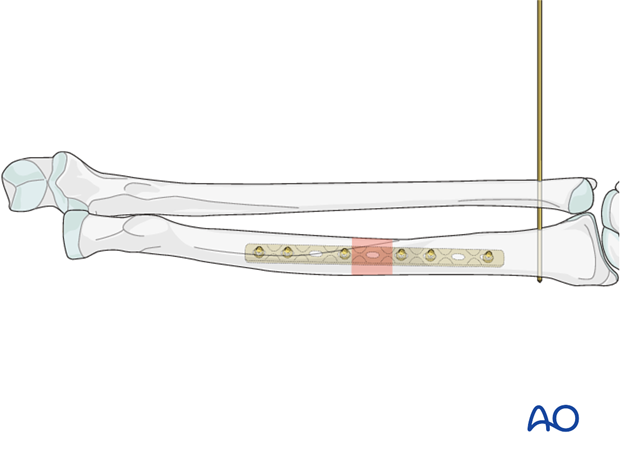
DRUJ stabilization (Galeazzi fracture-dislocation)
1. General considerations
Galeazzi fracture-dislocation
In Galeazzi fracture-dislocations the radial shaft fracture is associated with a dislocation of the head of the ulna at the distal radioulnar joint (DRUJ).
Most often, the ulnar head dislocation is posterior (dorsal), very seldom anterior (volar).
Galeazzi fracture-dislocations are relatively rare (3 - 6% of forearm shaft fractures).
Anatomical reduction and fixation of the radial fracture usually lead to spontaneous reduction of the distal radioulnar displacement.

In Galeazzi fracture-dislocations, anatomical reduction and stable fixation of the radius are mandatory if accurate and stable reduction of the ulnar head and a satisfactory outcome are to be achieved.
Once operative fixation has been completed, the surgeon must ensure the stability of the reduced ulnar head, preferably under image intensification. If the ulnar head cannot be reduced, exploration of the DRUJ is usually required. If the ulnar head is reducible, but is unstable, verify that the radial reduction is anatomical. If the radius is satisfactory, then the rotational forearm position in which the ulnar head is most stable will be the position for postoperative splinting. Transfixation of the DRUJ with one or more K-wires has been used but has to be regarded as the last resort.
Order of reduction and fixation
First, the radius will be reduced and fixed openly. Then check the position of the ulnar head, which reduces spontaneously in most cases. If the ulnar head is irreducible, or unstable, further steps need to be undertaken and these will be described in detail later.
Note on approaches
In Galeazzi fracture-dislocations, the approach to the radius can be either a Henry approach or a posterolateral approach depending on surgeon’s preference.
If the ulnar head does not spontaneously reduce after radial fracture reduction and fixation, a separate approach to the distal radioulnar joint (posterior or anterior) will be necessary.
2. Galeazzi fracture-dislocation
After fixation of the radius, check the position of the ulnar head throughout the range of forearm motion. The ulnar head reduces spontaneously in most cases. Stability is tested manually by rotating the forearm from pronation to supination whilst palpating the ulnar head.
Provided stability is assured, it is recommended to immobilize the DRUJ for 3 weeks in a removable splint, which controls forearm rotation, to allow for ligamentous healing.
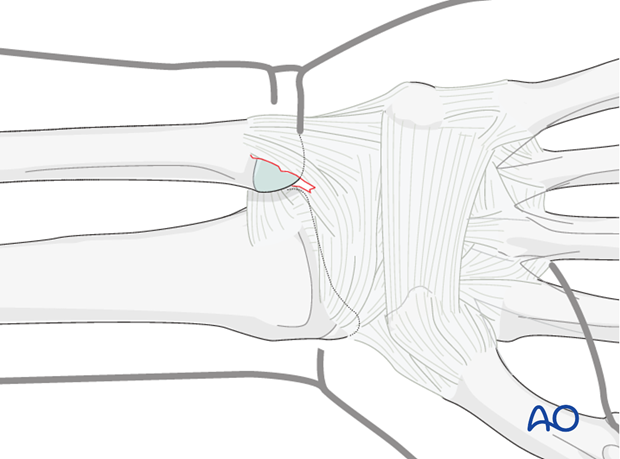
If the ulnar head is irreducible and the radial fixation is anatomical, immediate exploration of the DRUJ is necessary to deal with any ligamentous interposition or other obstruction (tendon). With posterior dislocations of the ulnar head, very occasionally the extensor carpi ulnaris tendon can become entrapped.
