Plate fixation of pilon compression fracture
1. General considerations
Introduction
Articular fractures need anatomical reduction and fixation. They may be simple or comminuted and may be fixed with an anatomical plate.
These fractures are very unstable.
Typically, they occur in two configurations:
- As centrally impacted, comminuted fractures, or
- With a T- or Y-type fracture geometry.
The articular fragments are reduced and fixed first. In a second step, the extraarticular fracture component is reduced and fixed.
The plate may be applied laterally or dorsally. The lateral application is preferred as it avoids disturbance of the extensor mechanism insertion.
It is desirable to obtain stable fixation to allow early motion and to minimize the risk of degenerative joint disease.
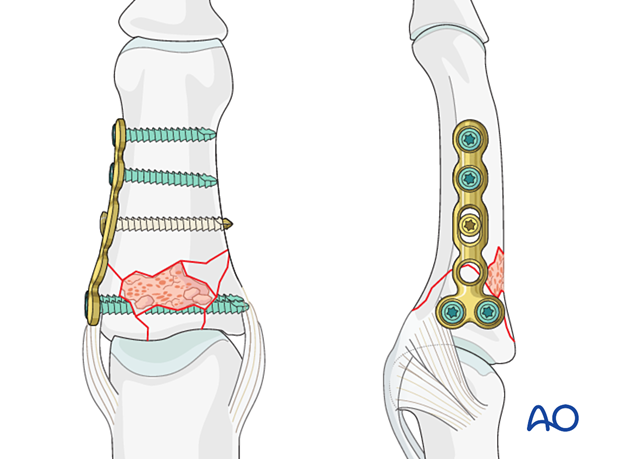
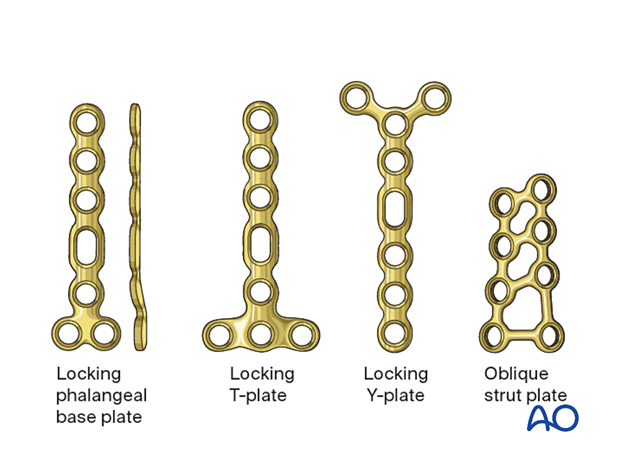
Plate selection
Several plate types are available for treatment of this fracture:
- T- or Y-plate, dorsal
- Strut plate; dorsal
- Phalangeal base plate, lateral
Select a plate according to fragment size, fracture geometry, and surgeon’s preference.
In this procedure the reduction and fixation of a comminuted articular fracture with a phalangeal base plate is shown.
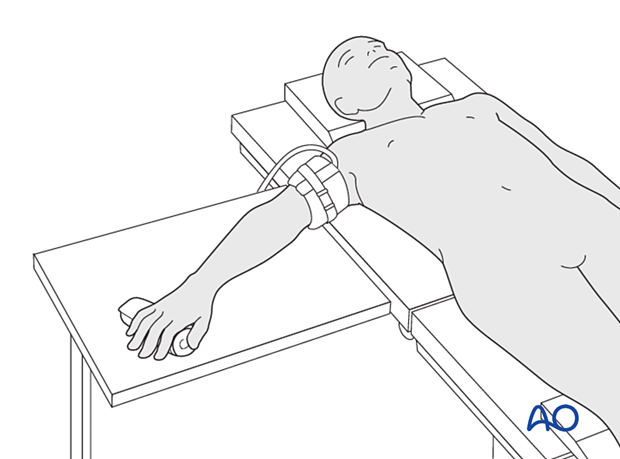
2. Patient preparation
Place the patient supine with the arm on a radiolucent hand table.
3. Approaches
For this procedure the following approaches may be used:
4. Reduction and fixation of the articular block in a simple T- and Y-shaped fracture
Reduction of T- and Y-fractures
If the fracture line allows, eg, in a T- or Y-shaped fracture with the articular fracture line running from radial to ulnar, a lag screw may be inserted to stabilize the articular fracture. This converts a three-part fracture to a two-part fracture.
