Dorsal approach to the PIP joint
1. Introduction
The dorsal approach to the proximal interphalangeal (PIP) joint offers access to the extensor tendon, joint capsule, collateral ligaments, and the distal part of the proximal phalanx and the base of the middle phalanx.
This approach may be extended proximally and distally as needed.
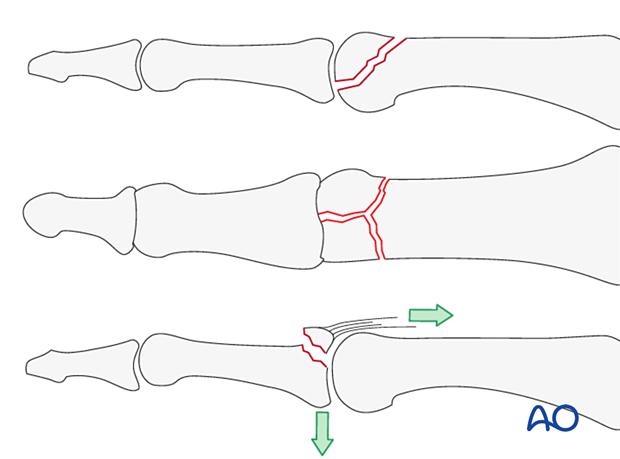
This approach is indicated for:
- Intraarticular fractures
- Dorsal coronal plane fractures of the condyles of the proximal phalanx
- Central slip avulsion fractures from the dorsal base of the middle phalanx
AO teaching video
Finger, proximal interphalangeal joint, dorsolateral approach
AO teaching video
Finger, proximal interphalangeal joint, midline approach
AO teaching video
Finger, proximal interphalangeal joint, dorsal Chamay approach
2. Surgical anatomy
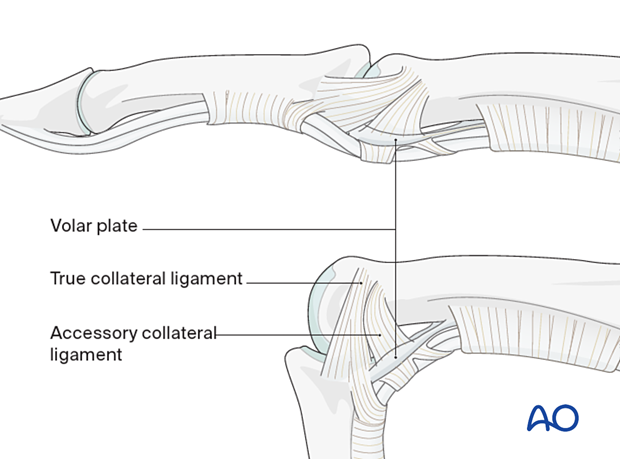
The interphalangeal joints are hinge joints. The heads of the proximal and middle phalanges each have two articular condyles that resemble a grooved trochlea and assist in preventing adduction/abduction and rotation in conjunction with the collateral ligaments.
Dynamic stability results from compressive forces, which increase during pinch and grip. Passive stability derives from the bone morphology and tension in the collateral ligaments and the volar plate. This passive stability is maximal in full extension.
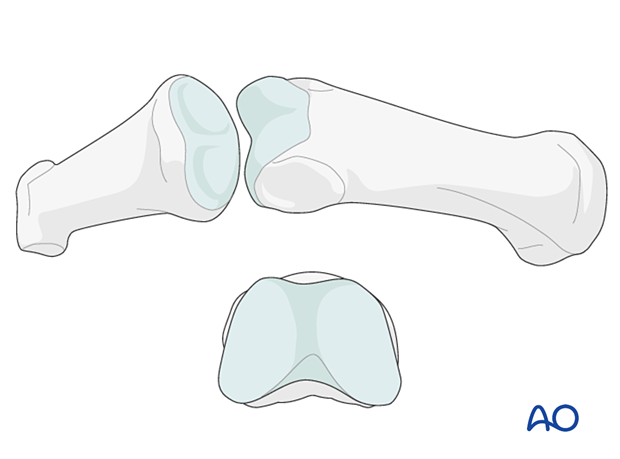
The two collateral ligaments and the volar plate are the primary structures stabilizing the interphalangeal joints and preventing displacement in the coronal plane (abduction/adduction).
