against the bone. Locking head screws engage in the plate using the threads and therefore the plate is not pressed against the bone.
These 3D models allow bending of locking head screws and conventional screws to be simulated.
The fixed angle locking construct (bottom panel) provides considerable stability and there is bending of both the screw and the plate. In contrast, the conventional screw (top panel) can freely rotate in its plate hole without causing deformation.
High stress is shown in red and low stress is shown in green.
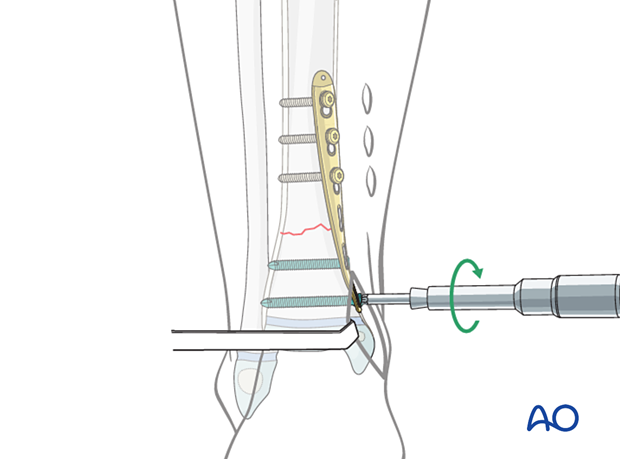
6. Minimally invasive plate osteosynthesis (MIPO)
Extent of surgical approach
Bridge plates are often inserted through a minimally invasive approach to avoid disruption of the fracture site.
Screws are either inserted through a stab incision or limited approach.
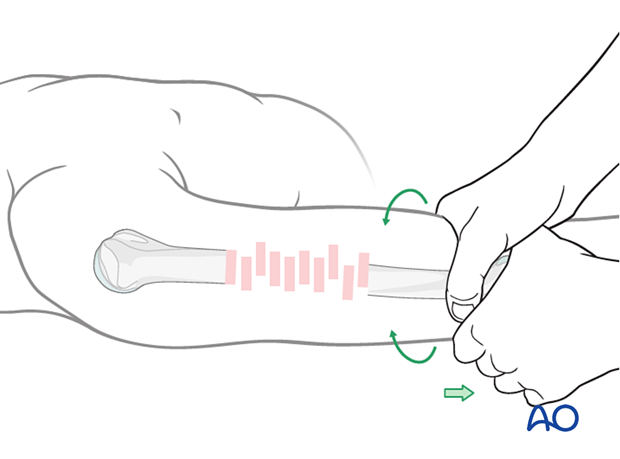
Reduction
Length, alignment, and rotation are corrected, and the main proximal and distal fragments are secured.
This is typically achieved with indirect reduction techniques including:
- Traction
- Temporary external fixation
- Reduction devices
This allows manipulation of the main fragments without opening the fracture site, preventing further soft-tissue injury.
An external fixator, or distractor, can provide alignment and temporary stability for bridge plating without disturbing the soft tissues at the fracture zone.
The position of the Schanz screws should not interfere with the plate application.
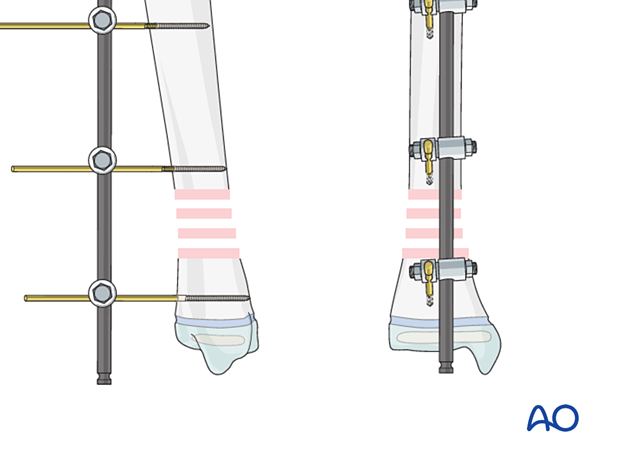
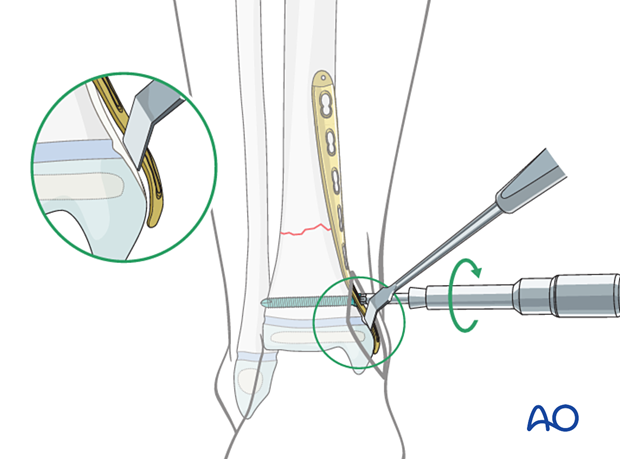
Plate insertion
The position of the plate and the MIO approach depends on the anatomical region.
