Midaxial approach to the middle phalanx
1. Introduction
The midaxial, also known as lateral, approach gives access to the midaxial ligaments, the proximal phalanx, and the proximal and distal end segments.
For management of articular fractures of the head, the incision may need to be enlarged distally.
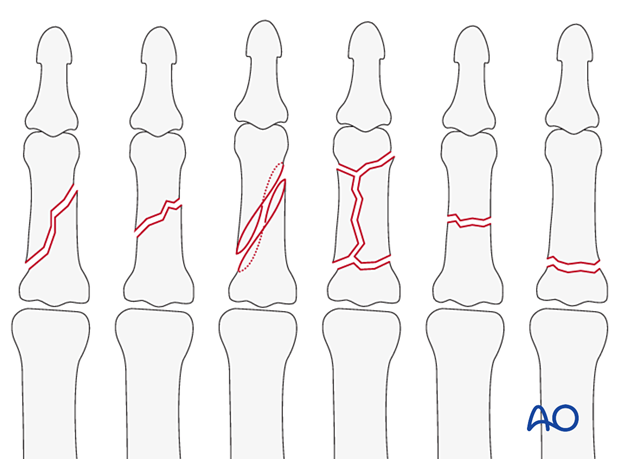
This approach is indicated for oblique, spiral, comminuted, or transverse fractures of the diaphysis and metaphysis of the middle phalanx.
AO teaching video
Finger, middle phalanx, lateral approach
2. Surgical anatomy
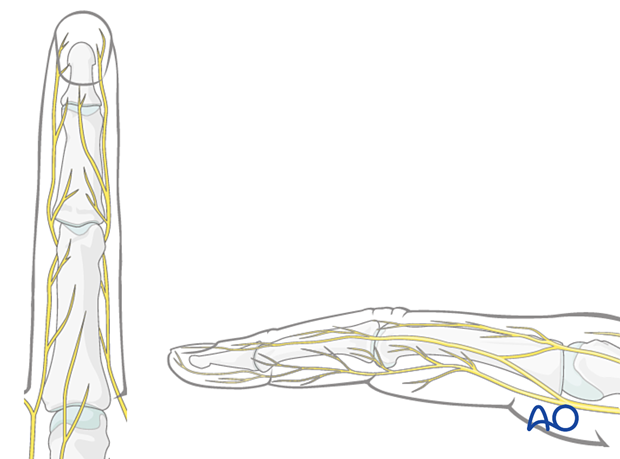
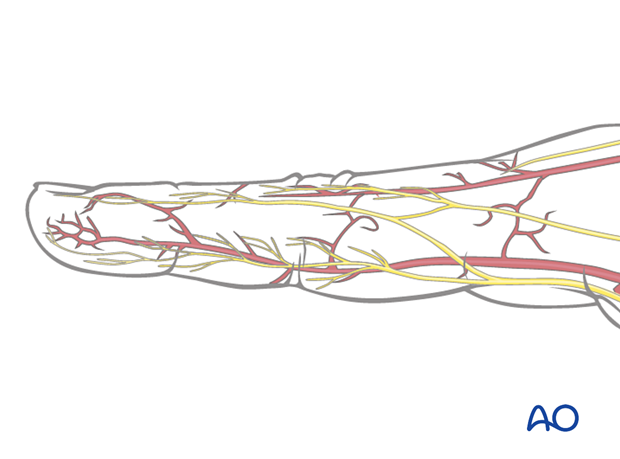
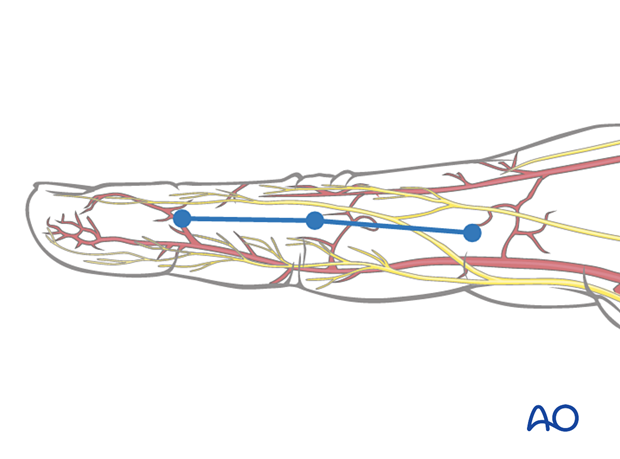
Nerve identification
Identify and protect the dorsal sensory branches of the radial and ulnar nerves in the thin subcutaneous tissue.