Make sure the screw track is not interfering with later plate application.
5. Reduction of a compression fracture
Compression fractures are not reducible by ligamentotaxis, as the centrally impacted fragments are devoid of soft-tissue attachments.
Direct reduction is, therefore, necessary.
The key to fixing compression fractures is restoring the joint surface to as close as normal as possible and supporting the reduction with bone graft and internal fixation.
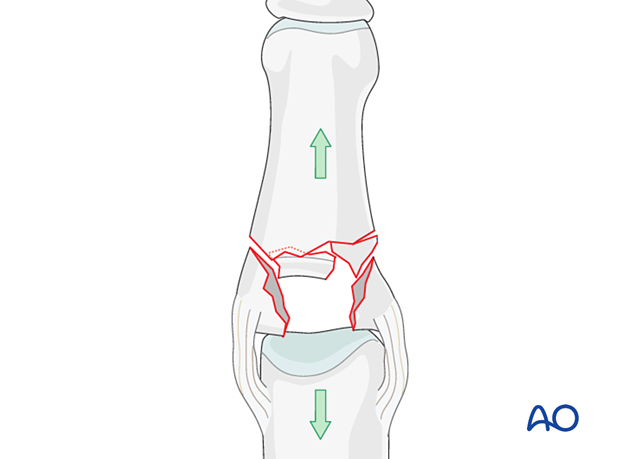
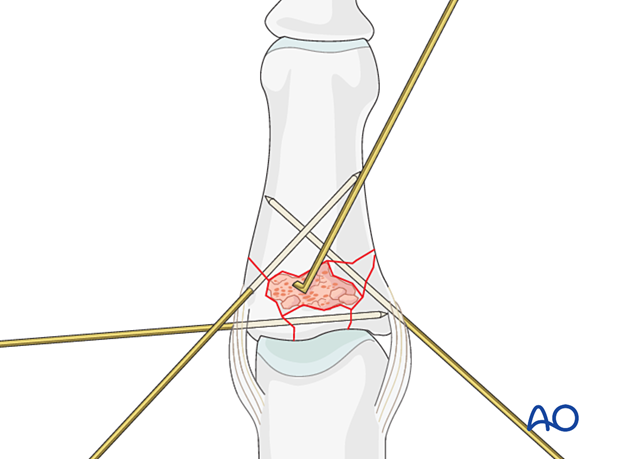
Use a K-wire, a dental pick, or a small curette to push the depressed fragments towards the head of the proximal phalanx, which should be used as a template to ensure congruity of the articular surface of the middle phalanx to reduce the risk of later degenerative joint disease.
If a cartilage step-off remains, degenerative joint disease is likely to follow.
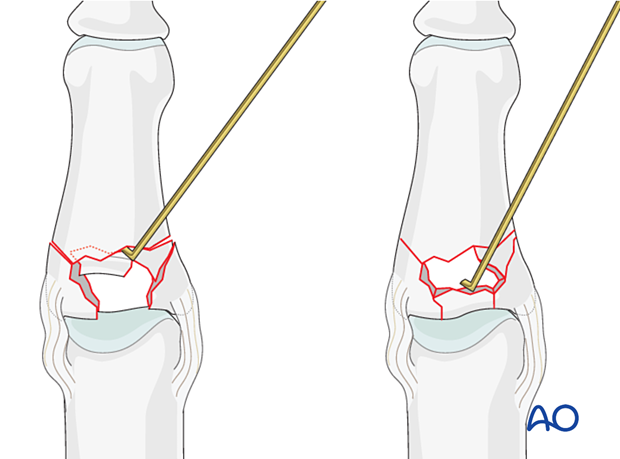
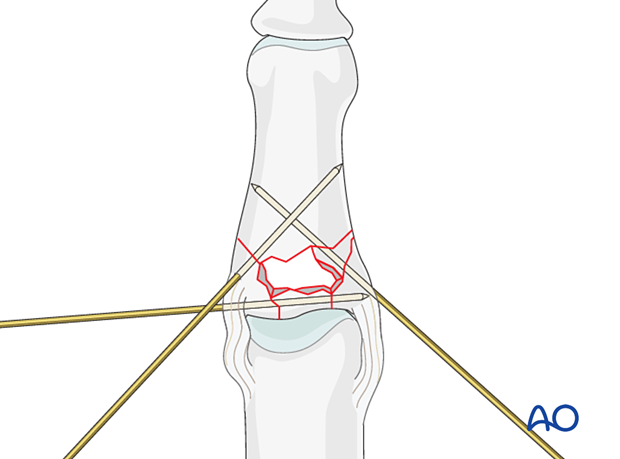
Preliminary K-wire fixation
Small K-wires may be used for preliminary fixation and support of the subchondral fragments.