If instability of a reducible ulnar head is persistent, additional stabilization is recommended.
The forearm should be examined to determine in which rotational position the DRUJ is restored. This will become the position for postoperative splintage. If the ulnar head is grossly unstable, temporary K-wire transfixation of both bones in a neutral position or in supination (as illustrated) can be the only solution. Such K-wire stabilization should be retained for 3-4 weeks postoperatively and forearm rotation prevented by appropriate casting.
1) Open reduction
Open exploration of the DRUJ with extraction of interposed soft tissues and their repair is needed in the rare cases where closed reduction of the DRUJ can not be achieved or maintained.
The approach chosen (whether anterior or posterior) depends on the direction of the displacement of the ulnar head.
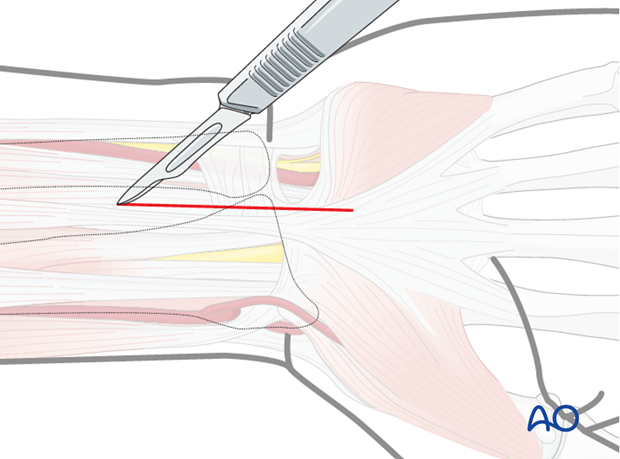
The posterior approach to the DRUJ is via the interval between the 4th and 5th extensor compartments.
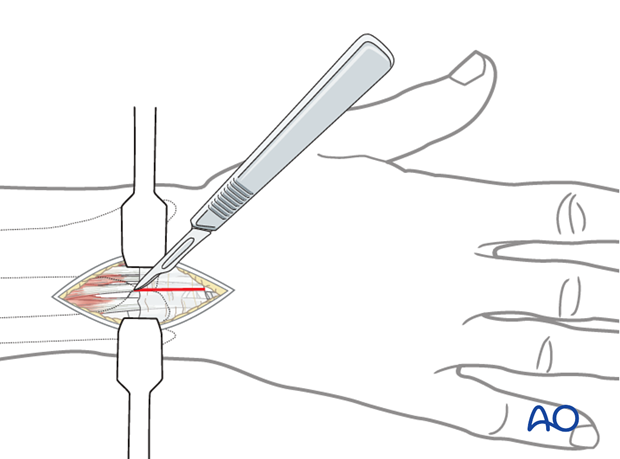
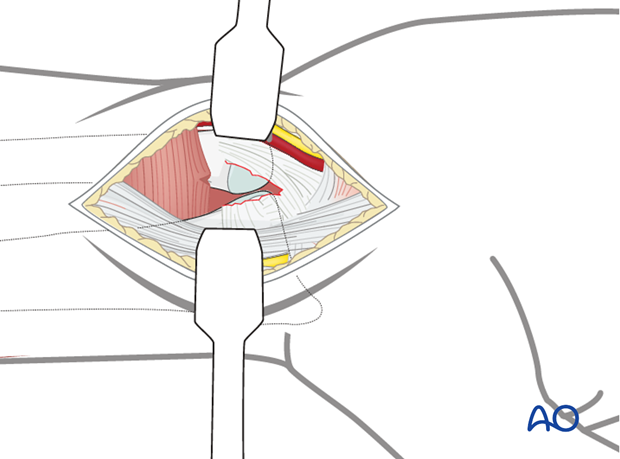
Gently retract the displaced ulnar head in order to inspect the interior of the joint for interposed soft-tissue or cartilage fragments. Clear the joint, reduce the ulnar head, usually by supination, and suture the torn edges of the articular capsule using interrupted resorbable sutures.
