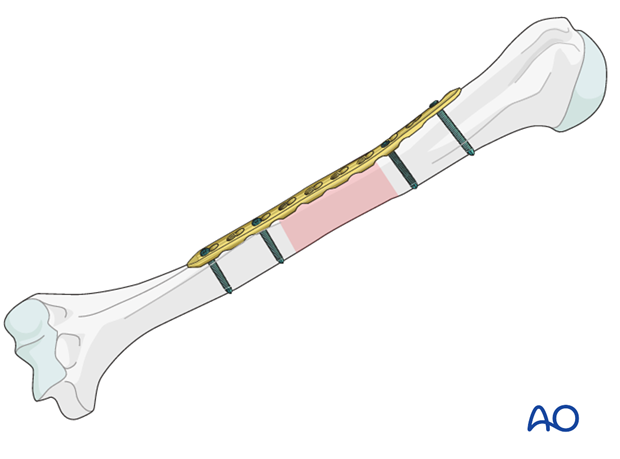
ORIF - Bridge plating (middle 1/3)
1. Principles
Bridge plating
Bridge plating uses the plate as an extramedullary splint, fixed to the two main fragments, while the intermediate fracture zone is left untouched. Anatomic reduction of the shaft fragments is not necessary. Furthermore, direct manipulation risks disturbing the blood supply. If the soft-tissue attachments are preserved, and the fragments are relatively well aligned, healing is predictable.
Reduction can usually be achieved indirectly using distraction.
Mechanical stability, provided by the bridging plate, is adequate for indirect healing (callus formation). Occasionally, a larger wedge fragment might be approximated to the main fragments with a lag screw. Lag screws should be avoided when there is significant comminution.
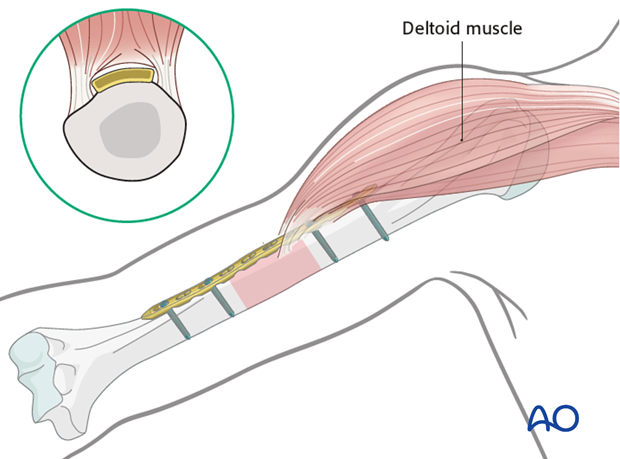
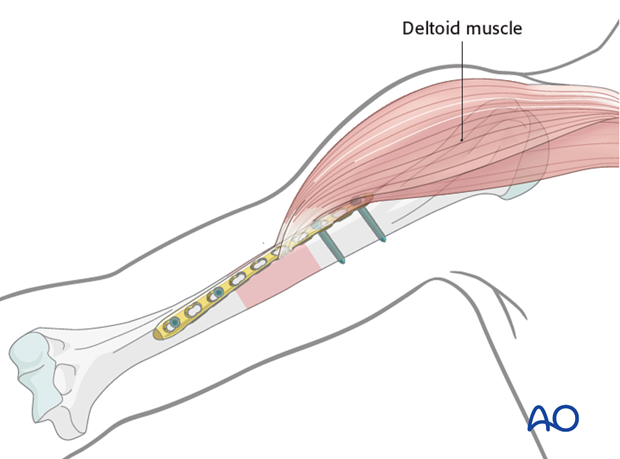
To illustrate the principles of bridge plating in humeral shaft fractures, the anterolateral plate application through an anterolateral approach is described. The application of a posterior plate follows the same principles.
