ORIF - Lag screws with or without plate
1. Introduction
The principle of this procedure is first to reduce and fix the articular block. The articular block is then fixed to the main fragment using lag screws. (Lag screws are contraindicated in cases of comminution.)
Anatomical reduction of the joint surface is essential to prevent chronic instability or posttraumatic degenerative joint disease.
Toe fractures versus long bone fractures
Toe fractures are different from long bone fractures.
- The bones are very small
- Fracture gaps are small
- Fixation devices don't need to counter large forces
Thus, following the AO principles is less critical than for long bones, and often isolated screws or K-wires alone will work satisfactorily.
Restoration of length, rotation, and angulation are important for cosmesis.
The hallux is particularly critical due to its importance for walking.
Timing of surgery
The timing of surgery is influenced by the soft tissue injury and the patient's physiologic status.
Dislocation or injuries associated with the skin at risk requires immediate intervention regardless of the amount of soft tissue swelling.
If possible, swelling should be significantly decreased before surgery, which can take up to two weeks in some instances.
Open fractures should be promptly irrigated and debrided, and treated with antibiotics. Definitive fracture fixation may not be possible during this setting.
Forefoot fractures do not contribute to physiologic instability. If there is no soft tissue at risk, urgent intervention is not required.
2. Patient preparation and approach
Patient preparation
This procedure is typically performed with the patient placed supine and the knee flexed 90°.

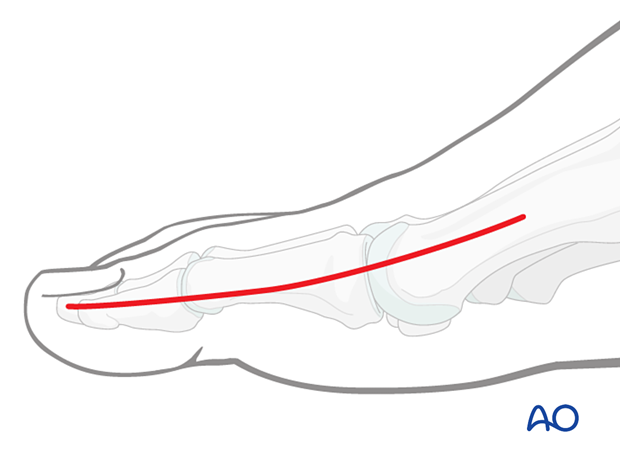
Approach
These fractures can be approached through either the:
Extension of the medial incision allows for visualization of the entire dorsal surface.
Lag screws may be inserted percutaneously.
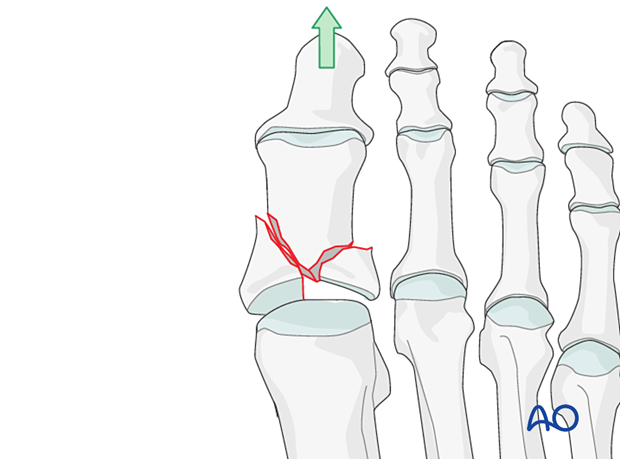
3. Reduction
Visualization
Visualization of the joint is challenging but can be improved by longitudinal distraction or a percutaneous reduction aid such as a mini distractor.
Visualization of the joint may be further improved by releasing the dorsal insertion of the extensor hallucis brevis.