6. Checking alignment
Identifying malrotation
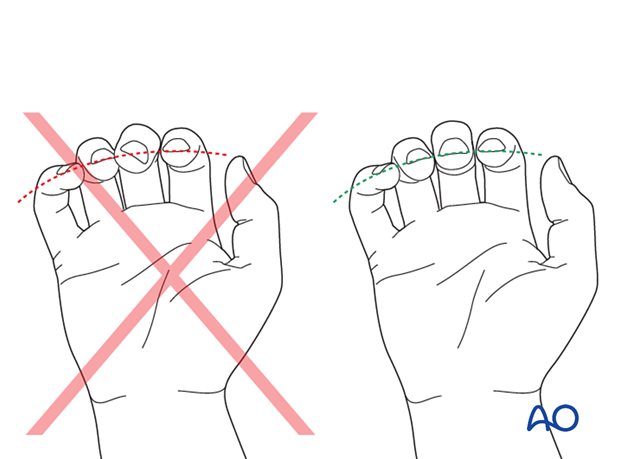
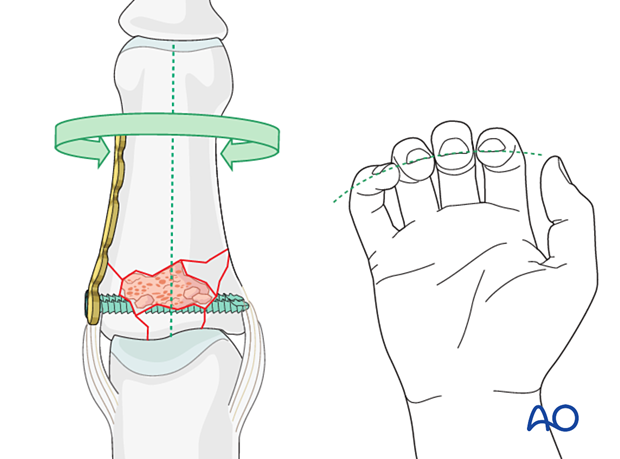
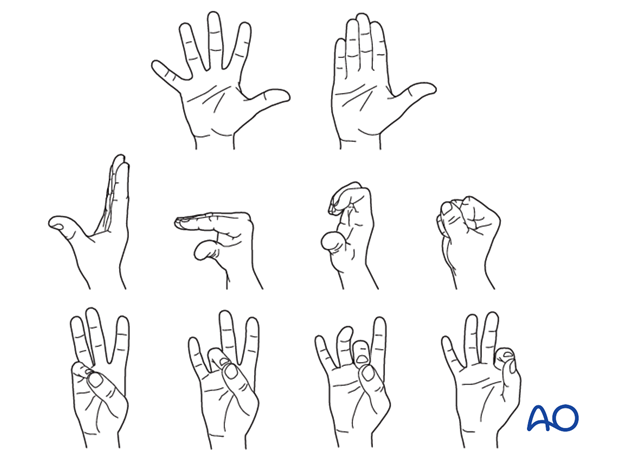
At this stage, it is advisable to check the alignment and rotational correction by moving the finger through a range of motion.
Rotational alignment can only be judged with the fingers in a degree of flexion, and never in full extension. Malrotation may manifest itself by overlap of the flexed finger over its neighbor. Subtle rotational malalignments can often be judged by tilting of the leading edge of the fingernail when the fingers are viewed end-on.
If the patient is conscious and the regional anesthesia still allows active movement, the patient can be asked to extend and flex the finger.
Any malrotation is corrected by direct manipulation and later fixed.