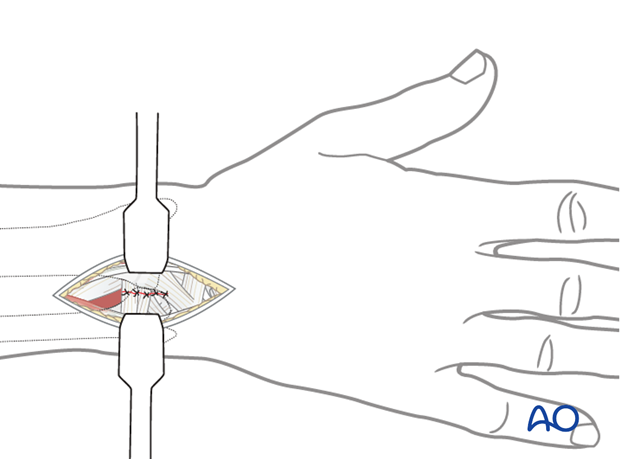
To avoid any redislocation, immobilization of the forearm in the rotational position of maximal stability is usually achieved using a cast or a removable brace that controls forearm rotation.
Temporary K-wire transfixation in the stable position is used electively by some surgeons and may become necessary if there is unacceptable residual instability after ligamentous repair.
To approach the DRUJ from the anterior aspect involves considerable deep dissection between important anatomical structures and should be avoided if possible. Fortunately, anterior dislocation of the ulnar head is rare. If the anterior approach to the radial fracture can be extended distally without major further dissection, the DRUJ can be approached in this manner, elevating pronator quadratus. By retracting the dislocated ulnar head, a limited view into DRUJ is possible and this may suffice for removal of interposed soft tissue.
Reduce the ulnar head; this is usually achieved by pronation. It is not usually possible to suture the torn ends of the articular capsule.
N.B.: In this illustration, the divided pronator quadratus muscle has been omitted for purposes of clarity.
