Lag screws
1. Principles
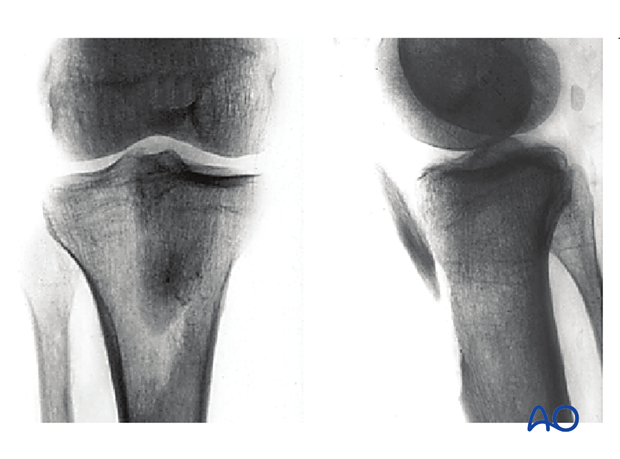
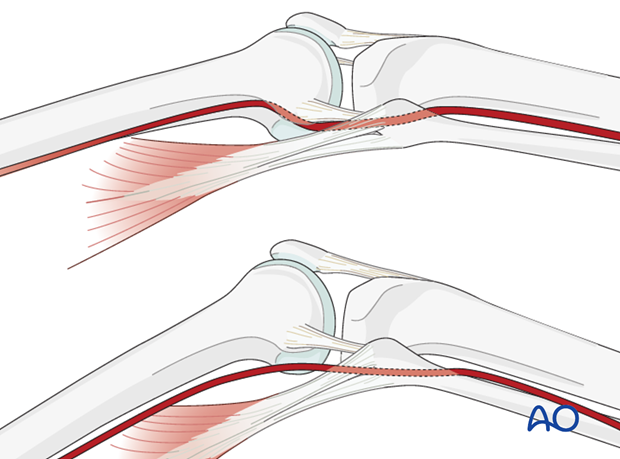
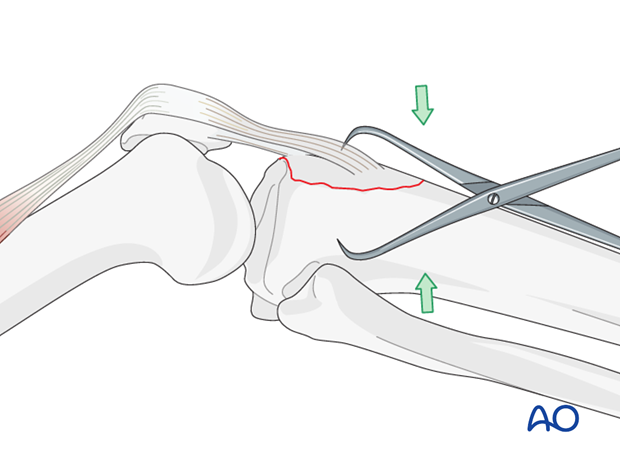
Pulling force of the patellar tendon
Due to the pulling force of the patellar tendon most of these fractures are displaced as shown here and need to be reduced. Reduction may be achieved by extending the knee. If this is not enough consider pushing the fragment into place with a ball-spiked pusher.
Reduction is not necessary in undisplaced fractures.
Knee flexion
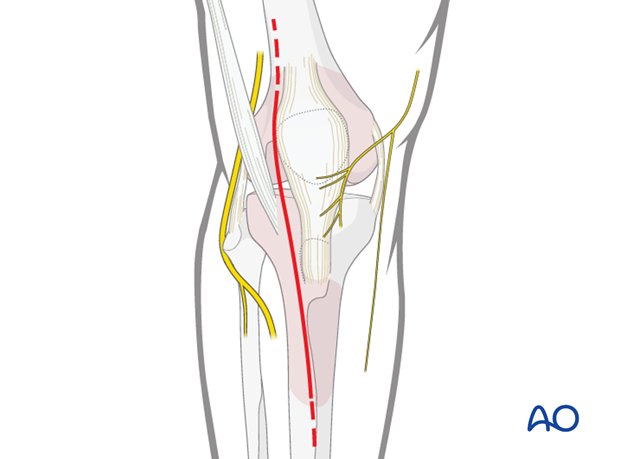
To lessen the possibility of damaging the popliteal neurovascular structures when you drill the proximal tibia in an anteroposterior direction flex the knee at least 15-20 degrees. In full extension the neurovascular bundle is closer to the bone.