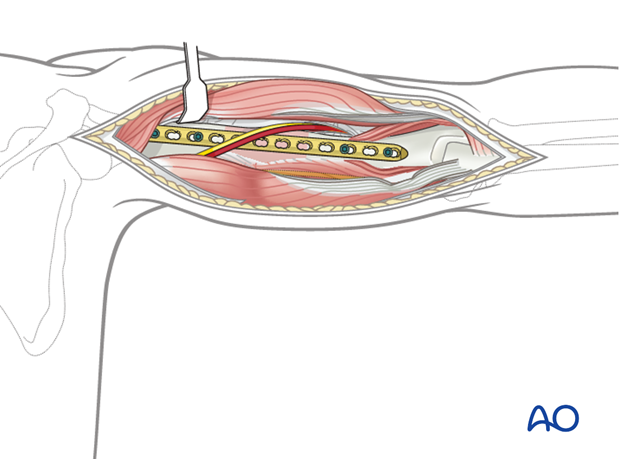
Bridge plate insertion
With open bridge plating, it is important to preserve soft-tissue attachments to the fracture fragments. To do this, stable provisional reduction (with external fixation, large distractor, or maintained manual traction), and minimal exposure and manipulation of the fracture zone are important. The bridge plate is applied through an incision just long enough for the plate.
Open fractures in the humeral shaft
Adequate surgical debridement is the crucial first step in the care of any open fracture.
Read more about the treatment of open fractures in the humeral shaft.
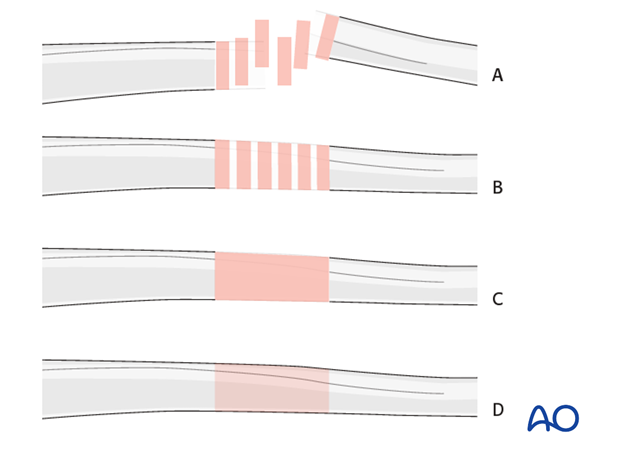
Note on illustrations
Throughout this treatment option illustrations of generic fracture patterns are shown, as four different types:
A) Unreduced fractureB) Reduced fracture
C) Fracture reduced and fixed provisionally
D) Fracture fixed definitively
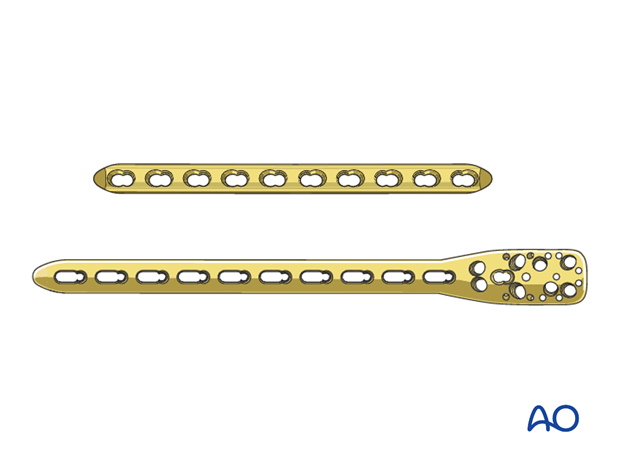
2. Choice of implant
Either a standard plate or a plate with locking head screws (LCP) can be used as a neutralization device. In poor quality bone the use of an LCP is recommended.
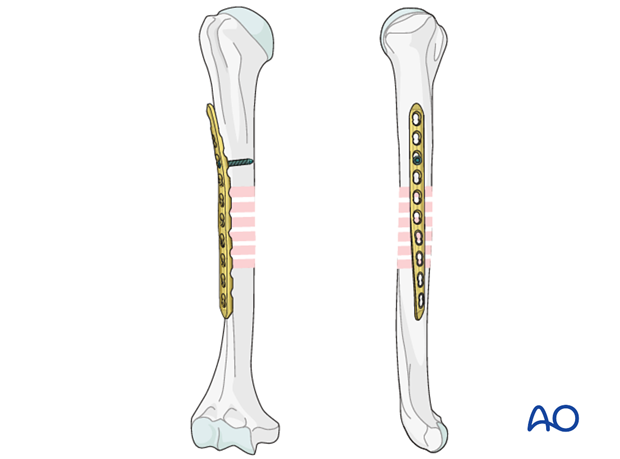
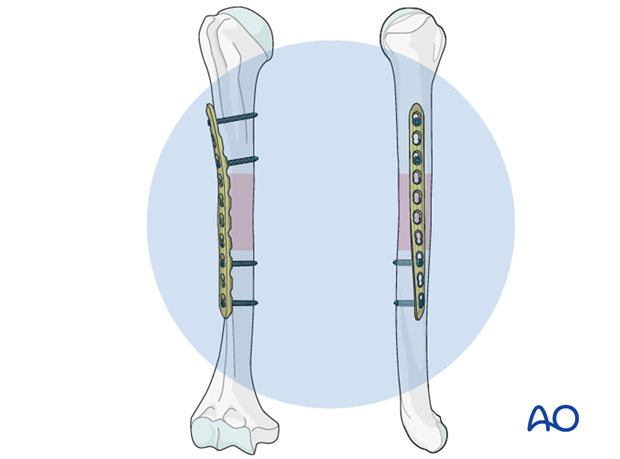
As bridge plating should span a long section of the bone, the length of the implant has to be chosen accordingly. It should be long enough to allow sufficient hold in the proximal and distal segments, generally a minimum of three bicortical screws in each. Typically, a ten or twelve-hole 3.5 mm LCP is sufficient. It is also possible to use a long PHILOS plate.