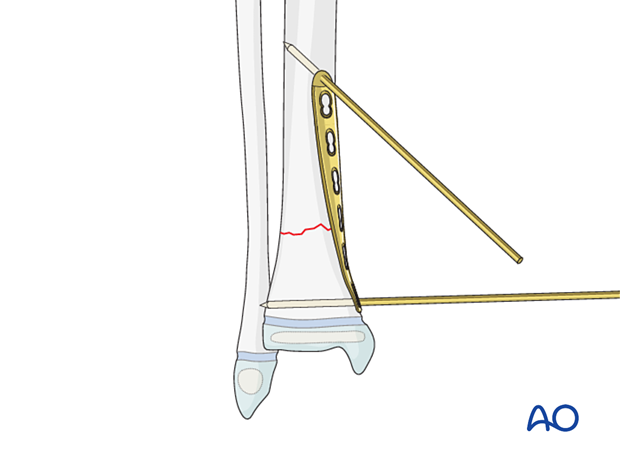
A submuscular tunnel is created with the plate or a periosteal elevator.
Some plate contouring may be necessary.
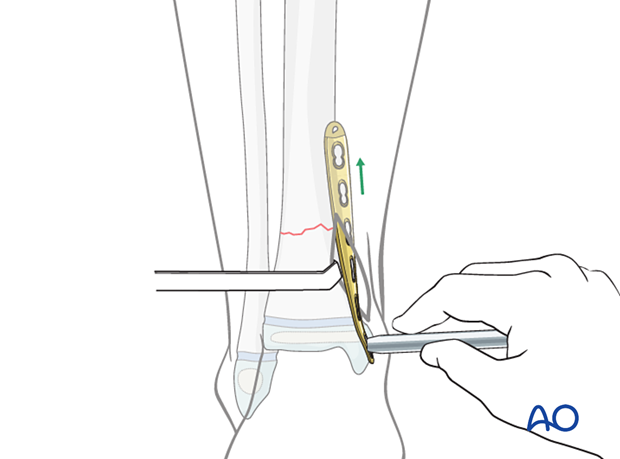
Plate fixation
The pate may be initially secured with K-wires inserted through pilot holes.
The sequence of screw insertion depends on the fracture configuration and anatomical region.
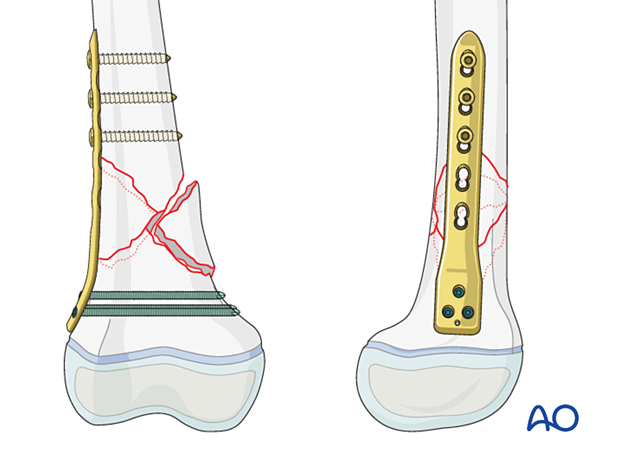
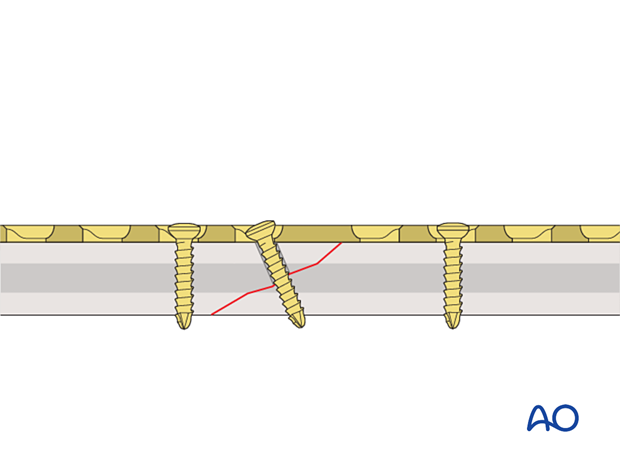
7. Buttress (antiglide) plate
Function
If the fracture morphology allows, a buttress plate may be applied as the primary stabilization device.