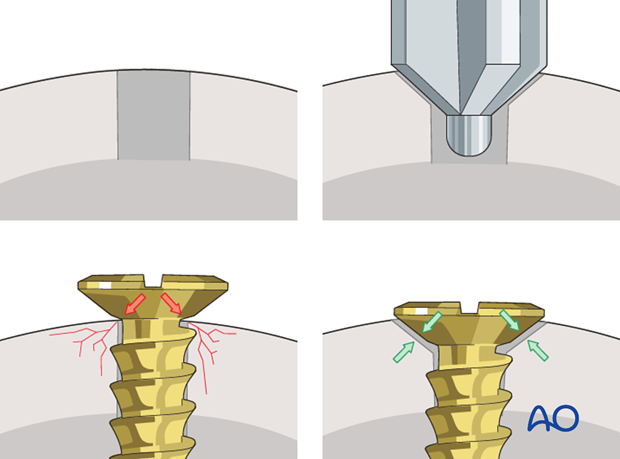
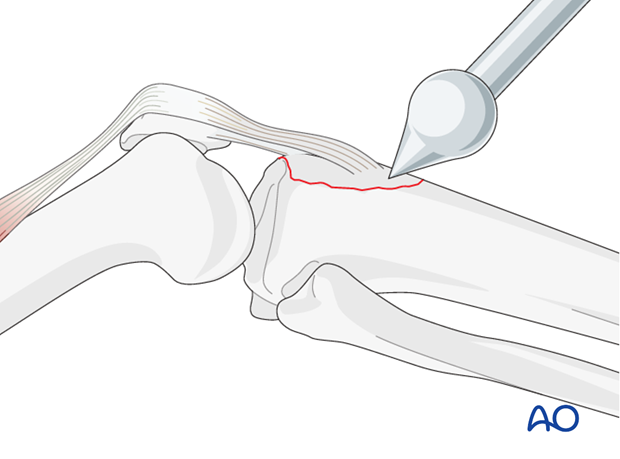
Countersinking
There are two important reasons for countersinking:
- To produce a lower profile of the screw head and thus avoiding soft-tissue irritation.
- Countersinking also ensures that the screw head has a maximum contact area with the bone, which leads to an even distribution of forces between the screw head and bone.
2. Patient preparation and approach
Patient preparation
This procedure is normally performed with the patient in a supine position.
Approach
For this procedure an anterolateral approach is used.
3. Open reduction
Use of clamp
After direct exposure of the avulsed tibial tuberosity in an open procedure, reduction may be achieved by using a small clamp placed on the anterior tibial cortex and the bone fragment. The reduction may additionally be secured by temporary K-wires.
Alternative: ball-spiked pusher
A ball-spiked pusher might also be used for the reduction.
4. Fixation
Lag screw application
Fixation of the tibial tuberosity is achieved by lag screw fixation in an anterior–posterior direction through the main fragment.
Cancellous screws are better in younger patients with solid cancellous bone. These screws are usually left in place after fracture healing.
In elderly people with osteopenia fully threaded screws should be used. Perforation of the posterior tibial cortex should be limited and visualized under image intensifier to avoid damage of nerves and vessels in the popliteal fossa.
Click here for further details on lag screw application.
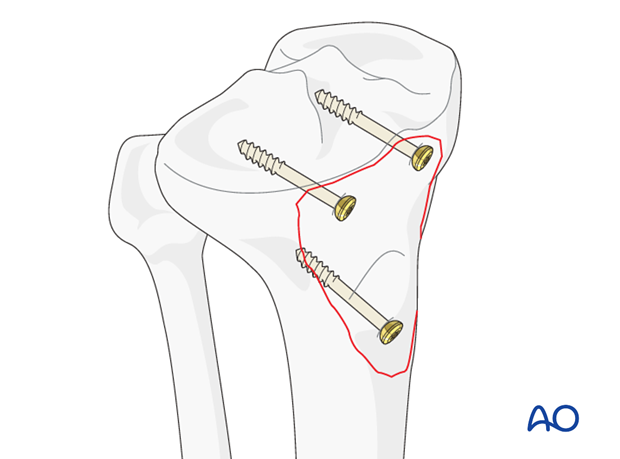
One should never rely on the lag screw fixation alone since the heads of the screws could easily cut out through the bone and fixation would be lost. Therefore, protect your lag screw fixation with a neutralizing cerclage wire as illustrated.