Longer plates are normally twisted to form a helix, so that the proximal end is applied to the lateral humerus while the distal end lies on the anterior surface.
3. Plate position
Introduction
The choice of plate position depends on the fracture morphology and location, the radial nerve pathology and the surgeon’s preference. The anterolateral, anterior, and posterior surfaces of the humeral shaft are all possible choices.
The medial surface is generally reserved for complex reconstructive procedures ie vascular repair in complex fractures. Since the use of this plate position is rare it is not further shown.
The location should allow sufficient plate length on both proximal and distal segments, with a minimum of three holes for each.
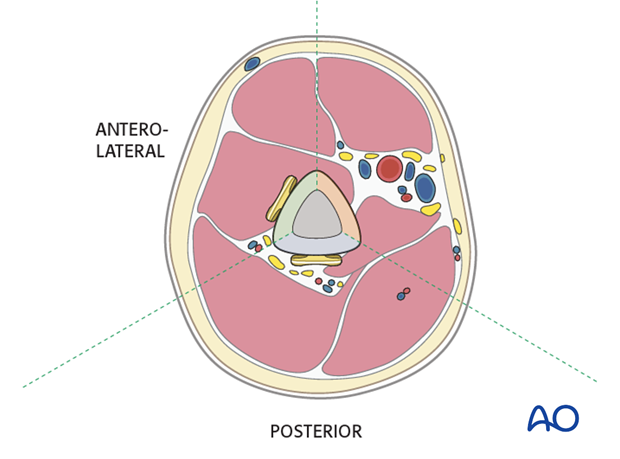
Anterolateral or anterior plate
An anterolateral plate fits well from very proximally to the distal fifth of the humerus and is selected if proximal and middle third fractures are present.
A plate in this position should provide stable fixation of the fracture and minimal soft-tissue damage.
Proximally, the plate may interfere with the deltoid insertion if it is placed laterally, or with the long head of the biceps tendon if the plate is positioned anteriorly. To overcome these problems the proximal end of the plate can be tunneled through the deltoid insertion.
Distally the plate may be applied to the anterior or lateral surfaces.
Depending on the chosen positions for the proximal and distal plate ends, the plate may need to be contoured and/or twisted to form a helix.
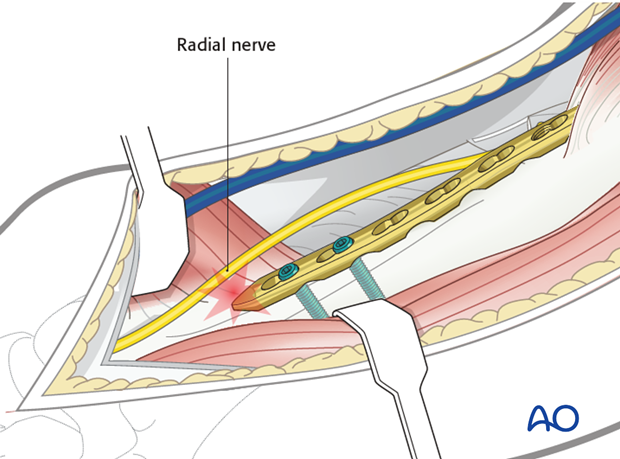
Neurological considerations should be taken into account. The radial nerve is at risk if the plate is applied to the lateral surface in the distal third. The plate should be twisted to ensure that the distal end avoids damaging the radial nerve.