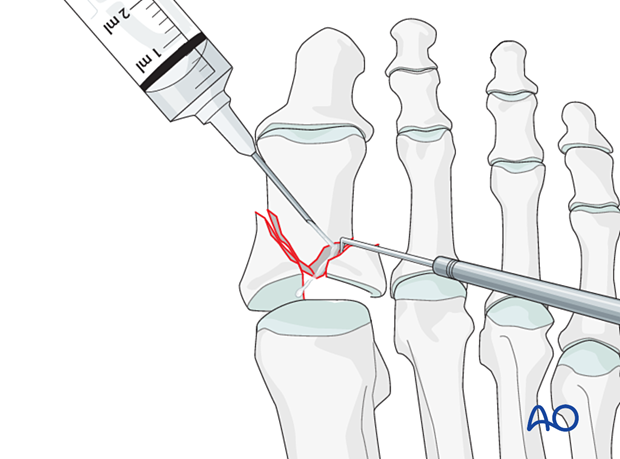
Irrigation and debridement
Clean the fracture using a dental pick. Direct suction or irrigation is helpful.
The fracture edges are exposed, and the fragment mobility is assessed. It is essential to maintain the vascularity of small fragments.
The extent of articular involvement is assessed, including separate osteochondral fragments.
If reconstruction of the articular surface is not feasible, a fusion of the joint should be considered.
Reduction and temporary fixation of the articular block
Reduction forcepsReduce and temporarily fix the articular block with pointed reduction forceps.
Be careful not to apply excessive force as this can lead to fragmentation. If possible, apply the reduction clamp so that the forces created by the clamp are at right angles to the fracture line. This clamp placement helps in reducing the fracture and in applying compression.
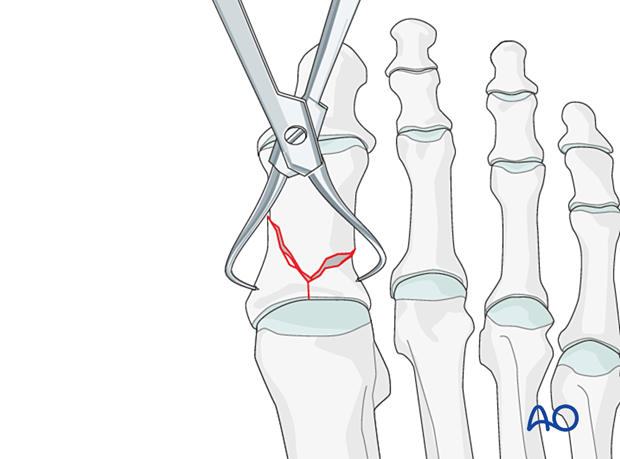
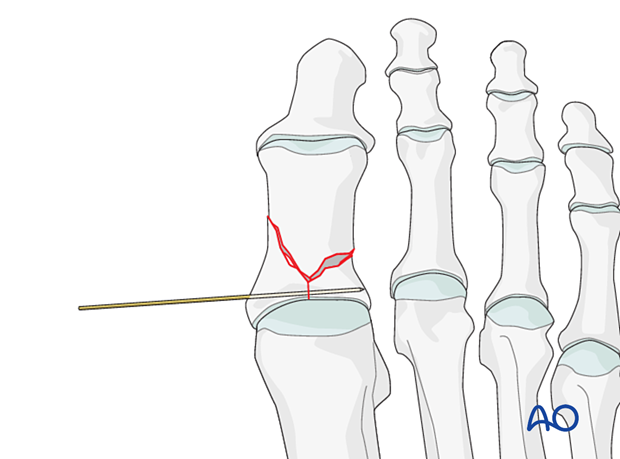
Insert a K-wire into one of the articular fragments and use it as a joystick to reduce the articular block. Once reduction is accomplished, advance the wire to secure the reduction.