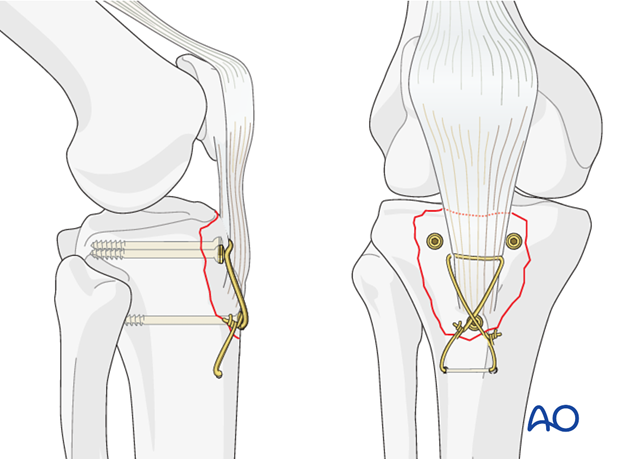
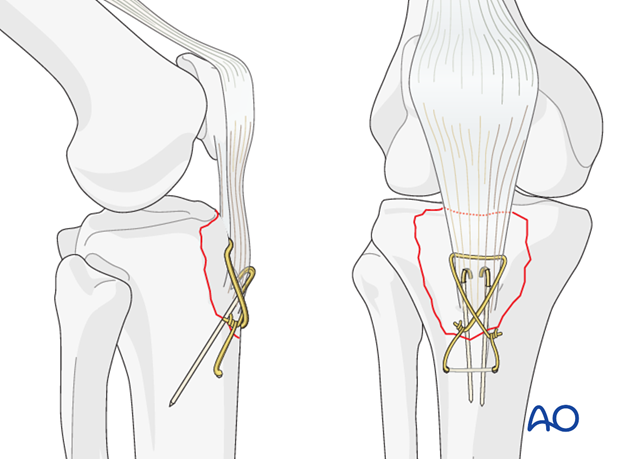
Alternative: cerclage compression wiring
A safe alternative in case of relatively small tibial tuberosity fragment or in case of comminuted fractures is cerclage compression wiring.
The cerclage wire is introduced through the Sharpey's fibers at the insertion of the patella ligament in the tibial tuberosity. K-wires provide rotational stability, are introduced through the proximal part of the tibial tuberosity and should engage the posterior cortex of the tibia.
Note: “Cerclage compression wiring” was referred to as “Tension band fixation”. We now prefer the term “Cerclage compression wiring” because the tension band mechanism cannot be applied consistently to each component of the fracture fixation. An explanation of the limits of the Tension band mechanism/principle can be found here.
5. Aftercare
If there is any doubt as to the security of the fixation, the limb should be immobilized in a cylinder cast for six weeks.
The neurovascular status of the extremity must be carefully monitored. Impaired blood supply or developing neurological loss must be investigated as an emergency and dealt with expediently.
Functional treatment
Functional treatment shall be applied for 2 – 3 days with patient still resting in bed starting on postoperative day 1. Apply a cylinder cast from postoperative day 3 on for a period of eight weeks.
The goal of early active and passive range of motion is to achieve a full range of motion within the first 4 – 6 weeks. Maximum stability is achieved at the time of surgery. A delay beyond a few days to allow swelling to subside is illogical and harmful.
Weight bearing
A hinged brace is used with non-weight bearing for 6 weeks.
Follow up
Wound healing should be assessed on a short term basis within the first two weeks. Subsequently a 8 week follow-up is usually performed.
Implant removal
Implant removal is not mandatory and should be discussed with the patient.