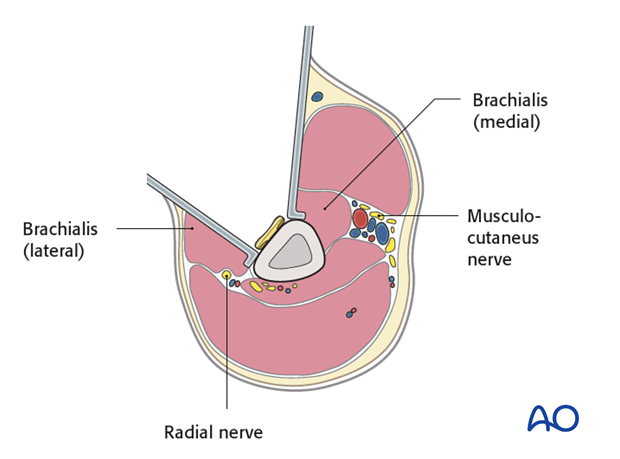
The innervation of the brachialis muscle is derived from both the radial and musculocutaneus nerves. The radial branch is at risk if the plate is applied to the anterior and anterolateral surfaces in the distal third while retracting the entire brachialis muscle medially. To avoid this it is safer to split the brachialis muscle.
If a small open fracture wound is present, the approach is made separately. Only if there is a large wound, after debridement, consider using the wound itself, with its necessary extensions, for plate insertion.
Posterior plate
The posterior surface is difficult to access proximally and limited by the axillary nerve. Therefore, posterior plating is best suited for middle and distal third fractures.
It is important to protect the radial nerve and its accompanying vessels in the spiral groove. If the plate interferes with the radial nerve, the plate must be placed underneath it. The course of the radial nerve in relation to the plate holes should be mentioned in the operation note. This will reduce the risk of accidental nerve damage if the plate should ever need to be removed.
4. Patient preparation and approaches
Patient positioning
Place the patient in a supine position or, alternatively, a beach chair position for placement of an anterolateral or anterior plate.
For placement of a posterior plate, a prone or lateral decubitus position is normally used.Approaches
The approach is selected depending on the chosen plate position.
For an anterolateral plate the anterolateral or extended deltopectoral approach may be used. For a more distal anterior or lateral plate, an anterolateral or lateral approach may be used.
The posterior surface can be accessed with a posterior approach (triceps-split or triceps-on approach).5. Reduction
It is important to restore axial alignment and rotation. A little shortening of 1 or 2 cm can be accepted in the humerus, and with extreme fragmentation may improve bone contact.
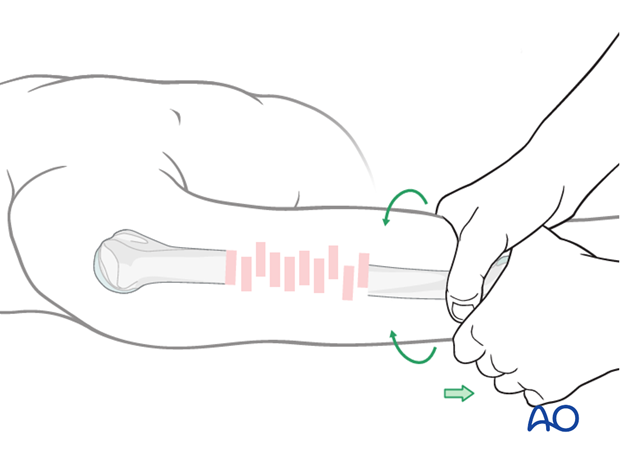
Manual reduction - limb realignment
Begin the reduction with traction on the distal humerus restoring bone length, tension in the soft tissues, realignment of the axis, and rotation.
Clear any interposed soft tissue by direct exposure. Preserve as much soft-tissue attachment as possible.
