Dorsal approach to the middle phalanx
1. Introduction
The dorsal approach offers access to the extensor tendon, and the metaphysis and diaphysis of the middle phalanx.
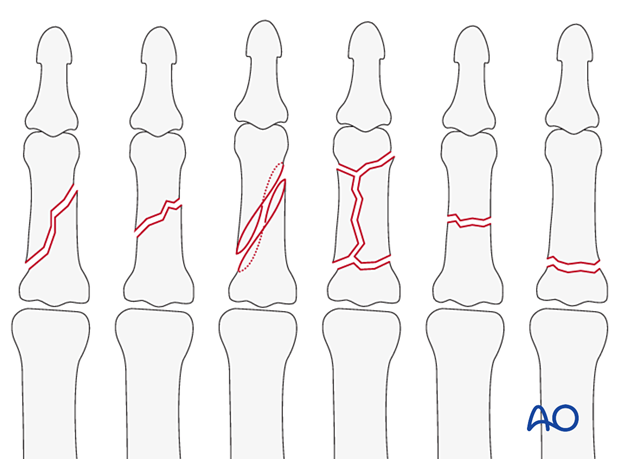
This approach is indicated for oblique, spiral, comminuted, or transverse fractures of the diaphysis, or metaphysis of the middle phalanx.
It can also be used for corrective osteotomies of malunited fractures.
AO teaching video
Finger, middle phalanx, dorsal approach
2. Surgical anatomy
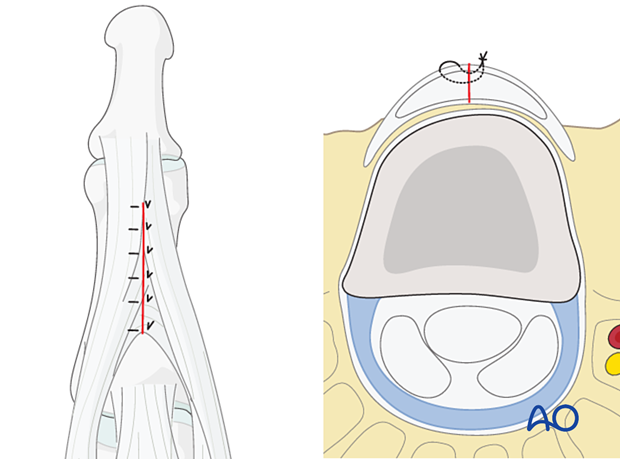
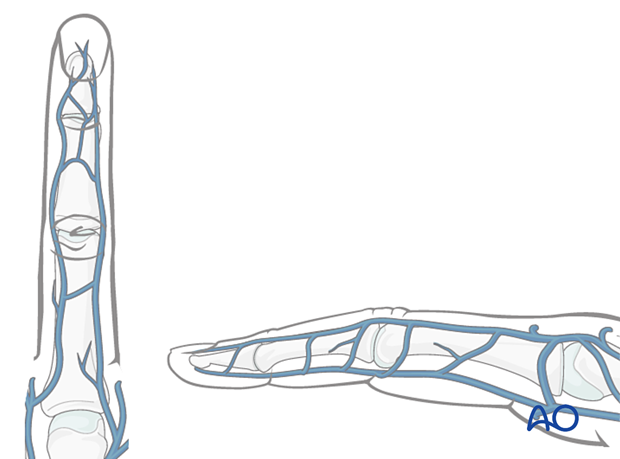
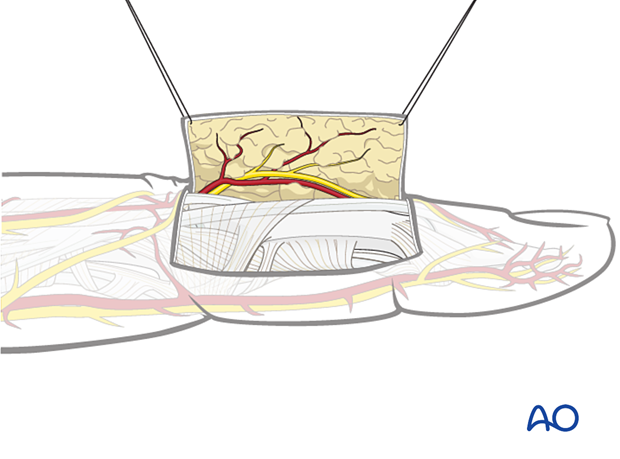
Nerve identification
Identify and protect the dorsal sensory branches of the radial and ulnar nerves in the thin subcutaneous tissue.
