Joint reconstruction of palmar impaction fracture
1. General considerations
Palmar impaction fractures need reduction of subchondral fragments. Bone graft and a subchondral screw should be added to support the articular surface.
Reduction, addition of bone graft, and insertion of a subchondral screw through a dorsal approach is shown in this procedure.
The recovery process after such injuries is slow. Advise the patient to expect 6–8 months for full recovery.
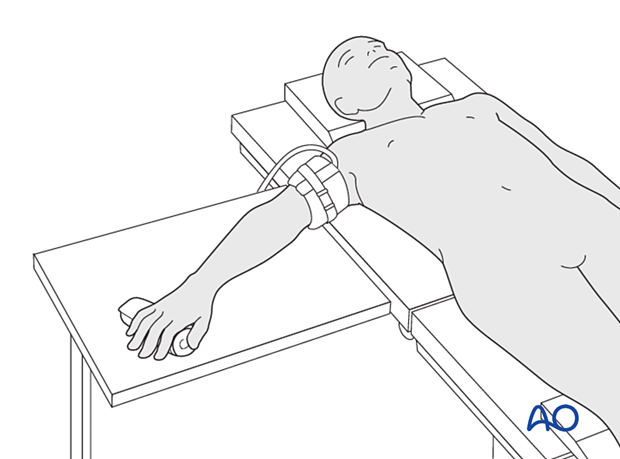
2. Patient preparation
Place the patient supine with the arm on a radiolucent hand table.
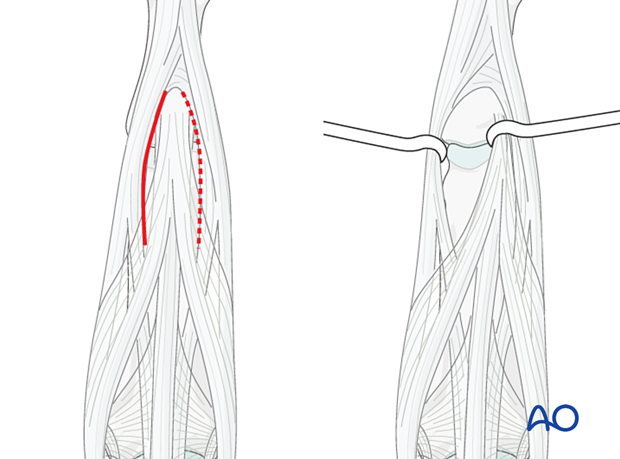
3. Approach
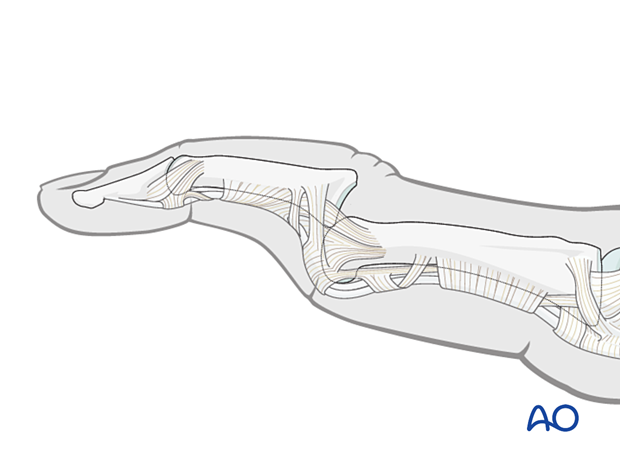
Often, a palmar approach, with shotgun extension, is used for these fractures.
However, since that approach requires considerable additional dissection and trauma to the soft tissues, with consequent inflammatory reaction and fibrosis, a dorsal approach may be more biological. An incision between the lateral band and the central slip is recommended.
Take special care to protect the insertion of the central slip, otherwise, a boutonnière deformity can develop.
4. Reduction of dislocation
Closed reduction
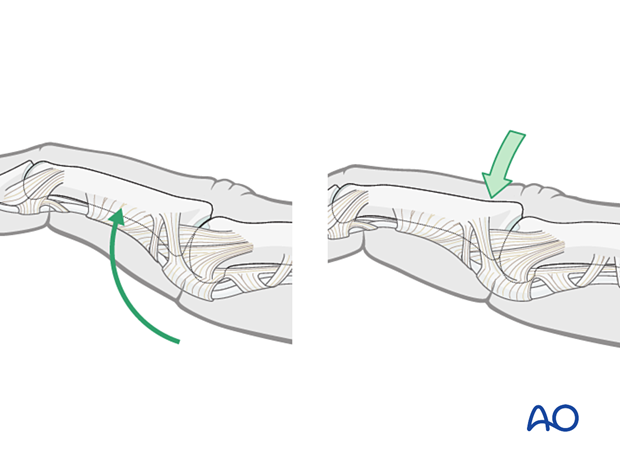
Dislocation usually presents as an extension displacement with dorsal deformity.