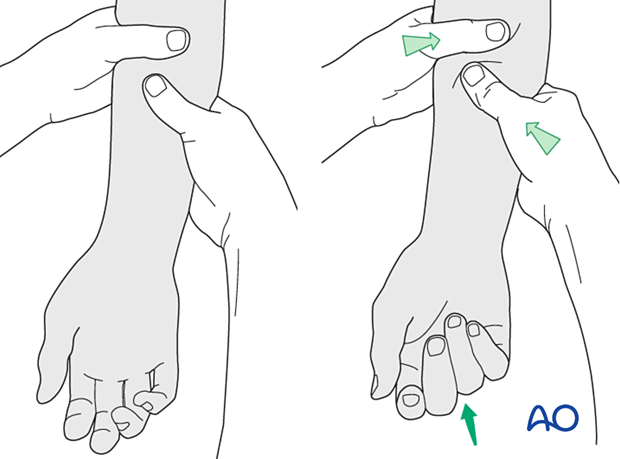
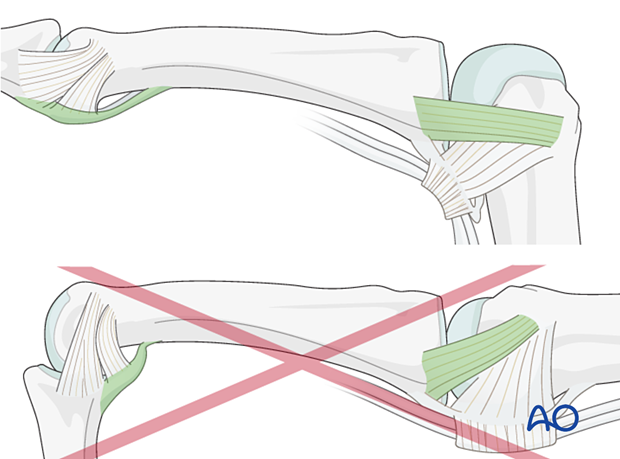
Using the tenodesis effect when under anesthesia
Under general anesthesia, the tenodesis effect is used, with the surgeon fully flexing the wrist to produce extension of the fingers and fully extending the wrist to cause flexion of the fingers.
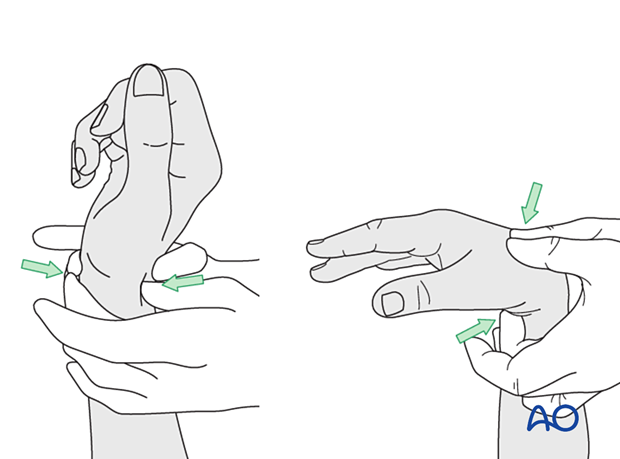
Alternatively, the surgeon can exert pressure against the muscle bellies of the proximal forearm to cause passive flexion of the fingers.
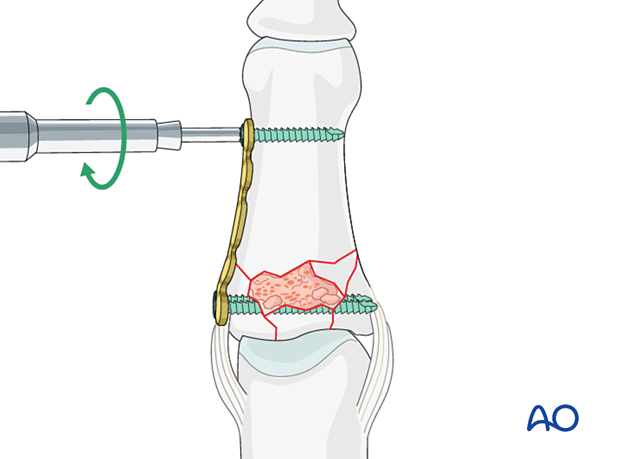
7. Adding bone graft
Since the subchondral cancellous bone is impacted, a void may remain following reduction of the articular fragments.
This jeopardizes fracture healing:
- Very unstable situation in which the fragments may easily redisplace (collapse)
- Delayed healing process
Therefore, bone grafting is recommended to provide support to the subchondral bone and increase the potential for bone regeneration and healing.
Use a pusher instrument to fill the whole fracture cavity and impact the bone graft.
Confirm reduction with an image intensifier.