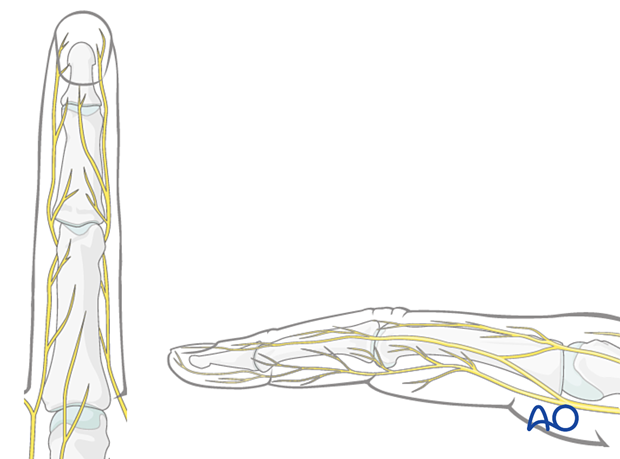
Vein identification
The dorsal venous system of the fingers has longitudinal and transverse branches. Be careful to preserve the longitudinal branches. For better exposure, the transverse branches may be ligated or cauterized but preserve as many dorsal veins as possible to avoid congestion and swelling, with consequent fibrosis and stiffness.
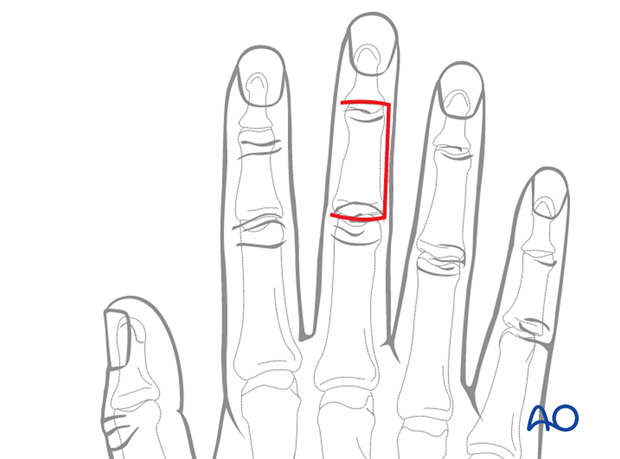
3. Skin incision
Several skin incision options are available. Each comes with benefits and disadvantages.
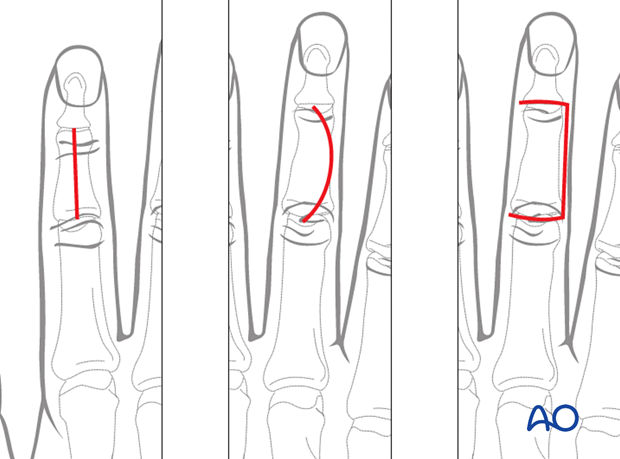
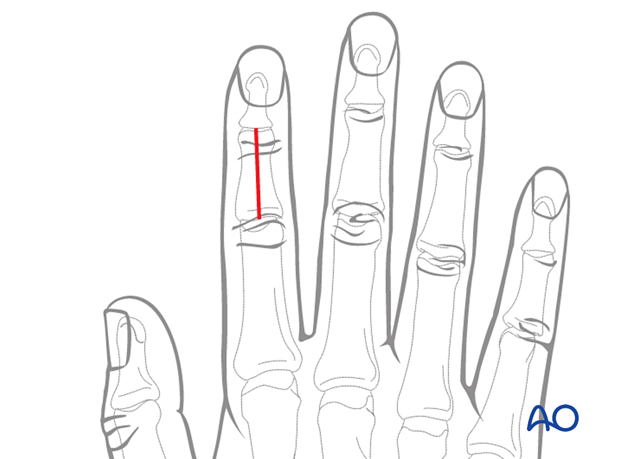
Straight dorsal incision
Perform a straight, midline, dorsal skin incision, starting at the proximal interphalangeal (PIP) joint and ending at the distal interphalangeal (DIP) joint. Depending on the fracture geometry, the incision may be shorter.