This can be reduced by increasing the deformity with gentle dorsally applied pressure on the middle phalanx to reduce the joint. This keeps the palmar structures in tension and reduced the risk of soft-tissue interposition.
5. Fracture reduction
The reduction of the articular fragments can be achieved in different ways depending on the fracture pattern:
- Closed by distraction
- Directly through the fracture
- Directly through a remote entry window (shown here)
Evaluation of the fracture
Evaluate the fracture.
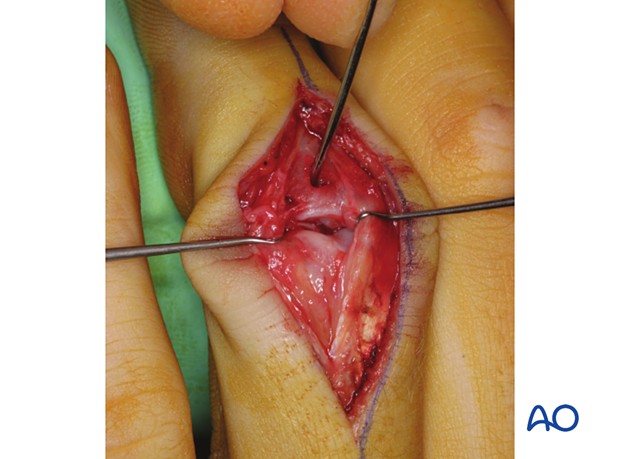
Often, the degree of comminution is not apparent from the x-rays and can only be determined under direct vision.
The image shows a fracture with a large area of the palmar articular surface comminuted and impacted. The only remaining articular cartilage is on the dorsal aspect. Bone grafting and reconstruction is the recommended option.
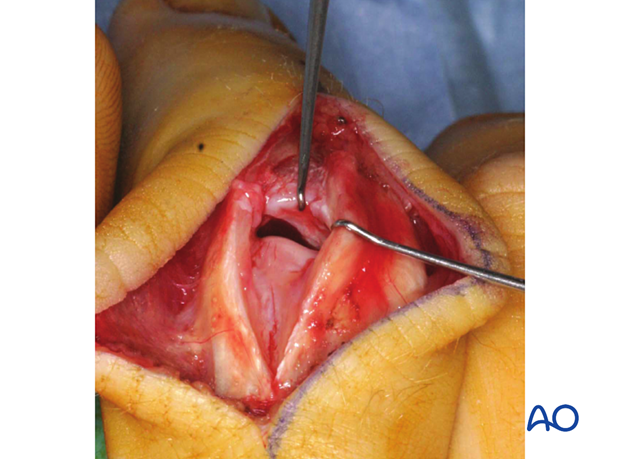
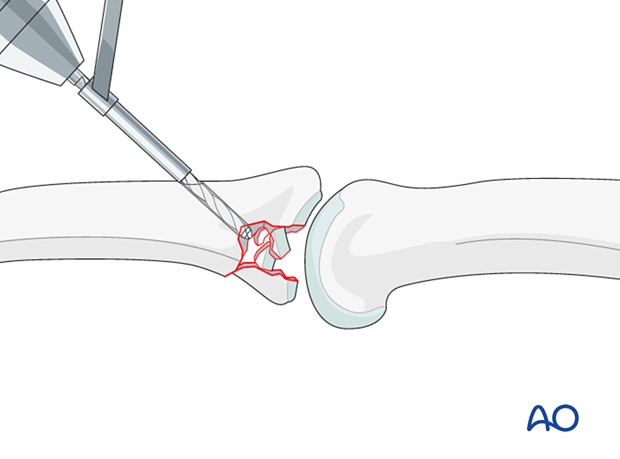
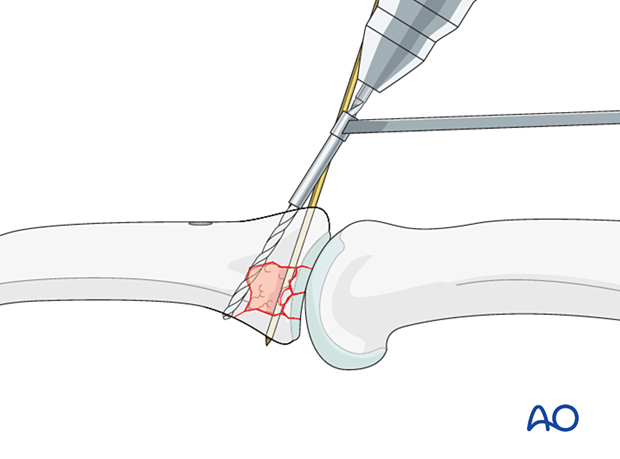
Creation of access window
A window will aid with the reduction of the articular fragments.