The collateral ligaments also prevent side-to-side translational displacement.
The accessory collateral ligaments slacken in flexion, while the true collateral ligament is further tensioned in flexion due to the greater palmar width of the condyles.
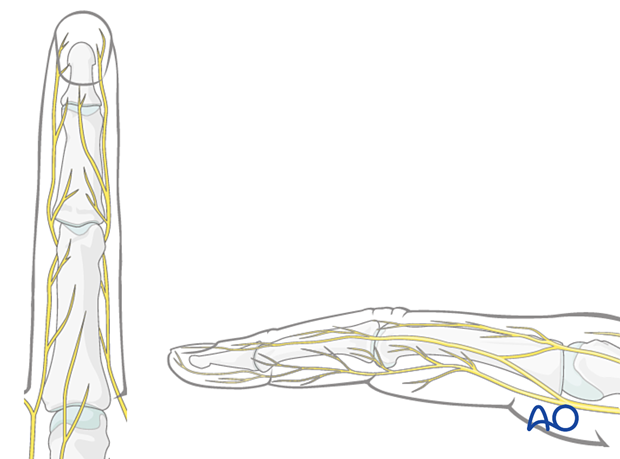
Nerve identification
Identify and protect the dorsal sensory branches of the radial and ulnar nerves in the thin subcutaneous tissue.
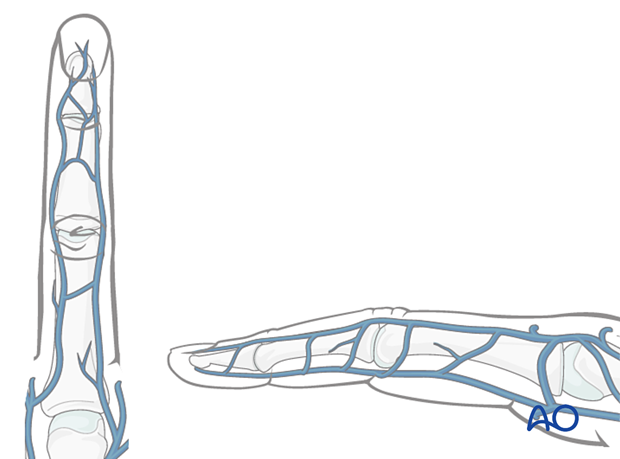
Vein identification
The dorsal venous system of the fingers has longitudinal and transverse branches. Be careful to preserve the longitudinal branches. For better exposure, the transverse branches may be ligated or cauterized but preserve as many dorsal veins as possible to avoid congestion and swelling, with consequent fibrosis and stiffness.
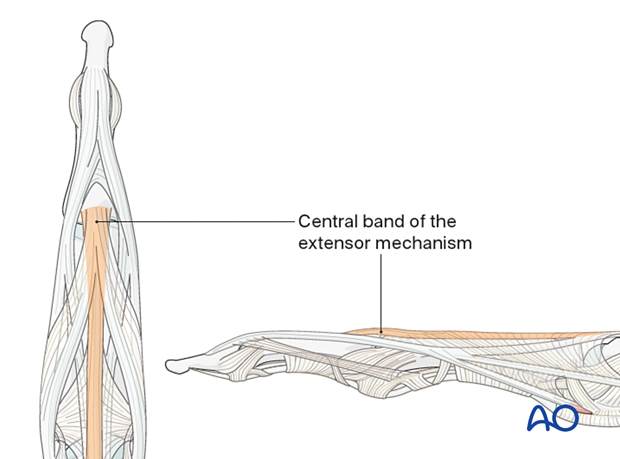
Preservation of soft-tissue structures
Preserve the insertion of the central band of the extensor mechanism to the dorsal aspect of the middle phalangeal base. If this is detached and not repaired, a boutonniere deformity may occur.