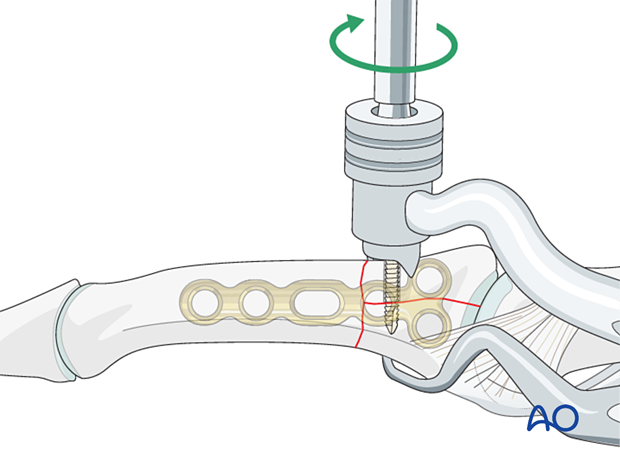
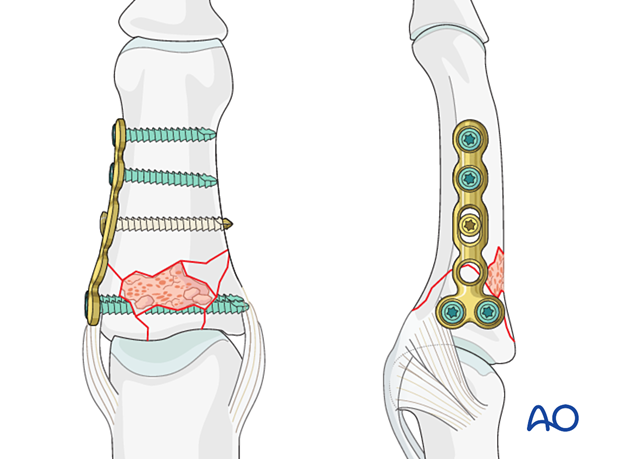
8. Plate fixation
Plate trimming
Adapt the plate length to fit the length of the middle phalanx. Avoid sharp edges, which may be injurious to the tendons. At least two screws need to be inserted on either side of the fracture zone.
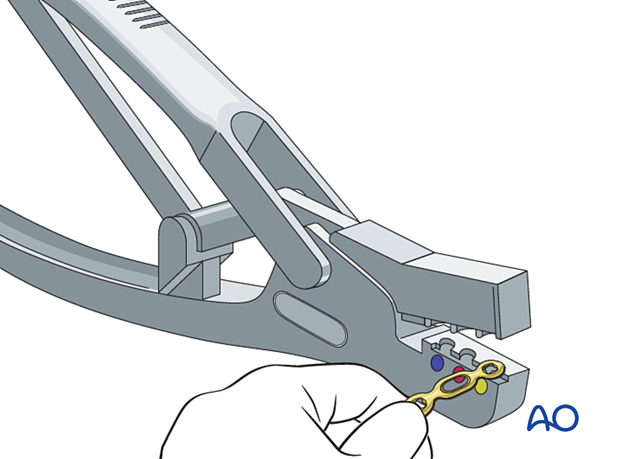
Plate positioning
Place the plate slightly dorsal to the midaxial line of the bone, allowing at least two screws in both end fragments.
Keep the plate in place with the atraumatic forceps.
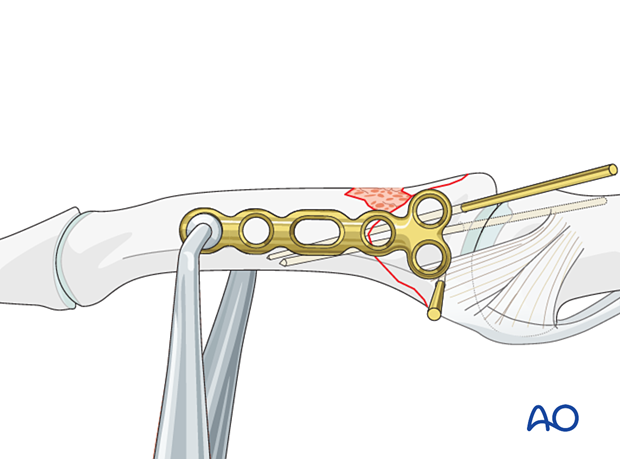
Screw insertion
Start with insertion of a locking head screw in the articular block.
Check the plate position and rotational alignment with an image intensifier and adjust it if necessary.