Buttress plates may be used to supplement lag screw fixation of epimetaphyseal fractures.
The lag screws may be inserted either through or separate from the buttress plate, preserving the growth plate.
Application
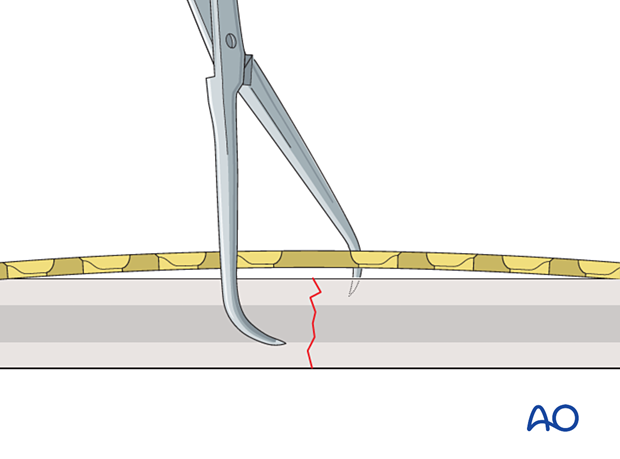
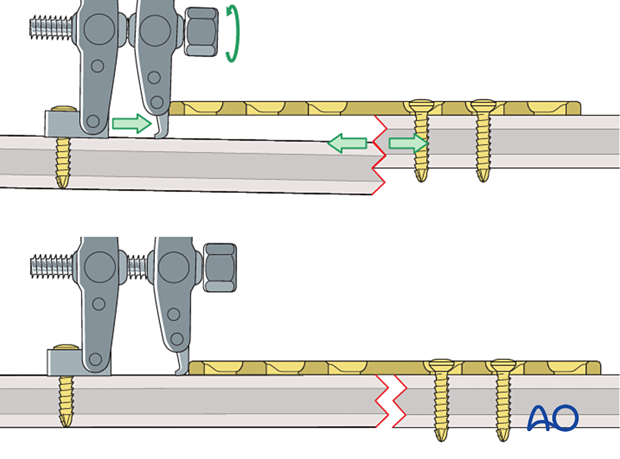
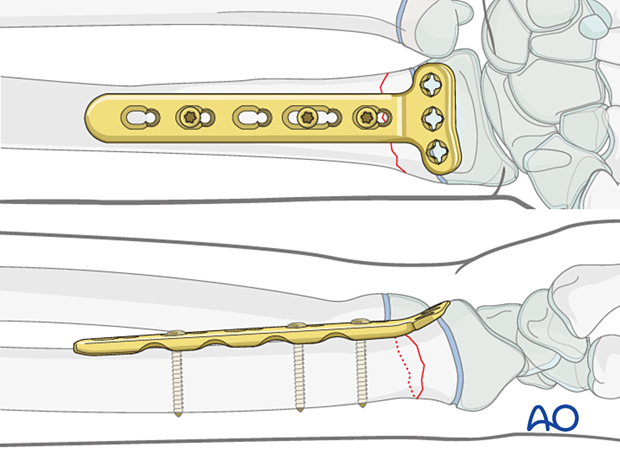
The fracture is reduced and stabilized with one or more lag screws following a standard technique.