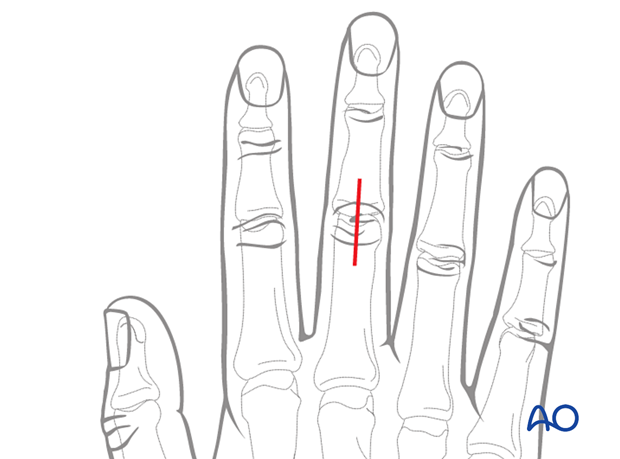
3. Skin incision
Several skin incision options are available. Each comes with benefits and disadvantages.
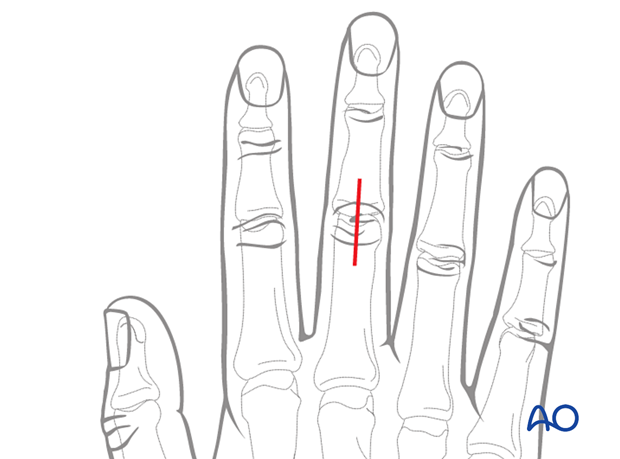
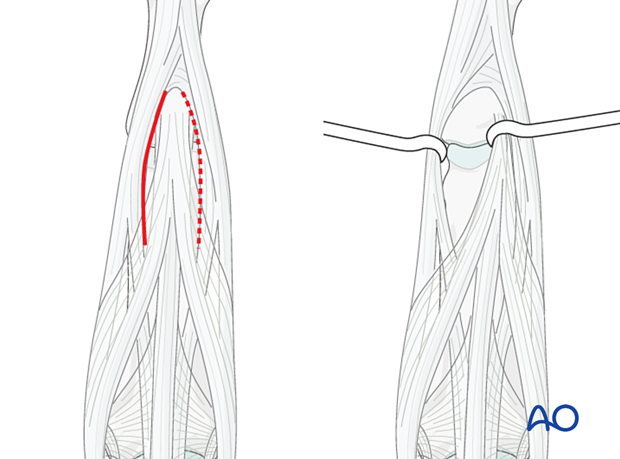
Straight dorsal incision
Perform a straight midline dorsal incision over the PIP joint.
Advantages:
- Perfusion and venous drainage are well preserved.
- Early postoperative motion will prevent scarring between the skin, tendon, and bone.
Disadvantage:
- Skin and tendon scarring are in the same line and tethering may occur.
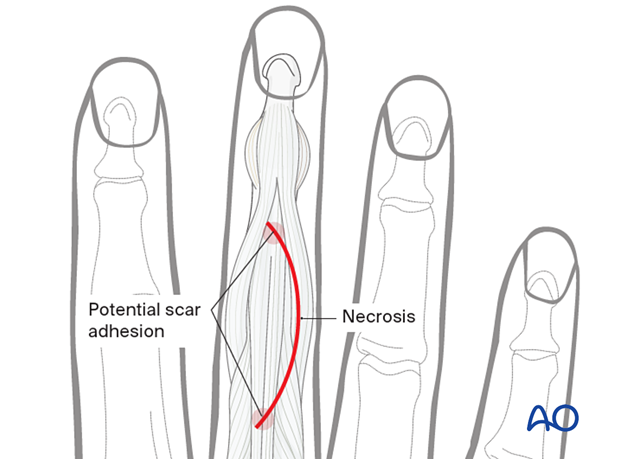
Curved skin incision
Perform a curved skin incision over the PIP joint. The convexity of the incision is planned so that the scar does not involve the radial border of the index or the ulnar border of the little finger. The fracture morphology and implant placement must be given priority when planning the incision.
Advantage:
- Skin and tendon scarring are not in line and tethering due to scarring may be avoided.