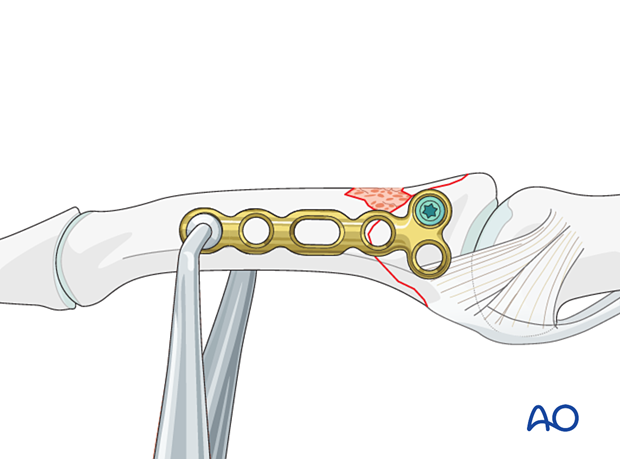
Correcting length and malrotation
Manipulate the distal part of the phalanx to correct length and malrotation.
Add a screw in the diaphysis.
Recheck the plate position and rotational alignment with an image intensifier and adjust it if necessary.
Complete the screw fixation according to the fracture configuration.
Cover the plate with periosteum to avoid adhesion between the tendon and the implant leading to limited finger movement.
9. Final assessment
Confirm fracture reduction and stability and implant position with an image intensifier.
10. Aftercare
Postoperative phases
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.
Postoperative treatment
If there is swelling, the hand is supported with a dorsal splint for a week. This should allow for movement of the unaffected fingers and help with pain and edema control. The arm should be actively elevated to help reduce the swelling.
The hand should be immobilized in an intrinsic plus (Edinburgh) position:
- Neutral wrist position or up to 15° extension
- MCP joint in 90° flexion
- PIP joint in extension
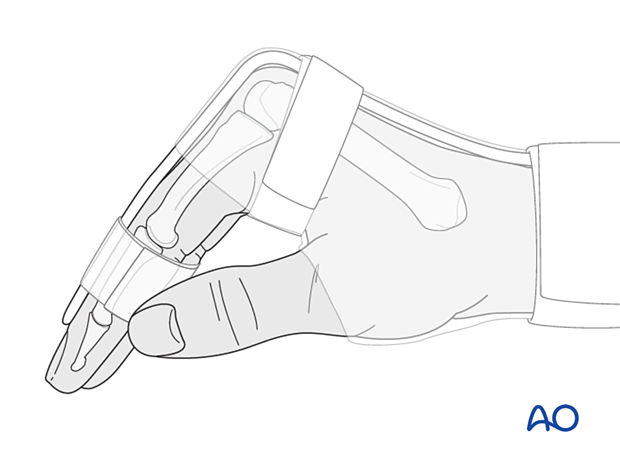
The MCP joint is splinted in flexion to maintain its collateral ligaments at maximal length to avoid contractures.
The PIP joint is splinted in extension to maintain the length of the volar plate.
After swelling has subsided, the finger is protected with buddy strapping to neutralize lateral forces on the finger until full fracture consolidation.
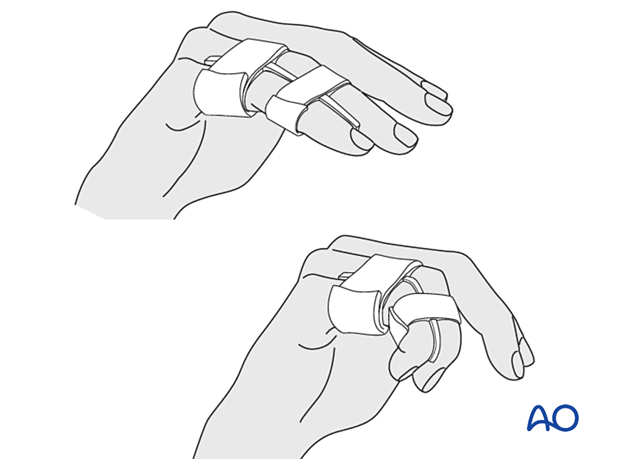
Mobilization
To prevent joint stiffness, the patient should be instructed to begin active motion (flexion and extension) of all nonimmobilized joints immediately after surgery.
Follow-up
The patient is reviewed frequently to ensure progression of hand mobilization.
In the middle phalanx, the fracture line can be visible in the x-ray for up to 6 months. Clinical evaluation (level of pain) is the most important indicator of fracture healing and consolidation.
Implant removal
The implants may need to be removed in cases of soft-tissue irritation.
In case of joint stiffness or tendon adhesion restricting finger movement, arthrolysis or tenolysis may become necessary. In these circumstances, the implants can be removed at the same time.