To avoid any redislocation, immobilization of the forearm in the rotational position of maximal stability is usually achieved using a cast or a removable brace which controls forearm rotation.
Temporary K-wire transfixation in the stable position is used electively by some surgeons and may become necessary if there is unacceptable residual instability after ligamentous repair.
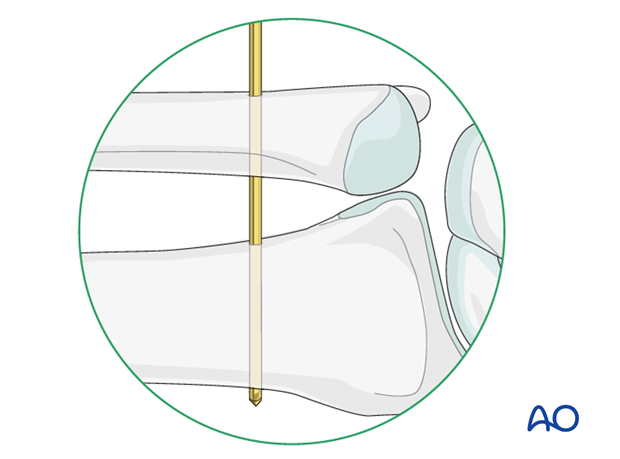
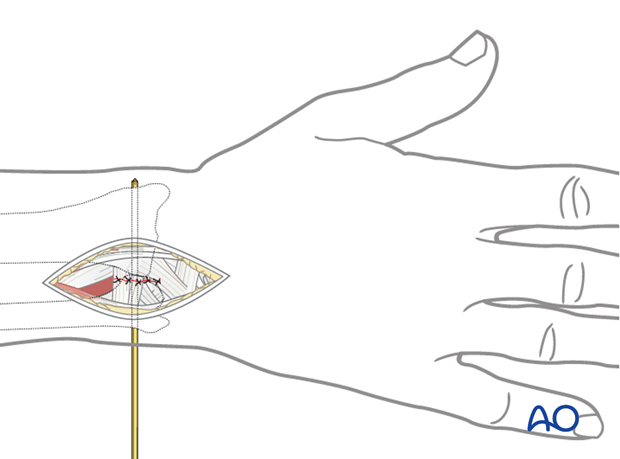
2) Closed reduction and transfixion
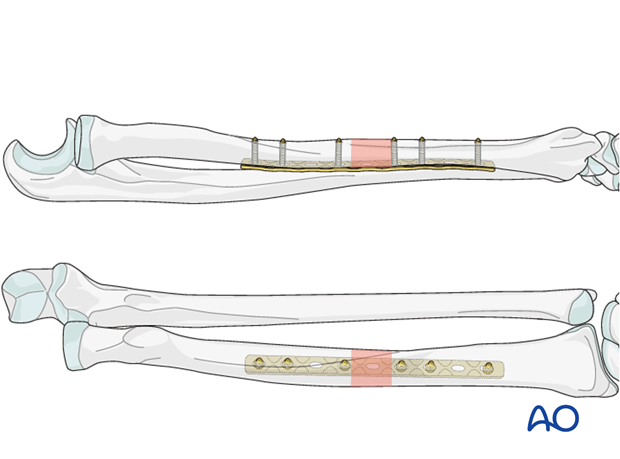
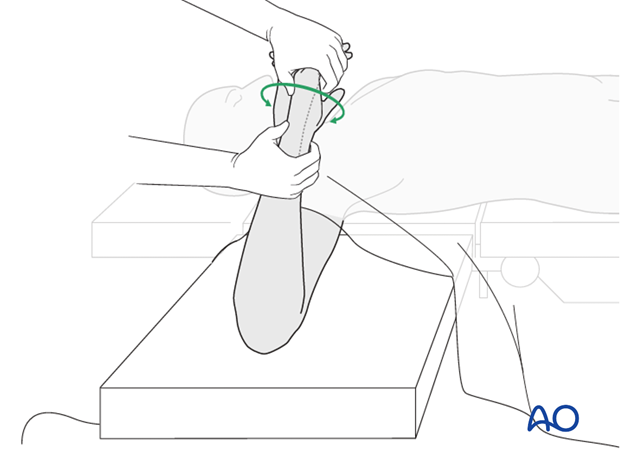
Closed reduction is maintained by temporary (3-4 weeks) transfixion of the two bones using K-wire transfixion proximal to the DRUJ. It is recommended to insert the K-wire(s) in the position of the forearm in which the ulnar head proves to be most stable.
Stability is usually in a neutral or supinated position (as illustrated), except in the rare cases of anterior displacement of the ulnar head. Most surgeons recommend cast or brace splintage of forearm rotation during the period of K-wire transfixion.
Pitfall: instability of ulnar head
Be aware that malreduction of the radius will lead to failure of spontaneous anatomical relocation of the ulnar head and subsequent instability. Such a situation will require revision of the radial fixation if optimal forearm function is to be restored.