Disadvantage:
- Relatively poor perfusion at the apex of the curve may risk skin necrosis and delayed healing.
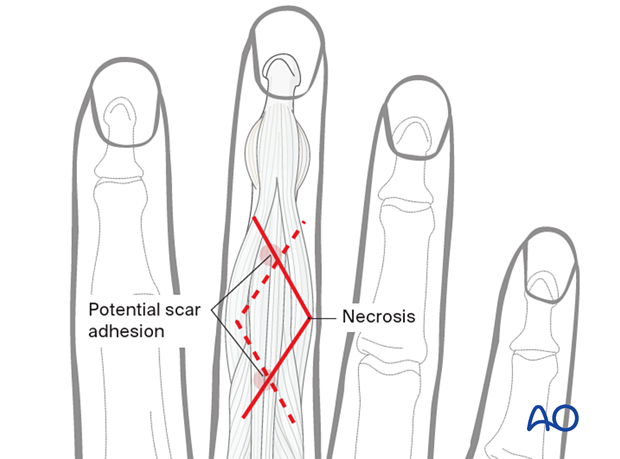
Zigzag skin incision
A zigzag incision may be used. This approach allows for:
- Full exposure of the joint and the shaft
- Paratendon or through tendon approach
Depending on the fracture pattern, the incision may be designed with an ulnar or radial apex.
The cutaneous digital nerves on the ulnar side of the 5th finger and the radial side of the 2nd finger should be preserved to protect skin sensitivity.
Advantage:
- Skin and tendon scarring are not in line and tethering due to scarring may be avoided.
Disadvantage:
- Relatively poor perfusion at the apex of the zigzag, with a risk of skin necrosis and delayed healing.
4. Skin retraction
Retract and elevate the skin and the subcutaneous tissue as a single layer. The extensor apparatus is fully exposed and intact.
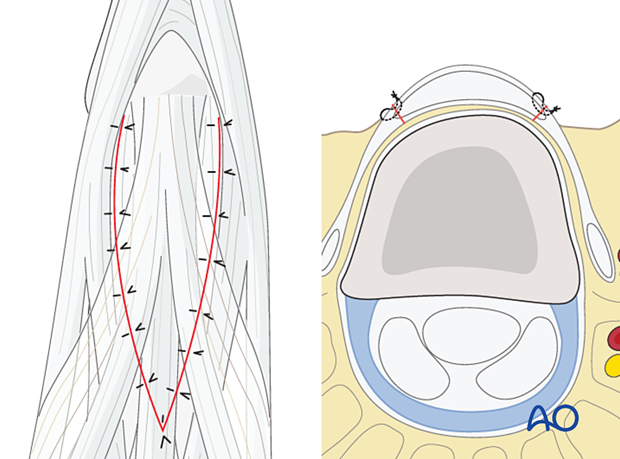
5. Tendinous approaches
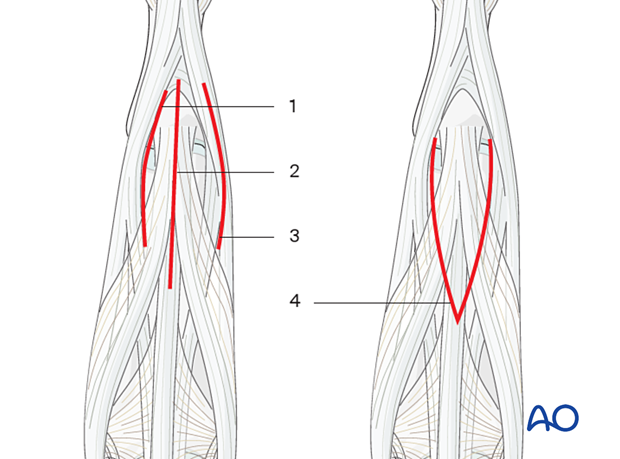
There are four possible approaches:
- Option 1: between the central and lateral extensor slips
- Option 2: Central midline extensor splitting
- Option 3: lateral to the lateral band of the extensor apparatus
- Option 4: Elevation of the central slip as a distally based, V-shaped flap (Chamay approach)
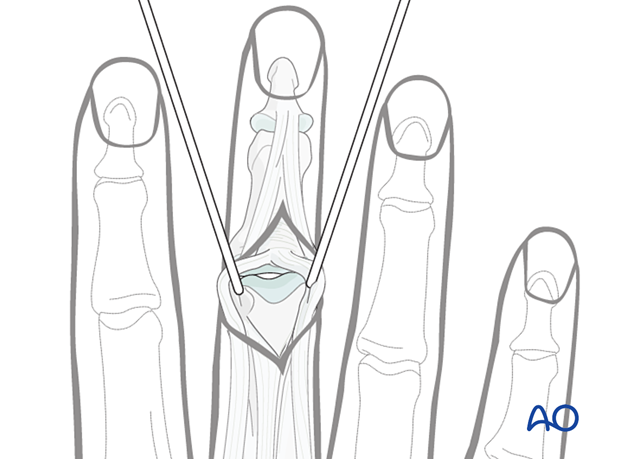
6. Option 1 – Approach between the central and lateral extensor slips (recommended)
Perform an incision in the tendon between the central slip and the lateral band.