This window should be located in the basal metaphysis of the middle phalanx, well away from the joint surface, in the interval between the central slip insertion and the collateral ligament.
Ensure that the window is distal enough not to interfere with later screw placement.
Use a 1.5 mm drill bit to create an oblique window into the cortical bone.
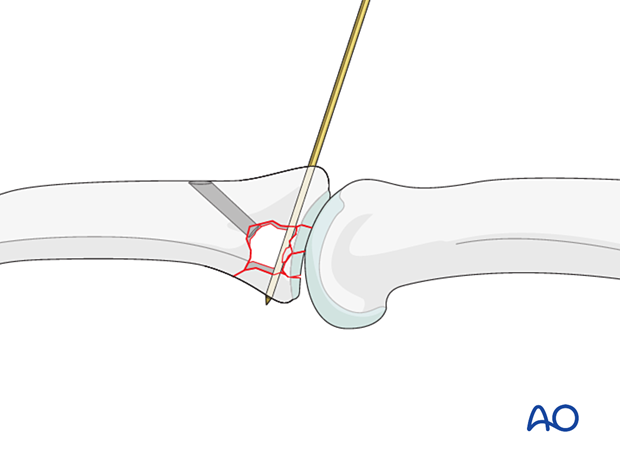
Reduction of the depressed articular fragments
Compression fractures are not reducible by ligamentotaxis, as the centrally impacted fragments are devoid of soft-tissue attachments.
Direct reduction is thus necessary.
The key to fixing compression fractures is restoring the joint surface to as close to normal as possible (anatomically) and supporting the reduction with bone graft.
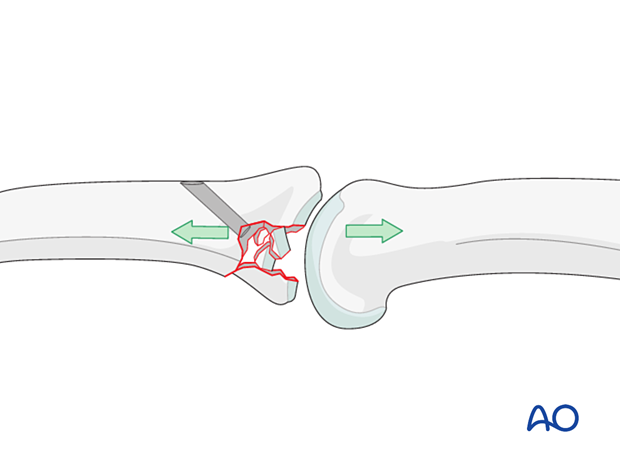
Insert a stout hypodermic needle, a dental pick, or a tiny curette, into the drill hole. Disimpact the fragments and push them towards the head of the proximal phalanx, which is used as a template to ensure congruity of the articular surface of the middle phalanx.
If a cartilage step-off remains, degenerative joint disease is likely to follow.