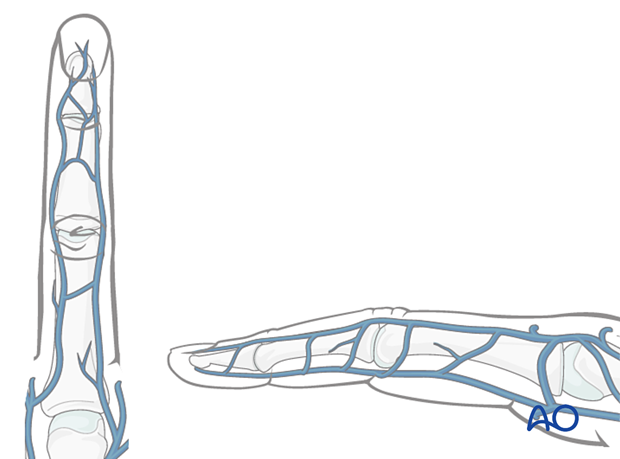
Vein identification
The dorsal venous system of the fingers has longitudinal and transverse branches. Be careful to preserve the longitudinal branches. For better exposure, the transverse branches may be ligated or cauterized but preserve as many dorsal veins as possible to avoid congestion and swelling, with consequent fibrosis and stiffness.
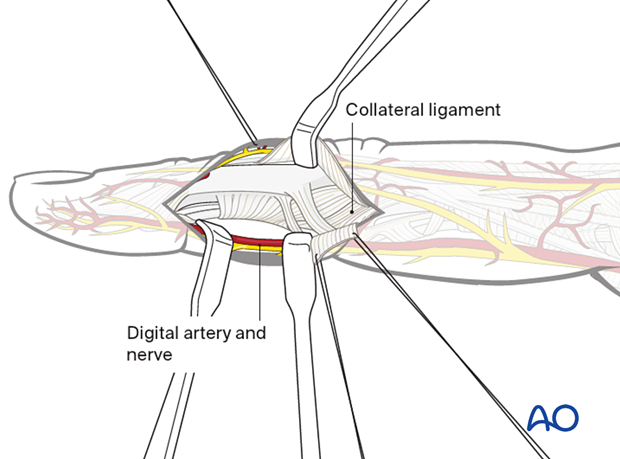
Digital artery and nerve
The digital artery and digital nerve lie palmar to the midaxial line in collateral relation with the flexor tendon sheath.
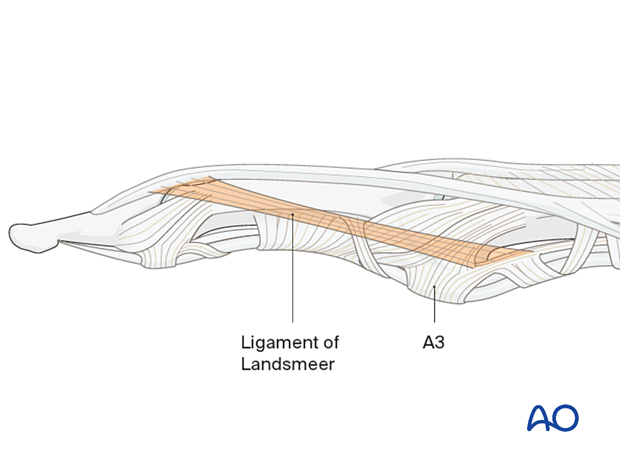
Preservation of soft-tissue structures
The oblique retinacular ligament of Landsmeer passes obliquely from the palmar aspect at the attachment of the A3 pulley to the terminal conjoint extensor tendon. This ligament must be preserved to avoid a mallet deformity.