Retraction of the slips exposes the dorsal capsule of the PIP joint.
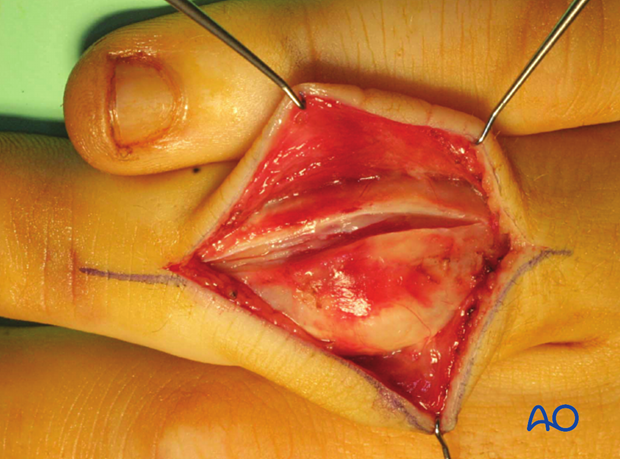
Capsulotomy
Perform a vertical capsulotomy to expose the joint.

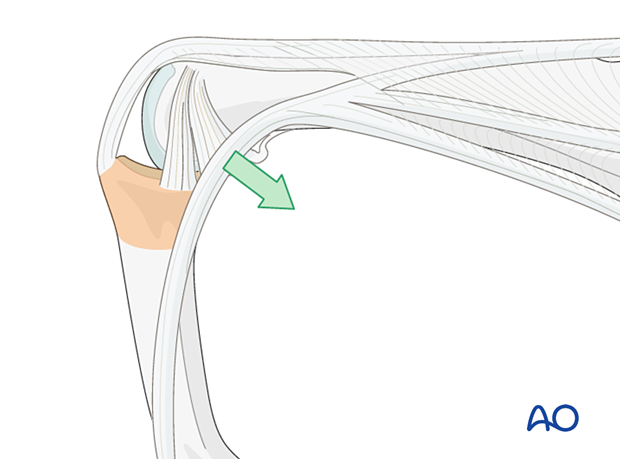
Flexion for better exposure
Flexing the PIP joint allows the lateral band to move in a palmar direction, giving better exposure to the joint.
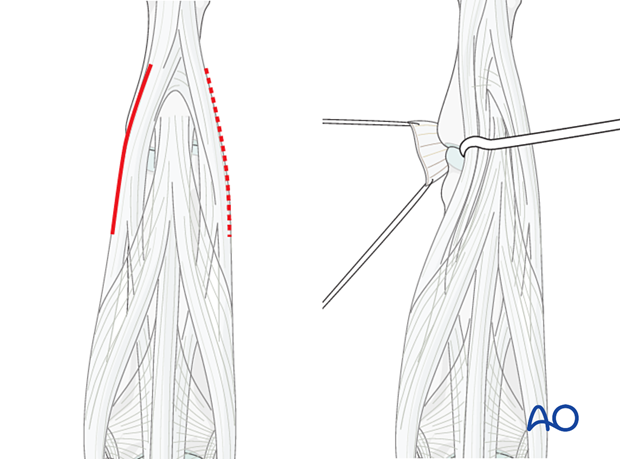
7. Option 2 – Central midline extensor splitting
Perform a straight incision and perform a longitudinal midline tenotomy.