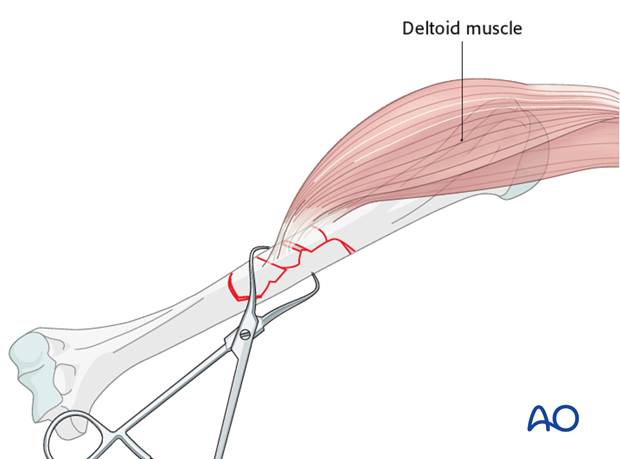
Pointed reduction forceps
When large fragments have significant muscle attachments, such as deltoid or pectoralis major insertion, they are often pulled away from the fracture zone. They should be reduced and held with reduction forceps while the plate is applied.
If there is concern that the fragment(s) will redisplace it may be secured with a screw or cerclage wire.
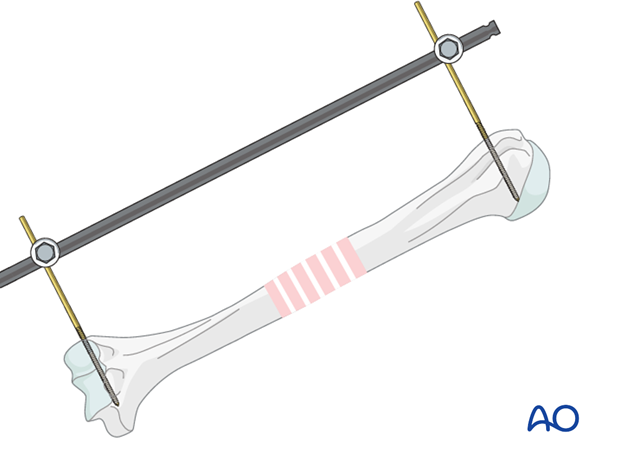
Reduction by external fixator or distractor
Particularly with comminuted fractures, use of an external fixator or distractor can provide alignment and stability for bridge plating without disturbing the soft tissues at the fracture site.
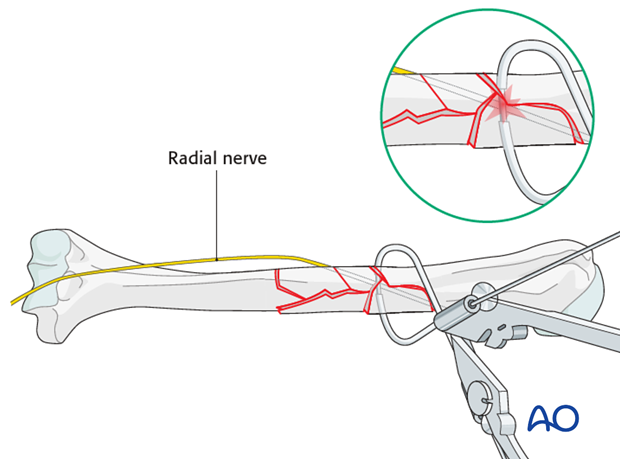
Insert proximal and distal pins outside the planned plate location. Take care not to injure the radial nerve. If in any doubt use incisions wide enough to allow palpation or direct visualization of the radial nerve.
Complete reduction may require additional correction of angulation or rotation. Folded linen bolsters under the fracture often help.
Comminuted fragments
Remember that alignment of comminuted fragments need not be anatomical, and that efforts to manipulate them often injure their blood supply.
Generally, soft-tissue attachments will bring these fragments into appropriate positions as the proximal and distal portions of the humerus are brought into correct alignment and fixed.
Occasionally, lag screws (through or outside a plate) or cerclage can be used to improve fracture fragment approximation. This option should be considered if important tendon insertions are still grossly displaced such as a fragment carrying the deltoid insertion and/or the pectoralis major/latissimus dorsi/teres major insertion. This helps to improve later clinical function.
If cerclage is used, take care not to injure the radial nerve. Keep the cerclage passer close to the bone. In any doubt, pass it under direct vision.