If it proves necessary to divide this ligament, it must be repaired carefully.
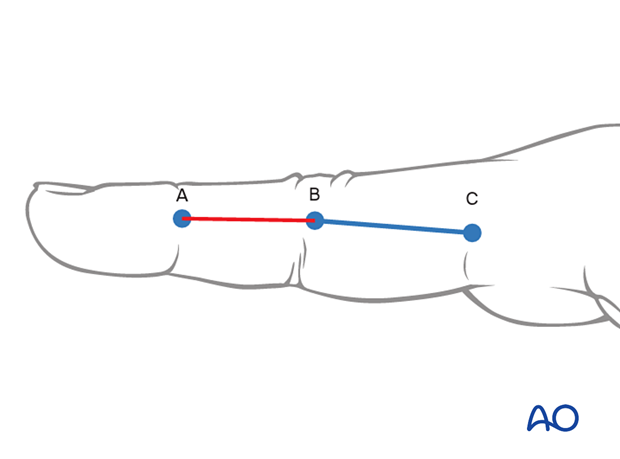
3. Skin incision
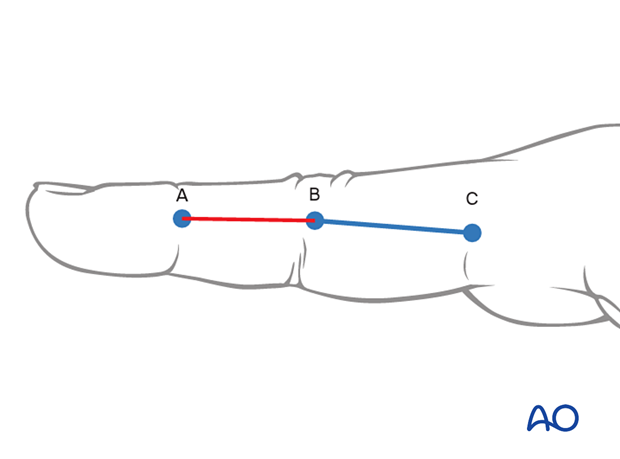
To plan the line of the incision, fully flex the finger as shown and mark the dorsal ends of the flexor creases with dots.
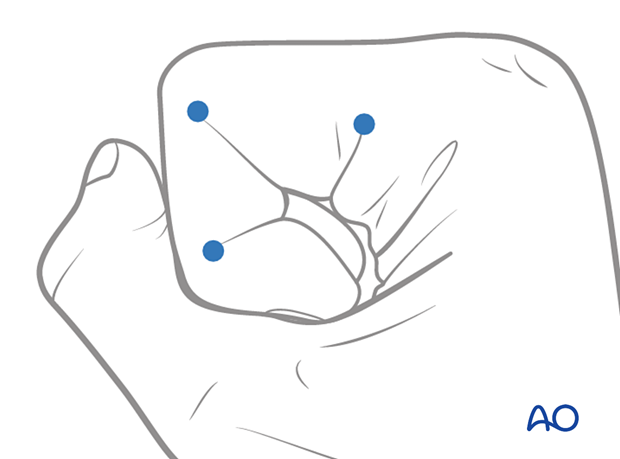
Extend the finger and connect the dots in a line.
The resulting line is safe for a midaxial skin incision. The digital artery and digital nerve will lie palmar to this line.
Make a skin incision from A to B. For further exposure, the incision can be extended proximally.
4. Deep dissection
Blunt dissection
Elevate the thin subcutaneous tissues by blunt dissection. Identify and protect the digital vessels and nerve on the palmar aspect, and gently retract them.