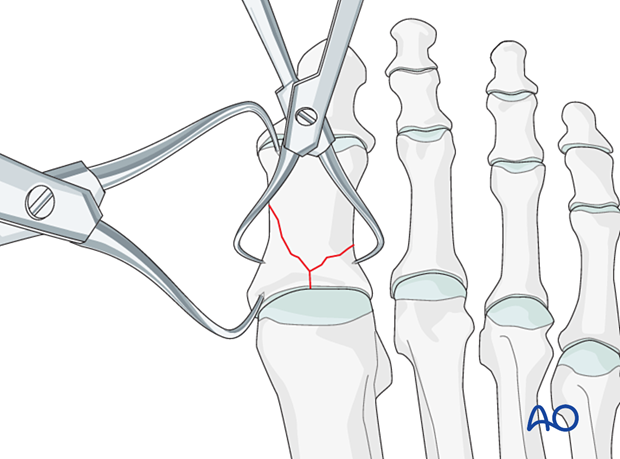
Reduction of the articular block to the shaft
Reduce the articular block to the shaft and restore anatomical axial rotation, length, and angulation.
A reduction forceps can be used to both perform and secure the reduction.
Alternatively, a K-wire can be used as a joystick to reduce the fracture and secure the reduction (as described above).
A periosteal elevator used as a lever may be helpful.
Verify length, rotation, and angulation.
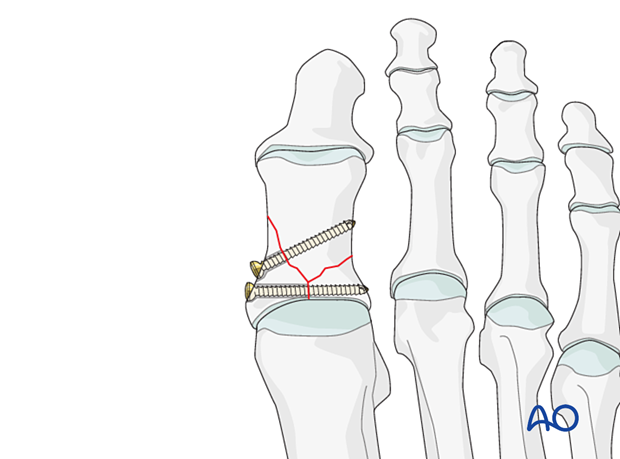
4. Fixation
Fixation of articular block
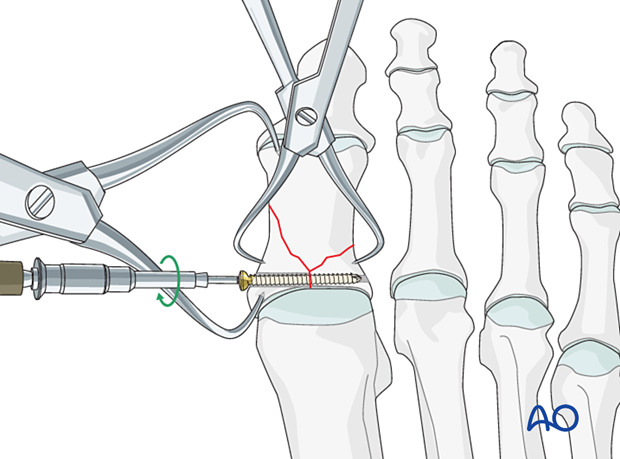
Fixation of the articular block to the diaphysis
Insert one bicortical lag screw to secure the articular block to the diaphysis.
Apply a plate if this screw fails to fix the shaft component adequately.
5. X-rays
Obtain x-rays to confirm alignment and hardware placement.
6. Aftercare
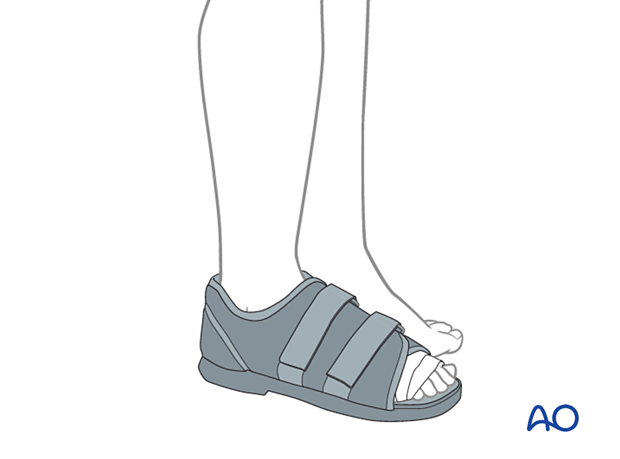
Weight-bearing may be allowed as long as the patient is provided with a flat, rigid sole shoe, which is continued for six weeks until X-rays or clinical examination is consistent with healing.