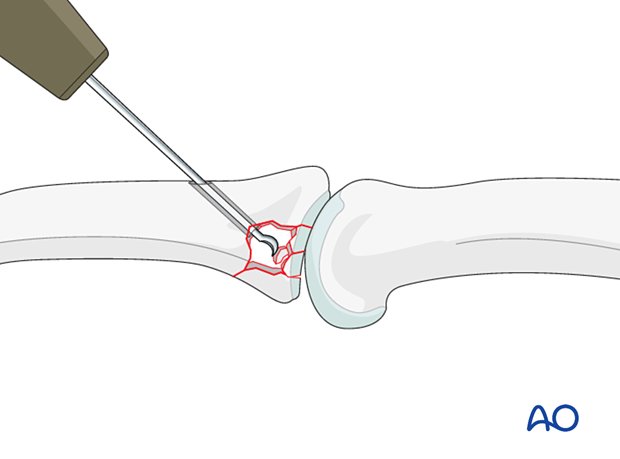
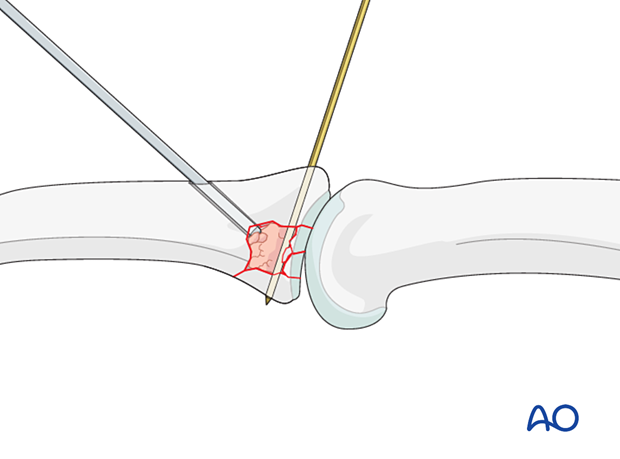
This intraoperative photo shows the reduction with a curette inserted through the cortical window.
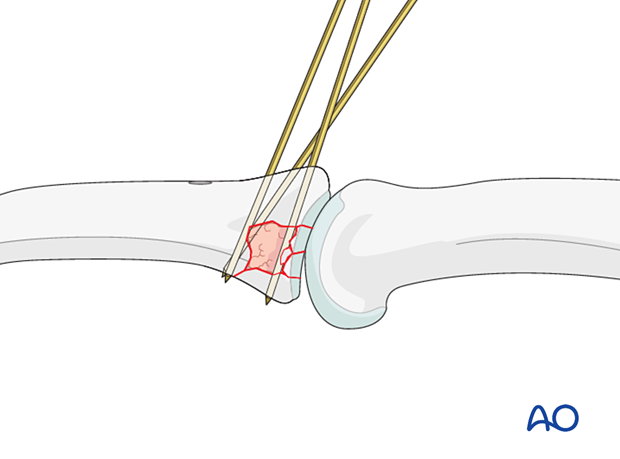
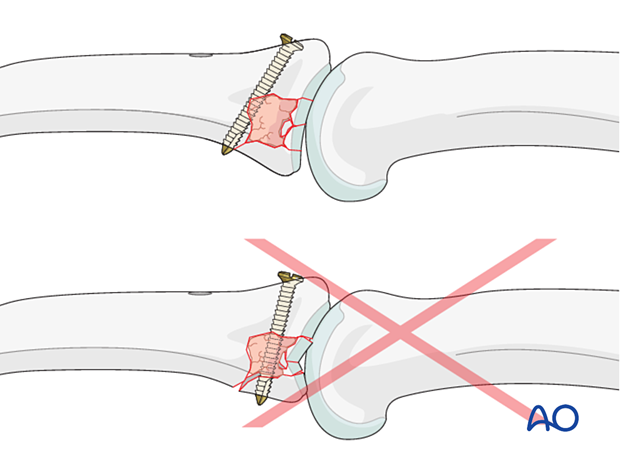
Stabilization of articular fragments
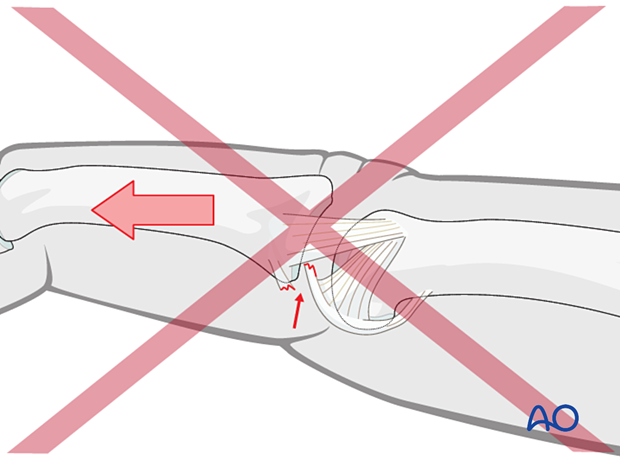
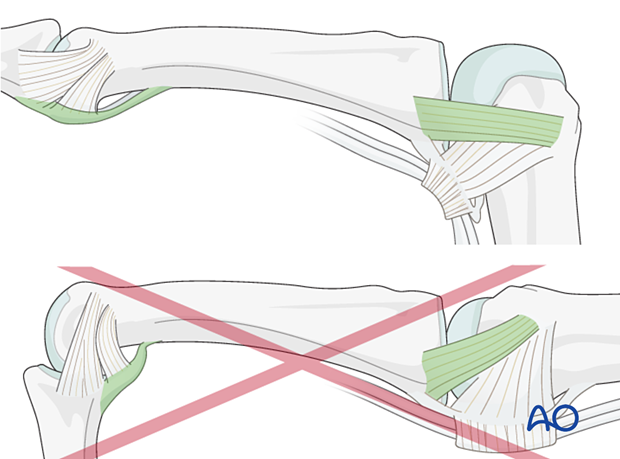
Insert one or more K-wires preferably from dorsal to palmar to stabilize the reduction of the articular fragments. This can be left until fracture consolidation.