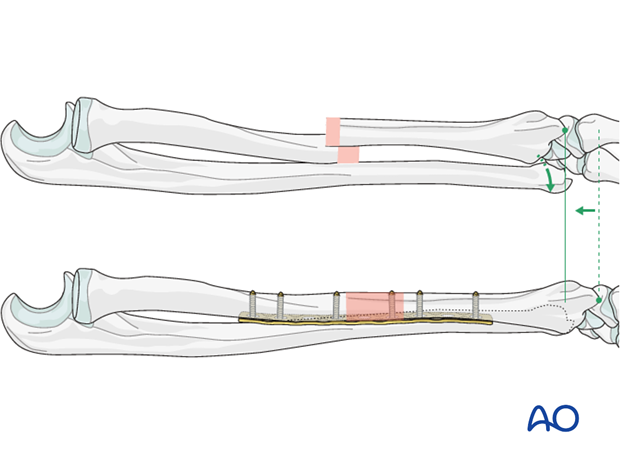
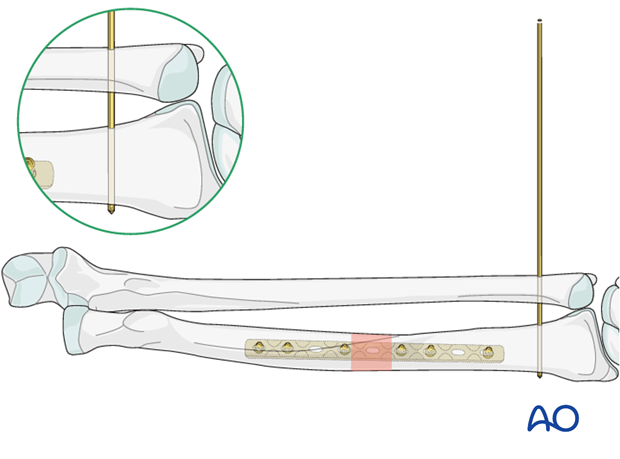
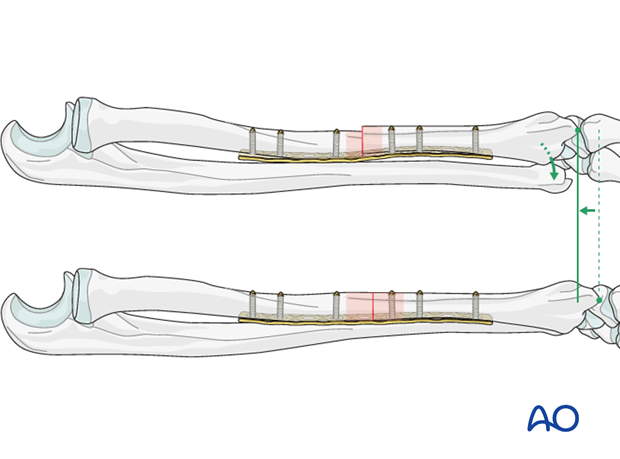
In the upper part of this illustration, the radius has been fixed in a position of displacement and shortening. This has prevented spontaneous reduction of the ulnar head.
In the lower part of the illustration, anatomical reduction of the radius has led to spontaneous reduction of the ulnar head.
3. Check of osteosynthesis
Check the completed osteosynthesis by image intensification. Make sure that the plate is at a proper location, the screws are of appropriate length and a desired reduction was achieved.
In those cases in which DRUJ transfixion has not been used, confirm the rotational position which affords maximal stability of the ulnar head. This will be the forearm position in which postoperative forearm splinting will be applied.
4. Assessment of Distal Radioulnar Joint (DRUJ)
Before starting the operation the uninjured side should be tested as a reference for the injured side.
After fixation, the distal radioulnar joint should be assessed for forearm rotation, as well as for stability. The forearm should be rotated completely to make certain there is no anatomical block.
Method 1
The elbow is flexed 90° on the arm table and displacement in dorsal palmar direction is tested in a neutral rotation of the forearm with the wrist in neutral position.
This is repeated with the wrist in radial deviation, which stabilizes the DRUJ, if the ulnar collateral complex (TFCC) is not disrupted.
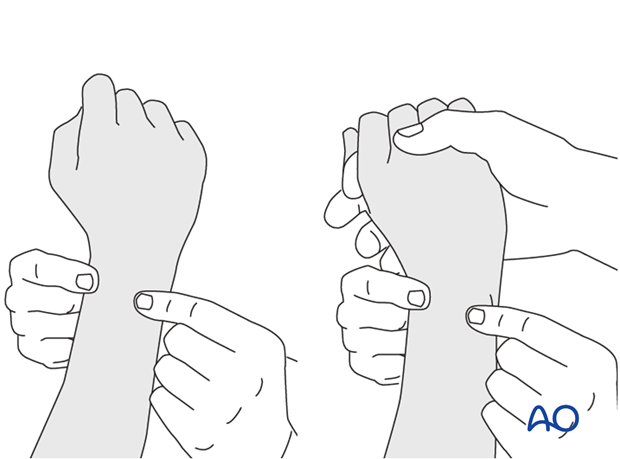
This is repeated with the wrist in full supination and full pronation.