If the fracture construct does not involve transarticular fixation and is stable, range of motion exercises (both actively and passively) may be initiated once soft tissues permit.
7. Case
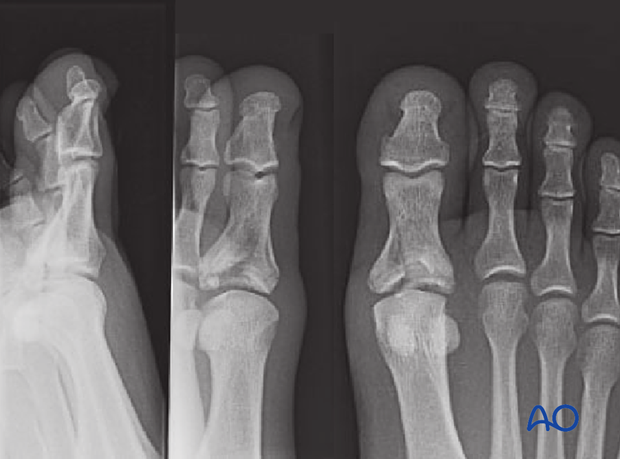
The patient had kicked a door in this case, resulting in a multifragmentary fracture of the hallux's proximal phalanx base.
The joint was multifragmentary requiring open reduction.
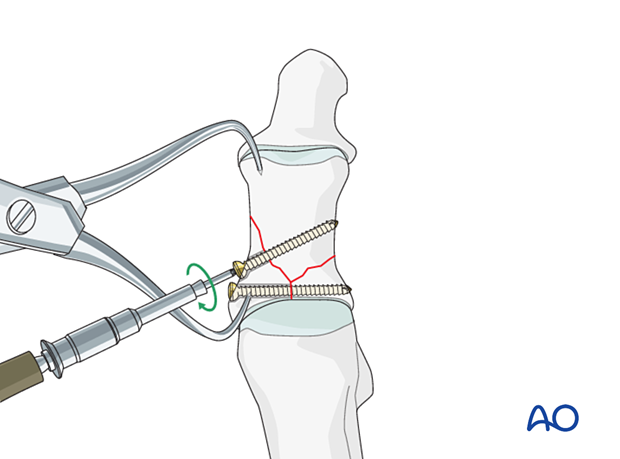
Intraoperative image showing a reduction clamp with the comminuted fracture and the joint surface reduced.
The joint surface was accurately reconstructed without the need of a bone graft.
A depth gauge is here being used to measure the required screw length.

The main fragment was fixed with an isolated lag screw. Because this bone is so tiny, no attempts were made to fix any other fragments.
The x-ray that the comminuted joint surface was still satisfactorily reduced postoperatively.
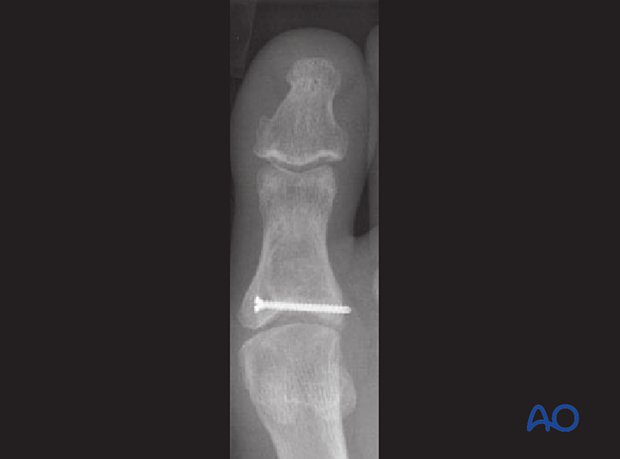
Lateral view