Insertion from palmar to dorsal may damage neurovascular bundle and flexor tendons.
6. Adding bone graft
Since the subchondral cancellous bone is impacted, a void may remain following reduction of the articular fragments.
This jeopardizes fracture healing:
- Very unstable situation in which the fragments may easily redisplace (collapse)
- Delayed healing process
Therefore, bone grafting is recommended to provide support to the subchondral bone and increase the potential for bone regeneration and healing.
Use a pusher instrument to fill the whole fracture cavity and impact the bone graft.
Confirm reduction with an image intensifier.
7. Buttressing
Use of K-wires
Buttressing of the bone graft with one or more K-wires may be considered.
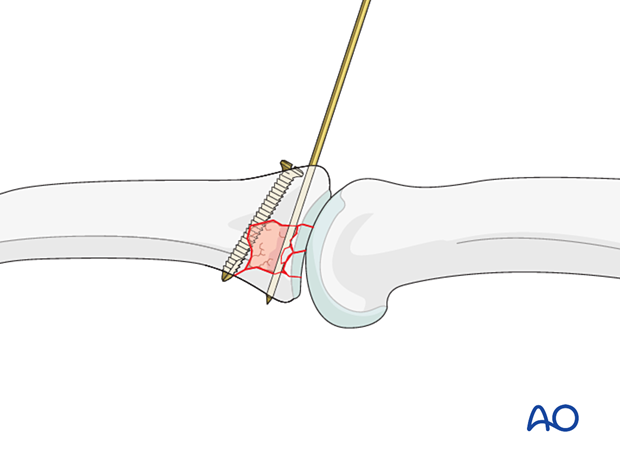
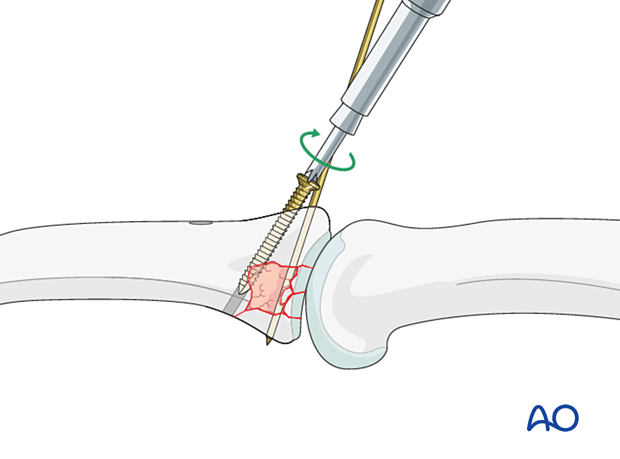
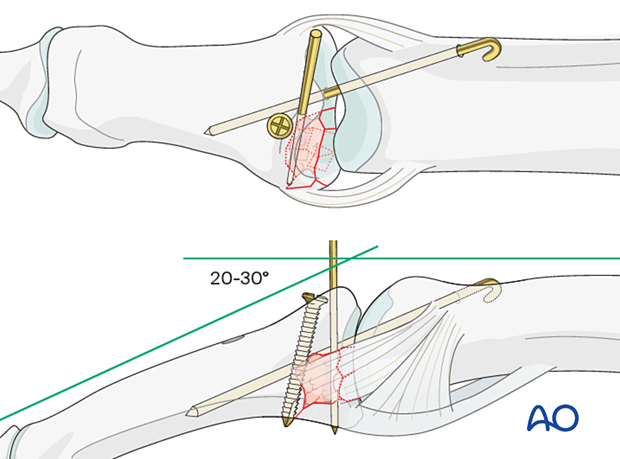
Use of a position screw
In the case of a larger cavity with structured bone graft, a position screw (a bicortical cortex screw without lag compression) may be used for buttressing.