Advantages:
- Perfusion and venous drainage are well preserved.
- Early postoperative motion will prevent scarring between skin, tendon, and bone.
Disadvantage:
- Skin and tendon scarring will be in the same line and tethering may occur.
- Limited approach to lateral structures.
Curved skin incision
Perform a curved skin incision extending from the PIP joint to the DIP joint.
The convexity of the incision is planned so that the scar does not involve the radial border of the index, or the ulnar border of the little finger. The fracture configuration and implant placement must be considered when planning the incision.
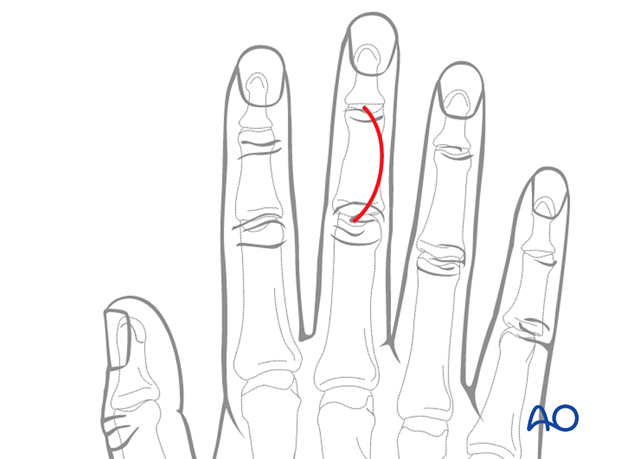
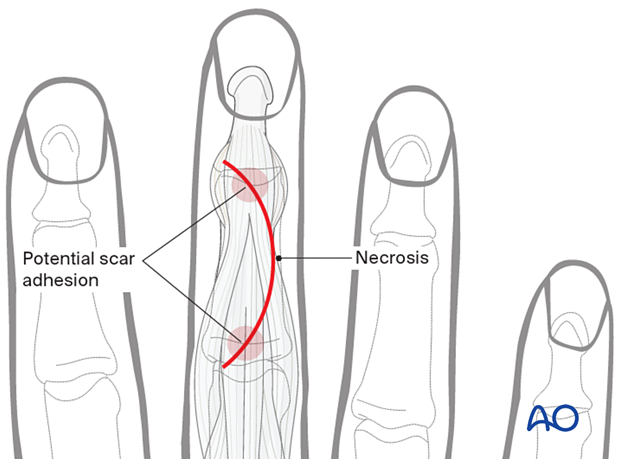
Advantage:
- Skin and tendon scarring are not in the same line and tethering due to scarring may be avoided.
Disadvantage:
- Relatively poor perfusion at the apex of the curve may risk skin necrosis and delayed healing.
Dorsal fasciocutaneous flap
Start a transverse incision at the level of the DIP joint crease. Continue the incision midaxially parallel to the bone axis avoiding damage to the neurovascular bundle. Curve it gently over the PIP joint crease.
This skin incision allows for an extensile paratendon or tendon split approach.
Depending on the fracture pattern, the flap may be created on the ulnar or radial side.
The skin on the ulnar side of the 5th finger and the radial side of the 2nd finger should be preserved to protect sensitivity.
It has the advantage of low risk of scar adhesion, apical flap necrosis, and a better esthetic result of skin scars.
Elevate the fasciocutaneous flap by sharp dissection in the subfascial plane outside the epitenon. Retract it using fine sutures.
Identify and preserve nerves and longitudinal veins.
4. Deep dissection
Keep in mind, when developing the flaps, that the layers must be elevated together to avoid devascularization.
There are two alternative deep approaches:
- Midline extensor tendon splitting
- Paratendon
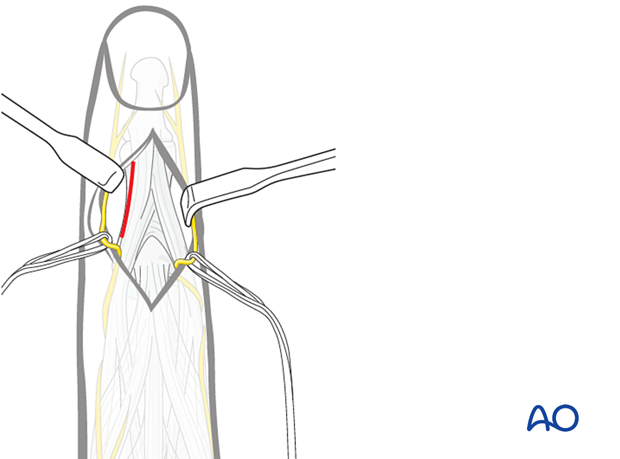
Midline extensor tendon splitting
Expose the terminal extensor tendon with its triangular ligament.