The transverse retinacular ligament (TRL) is now exposed.
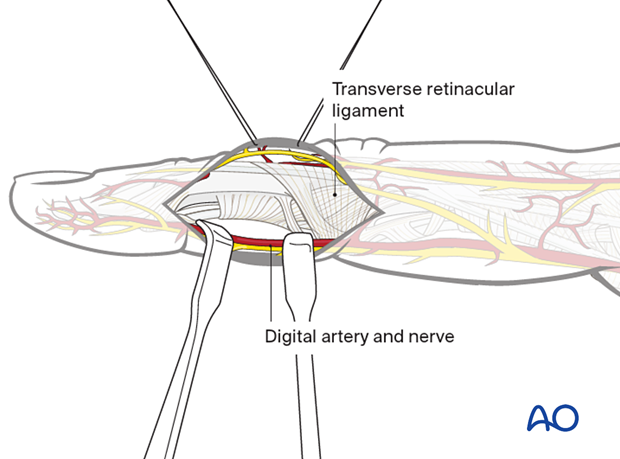
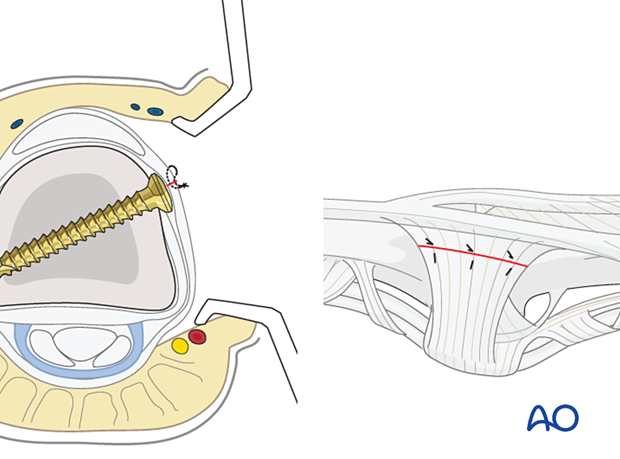
Division of the transverse retinacular ligament
Divide the TRL, using a dental pick inserted between it and the collateral ligament, to avoid accidentally cutting the collateral ligament.
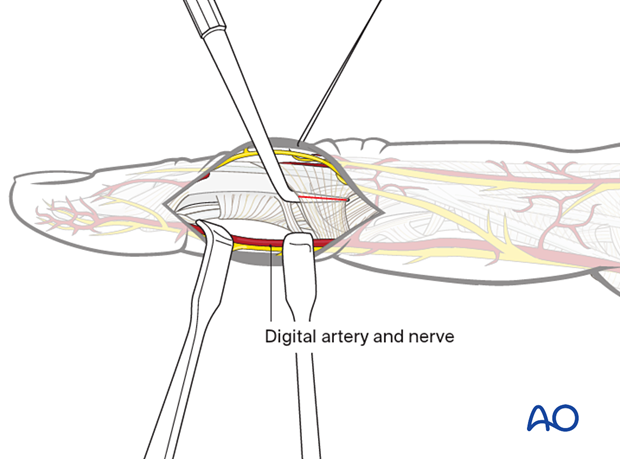
Exposure of the fracture
Elevate the dorsal fringe of the TRL dorsally with the lateral band to expose the collateral ligament. Retract the palmar remainder of the TRL in a palmar direction, using two fine sutures.
This exposes the fracture extraperiosteally. Elevate the periosteum only immediately adjacent to the fracture line(s).
5. Wound closure
Regardless of the chosen approach, all tendon incisions must be repaired with nonabsorbable monofilament sutures with an atraumatic needle prior to wound closure.
Repair the TRL with multiple fine mattress sutures prior to skin closure.
The following suture dimension should be used:
- 4.0 for central tendon repair
- 6.0 for associated ligament and periosteum repair
Cover any metallic implants with the periosteum as far as possible; this helps minimize contact between the extensor tendons and the implant.