However, it is preferred to use an antiglide plate.
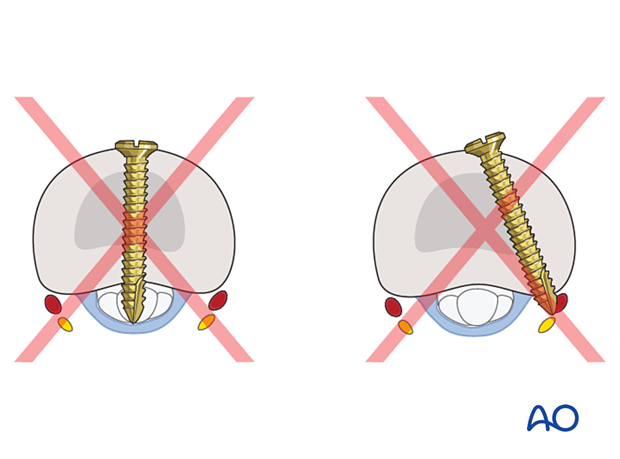
The screw must be inserted into uninjured palmar cortex and must engage both cortices.
The screw does not need to be inserted parallel to the joint surface. It is more important that it serve to stabilize the reconstruction, and that it has good purchase in both cortices.
The screw head must be of no greater diameter than a third of the distance between the articular cartilage and the access window. Usually, a 1.0 mm or a 1.3 mm screw is used.
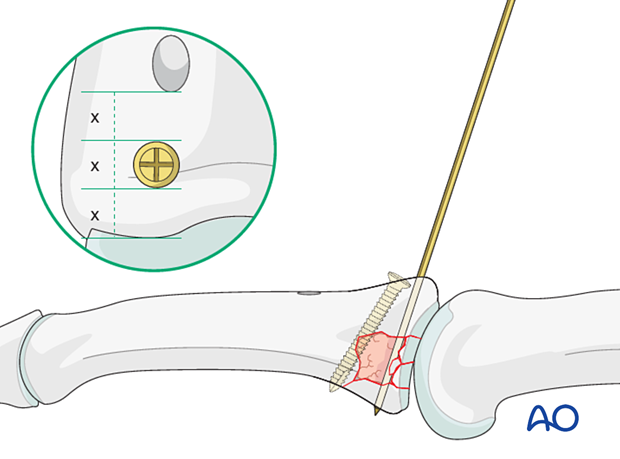
Use a drill guide carefully to drill a hole through both cortices.
Accurately measure screw length with a depth gauge.
No countersinking is necessary.
Gently insert the screw.
If possible, a second screw may be inserted in the same fashion.
8. Protection of articular reconstruction
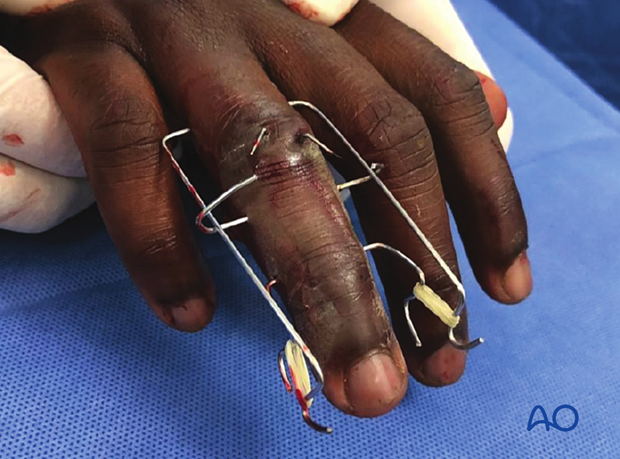
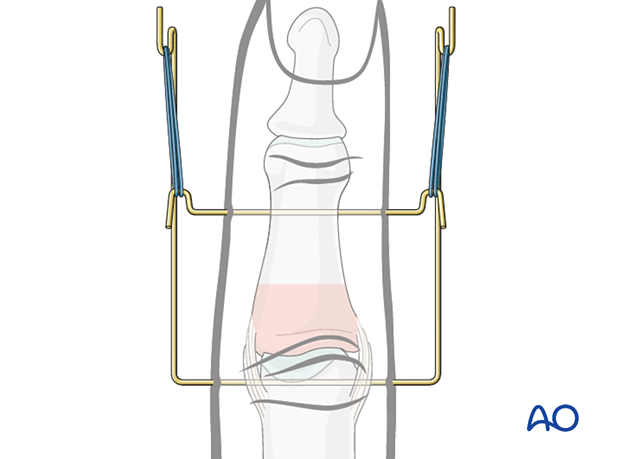
Dynamic external fixator
A dynamic external fixator may be added for 4 weeks to keep the PIP joint to length and to allow for early mobilization.