The disadvantage of this approach is the possibility of developing a boutonnière deformity or lack of extension.
8. Option 3 – Approach lateral to the lateral band of the extensor apparatus
Incise lateral to the lateral band.
Divide the transverse retinacular ligament (TRL), using a dental pick inserted between it and the collateral ligament, to avoid accidentally cutting the collateral ligament.
A longitudinal capsulotomy allows the joint to be inspected.
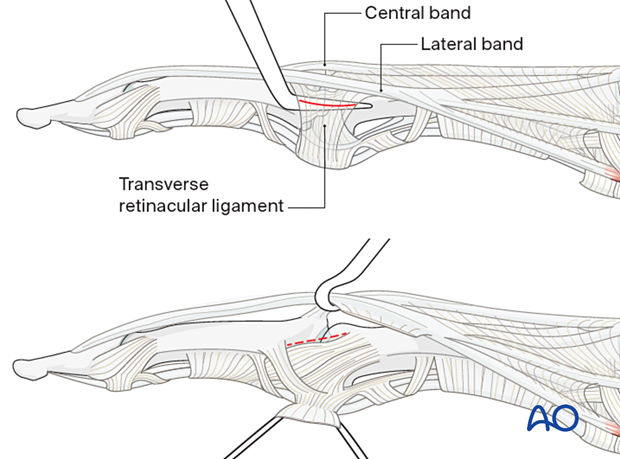
9. Option 4 – Elevation of the central slip as a distally-based, V-shaped flap (Chamay approach)
Raise the central extensor slip as a distally based, V-shaped flap, leaving it attached to the base of the middle phalanx.
Perform a transverse dorsal capsulotomy.
Flexing the joint causes the lateral band to slip in a palmar direction, exposing the whole joint.
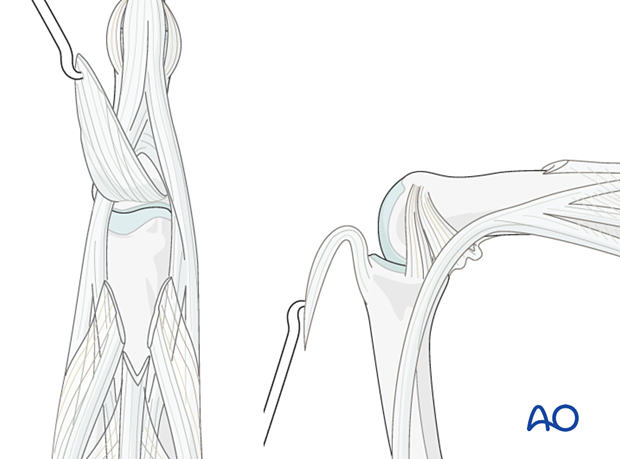
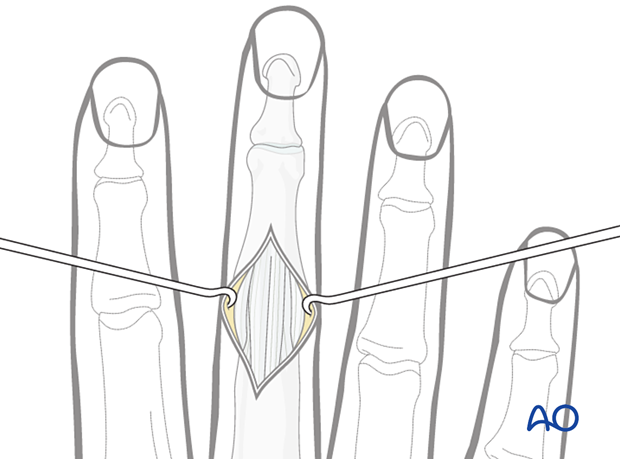
10. Wound closure
Regardless of the chosen approach, all tendon incisions must be repaired with nonabsorbable monofilament sutures with an atraumatic needle prior to wound closure.
The following suture dimension should be used:
- 4.0 for central tendon repair
- 6.0 for associated ligament and periosteum repair
Cover any metallic implants with the periosteum as far as possible; this helps minimize contact between the extensor tendons and the implant.