Method 2
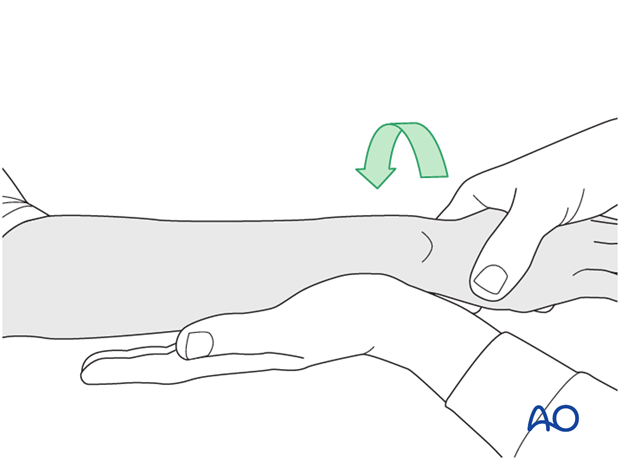
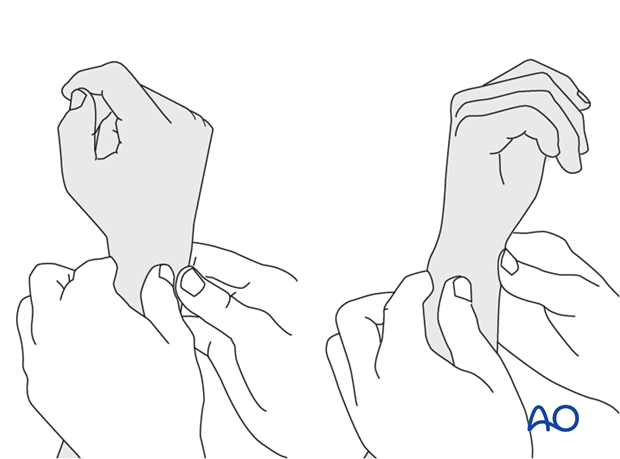
In order to test the stability of the distal radioulnar joint, the ulna is compressed against the radius...
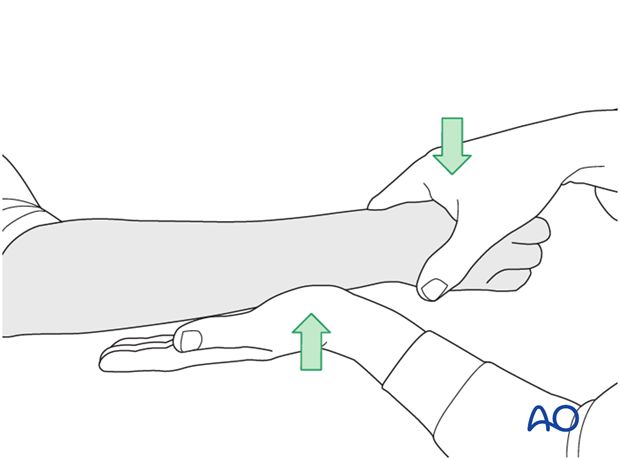
...while the forearm is passively put through full supination...
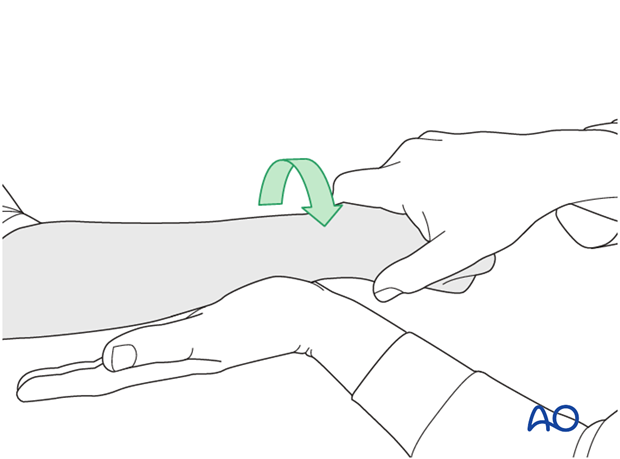
...and pronation.
If there is a palpable “clunk”, then instability of the distal radioulnar joint should be considered. This would be an indication for internal fixation of an ulnar styloid fracture at its base. If the fracture is at the tip of the ulnar styloid consider TFCC stabilization.