Joint transfixation with K-wire
Following articular reconstruction, if joint instability persists, the PIP joint may be transfixed with a K-wire obliquely, with the joint in 20°–30° of flexion to protect the ligament reattachment. This has a high risk of joint stiffness.
Leave the end of the K-wire outside of the skin for later removal.
The K-wire can be removed after 3–4 weeks.
9. Final assessment
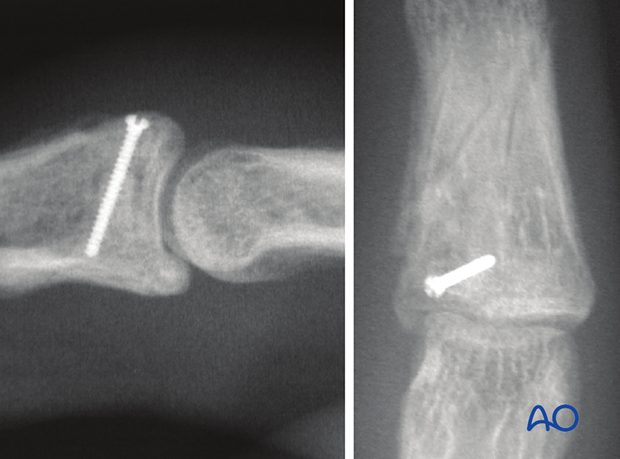
Check joint congruity using image intensification or x-ray. Reduction must be anatomical.
10. Aftercare
Postoperative phases
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.
Postoperatively
If the joint reconstruction has been supported with a dynamic external fixator, additional splinting is not necessary. Early controlled joint mobilization is encouraged.
If joint transfixation has been applied, the hand is immobilized with a dorsal splint for 3–4 weeks. This should permit movement of the unaffected fingers. The arm should be actively elevated to help reduce the swelling.
The hand should be immobilized in an intrinsic plus (Edinburgh) position:
- Neutral wrist position or up to 15° extension
- MCP joint in 90° flexion
- PIP joint in extension
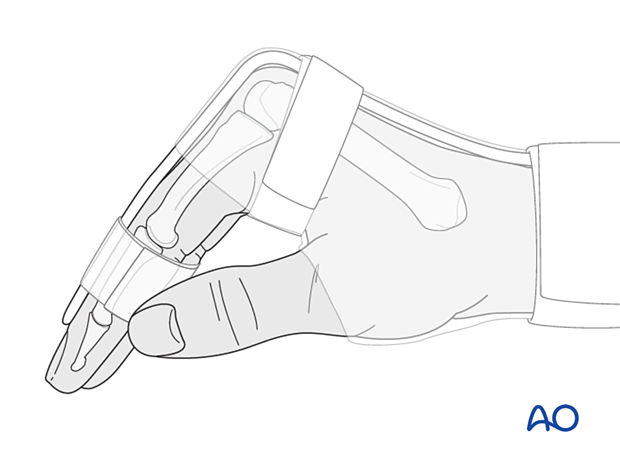
The MCP joint is splinted in flexion to maintain its collateral ligaments at maximal length to avoid contractures.
The PIP joint is splinted in extension to maintain the length of the volar plate.
Follow-up
The patient is reviewed frequently to ensure progression of hand mobilization.
In the middle phalanx, the fracture line can be visible in the x-ray for up to 6 months. Clinical evaluation (level of pain) is the most important indicator of fracture healing and consolidation.
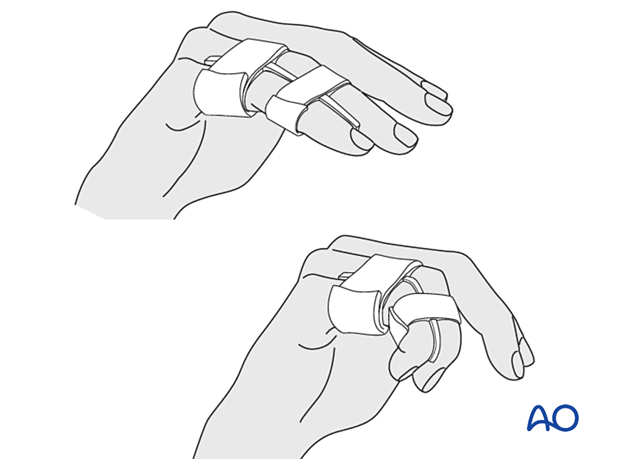
Remove the splint and K-wire after 3–4 weeks and protect the finger with buddy strapping to a neighboring finger to neutralize lateral forces on the finger.