6. Plate fixation
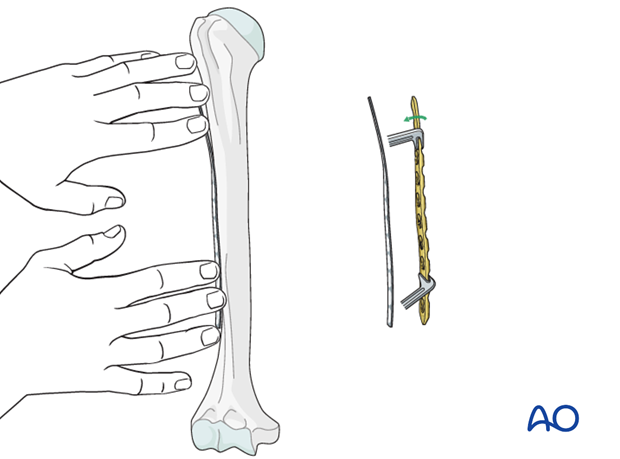
Contouring the plate
Depending on the planned plate location, some contouring of the plate is likely to be necessary to fit the plate to the bone perfectly so that tightening its screws does not displace the fracture. This is true distally, posteriorly, and also on the anterolateral surface centrally. Sometimes twisting the plate around the shaft of the humerus provides a better fit and allows a longer plate.
Shape a malleable template to the bone surface. Use this template as a guide to shape the plate to fit the bone.
Use care to avoid fracture displacement while contouring the plate.
Pitfall: avoid soft-tissue damage
During contouring and application of the bridge plate, the soft tissues attached to the fracture fragments must be preserved . Provisional fracture stabilization and minimal handling of the fracture site are the keys to this.
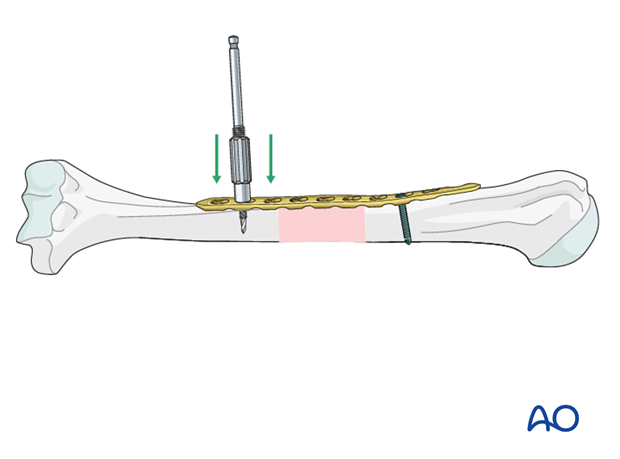
Plate application
Apply the properly contoured plate to the proximal fragment, so that it is correctly aligned with the humeral axis.
When the plate fits satisfactorily against the proximal fragment, attach it provisionally with a single bicortical nonlocking screw while holding it manually against the bone. Alternatively, a locking screw can be used at this moment if the reduction and plate position does not need further adjustment. Sometimes it is helpful to clamp the plate to the proximal fragment of the humerus with bone forceps.
Apply the plate to the distal fragment to correct rotation and axial alignment.
Check in the lateral view that the plate is parallel to the longitudinal axis of the humerus.
Alignment and fixation of the distal fragment
Once the plate is fixed proximally, bring the distal fragment into alignment against the plate.
Hold the plate manually against the bone and check reduction and plate position. If necessary, loosen the screw in the proximal fragment and adjust the plate position. Occasionally it is necessary to remove the plate and perform further contouring.
Once reduction and plate position are satisfactory insert a first distal screw.
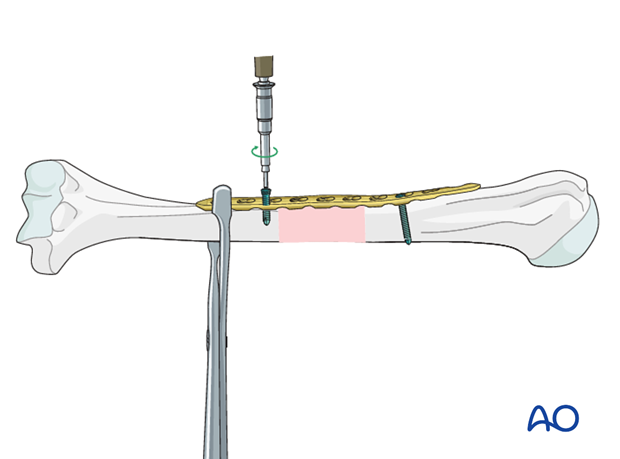
Sometimes it is helpful to clamp the plate to the humerus with bone forceps as shown. Carefully pass the forceps close against the bone during application to avoid injury to adjacent nerves.