Make a longitudinal incision through both the terminal extensor tendon and its triangular ligament, taking care to preserve the periosteum.
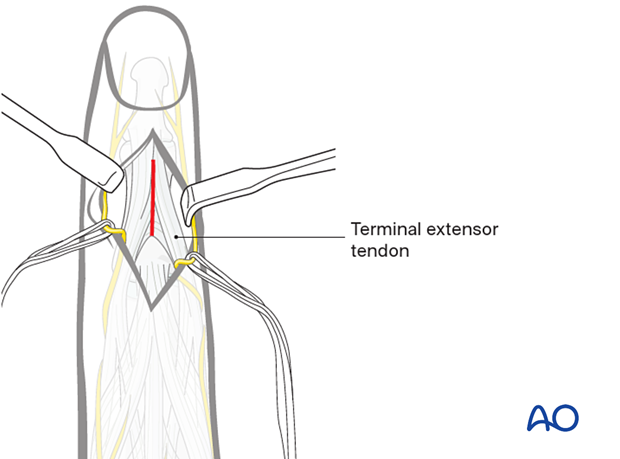
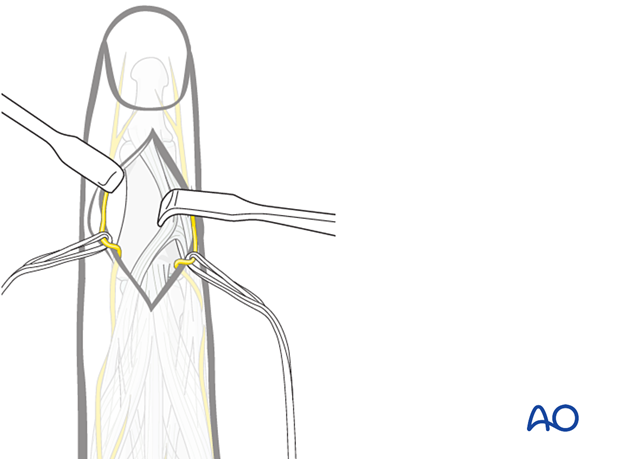
After incising the terminal extensor tendon and its triangular ligament, two small retractors are used to expose the bone.
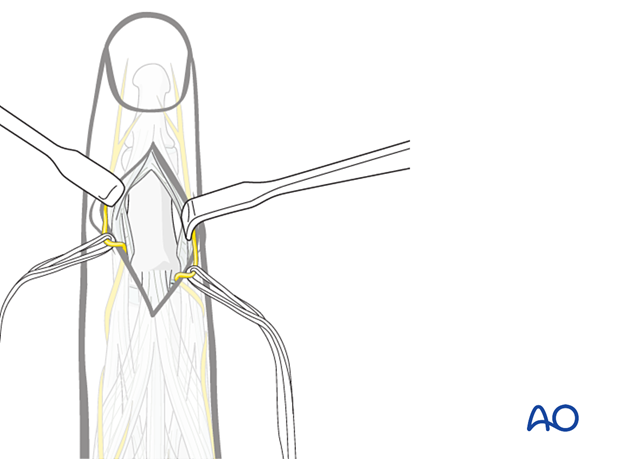
Paratendon approach
Perform an incision between the lateral band and the central slip of the extensor tendon. The incision may be on the radial or ulnar side according to the fracture pattern.
Retract the extensor tendon towards the midline, according to the fracture pattern and requirements of fixation
5. Wound closure
Regardless of the chosen approach, all tendon incisions must be repaired with nonabsorbable monofilament sutures with an atraumatic needle prior to wound closure.
Repair the terminal extensor tendon and its triangular ligament with fine interrupted mattress sutures.
The following suture dimension should be used:
- 4.0 for central tendon repair
- 6.0 for associated ligament and periosteum repair
Cover any metallic implants with the periosteum as far as possible; this helps minimize contact between the extensor tendons and the implant.