Mobilization
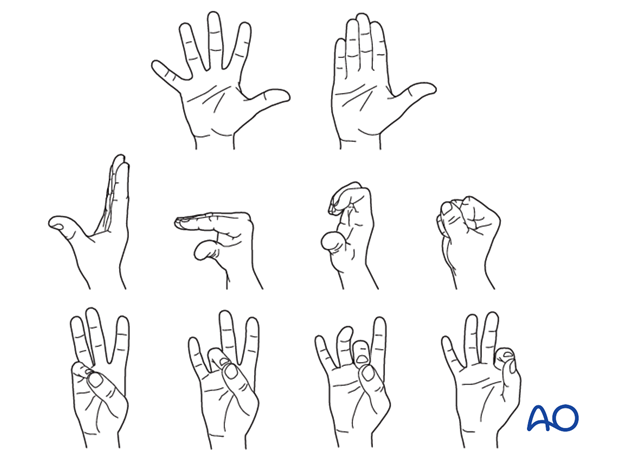
If the fixation is stable enough, the patient is encouraged to take off the splint 2–3 times daily, and to commence with gentle active exercises, provided no transarticular K-wire has been used or has already been removed.
After 4 weeks, the splint (and any K-wire or dynamic external fixator) is removed, and unrestricted active flexion and extension are permitted.
Implant removal
The implants may need to be removed in cases of soft-tissue irritation.
In case of joint stiffness or tendon adhesion restricting finger movement, arthrolysis or tenolysis may become necessary. In these circumstances, the implants can be removed at the same time.
11. Case
Multifragmentary fracture of the 4th middle phalanx with palmar impaction
AP, oblique, and …
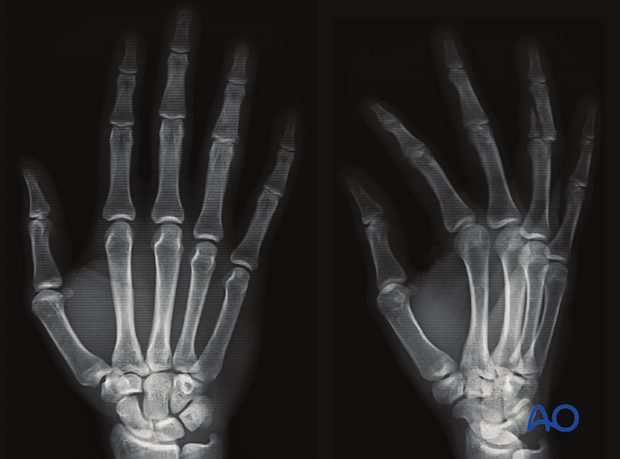
… lateral x-ray

K-wires for articular fragment stabilization and for dynamic external fixation inserted

AP view of the final construct with K-wire stabilization of the articular fragments
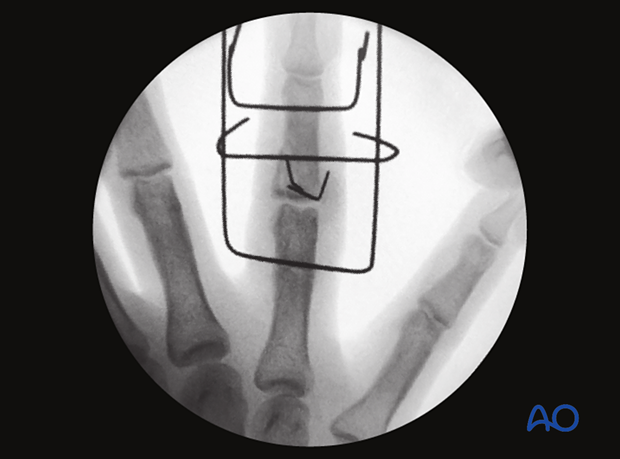
Lateral view

Final assessment of the construct and joint congruency though a range of motion

Postoperative image of the final construct