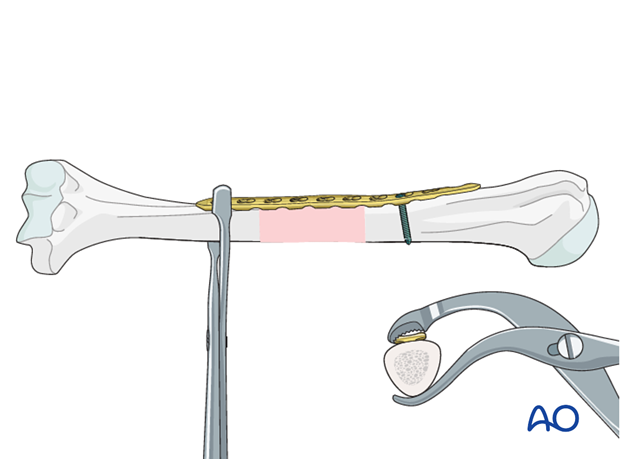
Another option is the use of the push-pull reduction device, from the LCP set, as shown here. Choose a hole which will not be used for final screw fixation.
Insert the first distal screw. Depending on the fixation technique either a nonlocking or a locking screw can be used near by the fracture site.
Finalizing the fixation
If the alignment is satisfactory, add the remaining screws to both main fragments and reconfirm alignment.
The number of screws depends on the type of screws, the fracture morphology and the bone quality.
Using locking screws, two bicortical screws on each side may be sufficient, otherwise, it is recommended to use 6 fixation points on each side. For both major fragments, place one locking screw close to the fracture, and the second at the end of the plate.
Confirm the reduction, plate position, and screw length under image intensification.
Confirm rotational alignment by physical examination.
7. Final radiological assessment
Check for proper reduction and implant position with image intensification in AP and lateral views.
Also confirm correct torsional alignment of the humerus.
8. Aftercare
Principles
The aim of any surgical fixation of humeral shaft fractures is a stable osteosynthesis of the fracture allowing early passive and active motion. This is crucial to prevent elbow stiffness.
The rehabilitation regimen should take account of any damage to soft tissues, either as a result of the injury or due to the surgery. It also needs to take account of the security of the fixation.
Immediate postoperative care
Carefully examine the patient for neurological deficits and pulses.
Early treatment
In the beginning lymph drainage and elastocompressive bandages may be helpful.
Consider a sling for pain relief within the first days.
Treatment for refixation of deltoid detachment
If the deltoid was detached and reattached, active deltoid contraction should be delayed for the first six weeks.
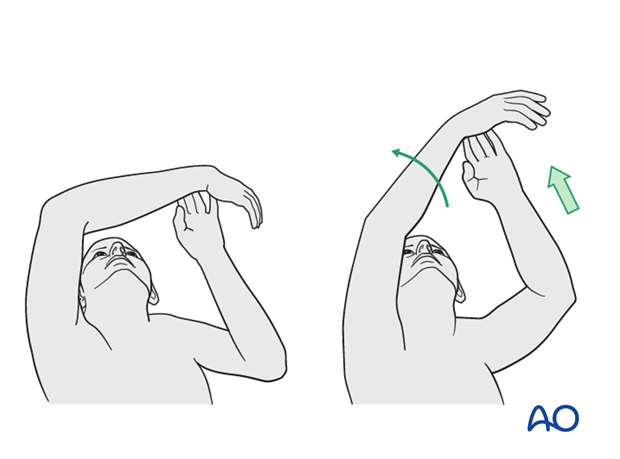
Mobilization
In the early phase the rehabilitation consists of classic maneuvers eg overhead motion exercises.
Rehabilitation should address the entire upper limb.
Exercise against resistance
Depending on the bone quality and compliance of the patient, exercise against resistance might be limited.
Follow-up
Clinical and radiological follow-up should be scheduled at least 6 weeks, 12 weeks and 6 months after surgery and continued until a bony healing is confirmed.
Hardware removal
Typically, humeral plates are left in situ indefinitely.
If removal is considered, bony healing should be confirmed. Plates are not normally removed for at least one year after surgery.
Be aware of the risk to the various nerves when dissecting the soft tissues to gain access to the distal humerus for removing anterior or anterolateral plates.
As the radial nerve runs over a posterior plate, removing this plate should only be considered with great caution, and the patient must be well informed about the risks. The original operation note should describe the relation of the nerve to the plate and should be reviewed before plate removal.