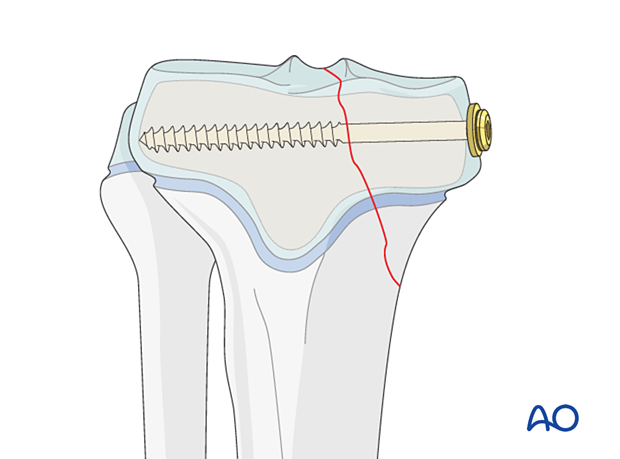
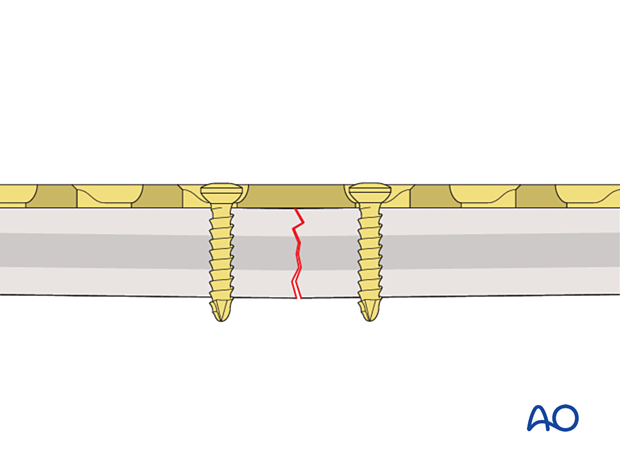
The plate is contoured, leaving a small gap between the central part and the bone.
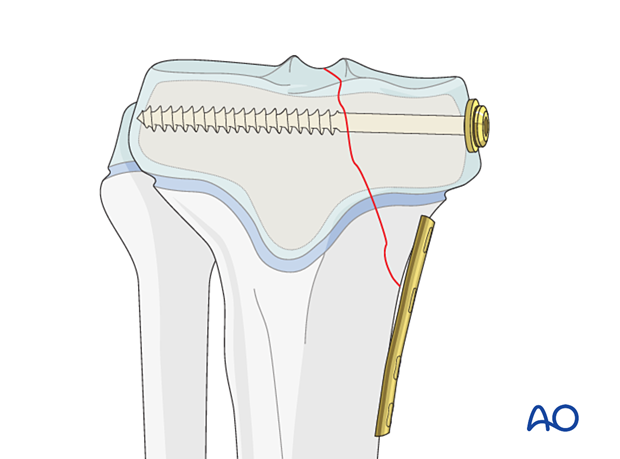
The plate is applied, and a bicortical screw is inserted in the hole closest to the fracture.
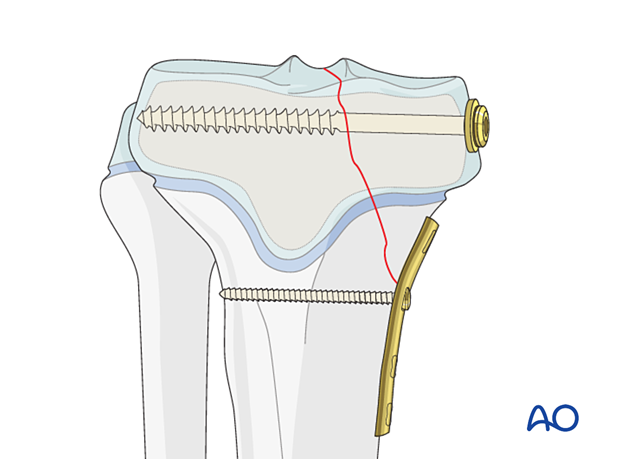
The buttress plate is secured with additional bicortical screws, inserted in neutral mode.