Anterior lag screw
33B3.1 Partial articular fracture, frontal/coronal, anterior and lateral flake
- 1/6 – Principles
- 2/6 – Preparation and approach
- 3/6 – Reduction
- 4/6 – Fixation outside of the articular surface
- 5/6 – Fixation through articular surface
- 6/6 – Aftercare
1. Principles
General considerations
Anterior and lateral flake fractures may be associated with patellar dislocation/subluxation.
These osteochondral fragments are very often avascular, and their incorporation occurs by “creeping substitution” as vessels grow into the fragment from the living underlying cancellous bone. This requires the abolition of all interfragmentary movement by rigid interfragmentary compression. If this is not achievable, then nonunion and late separation can occur. For this reason, smaller fragments may need to be excised, or washed out of the knee joint.
Osteochondral fractures of the medial, or lateral, ridge of the patellar groove of the femur will usually require open parapatellar approach for reduction and fixation. When full arthroscopic resources, including an expert surgeon, are available, arthroscopic reduction and percutaneous fixation may be considered, but require high levels of skill and expertise.
Check the retropatellar surface for lesions.
In these injuries, there may be small osteochondral defects that are not reconstructable. Every reasonable attempt should be made to reconstruct the articular surface. On the other hand, a loose small fragment in the knee joint is clinically worse than a small articular defect. Therefore, surgical judgment must be exercised in determining whether a fragment is reconstructable, or not.
Specialist knee reconstruction surgeons have available advanced techniques to reconstruct the articular surface. Osteochondral autograft and allograft transfer within the knee are possible. Cultured chondrocyte grafting shows promise for the future.
2. Preparation and approach
Approaches
HeadlineL4Osteochondral fractures of the medial or lateral ridge of the patellar groove of the femur will usually require an open medial or lateral parapatellar approach for reduction and fixation.
When full arthroscopic resources, including an expert surgeon, are available, arthroscopic approach and reduction and percutaneous fixation may be considered, but require high levels of skill and expertise.
3. Reduction
Reduction
Achieve reduction by manipulating the fracture with an elevator. Small ball-spiked pushers, or a dental pick, may also be used.

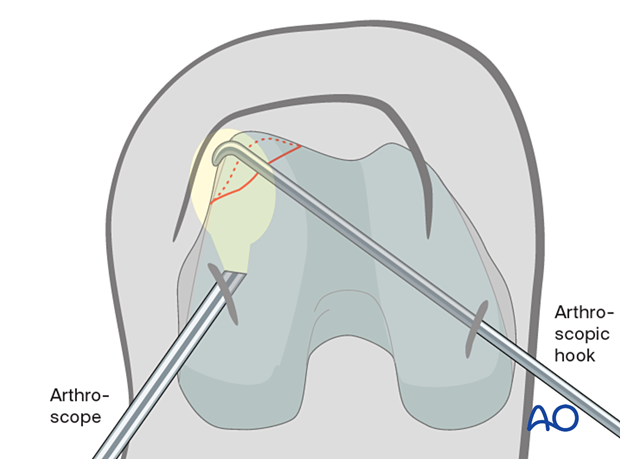
Alternative: reduction under arthroscopic view
Achieve reduction by manipulating the fracture with the hook (illustrated) using arthroscopic control. Small ball-spiked pushers may also be used, inserted through separate portals.
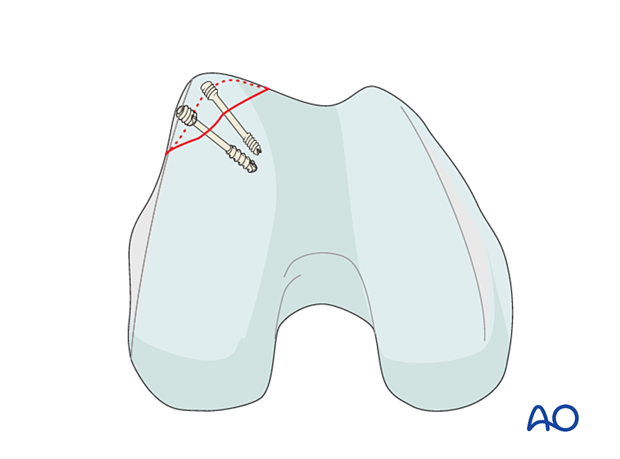
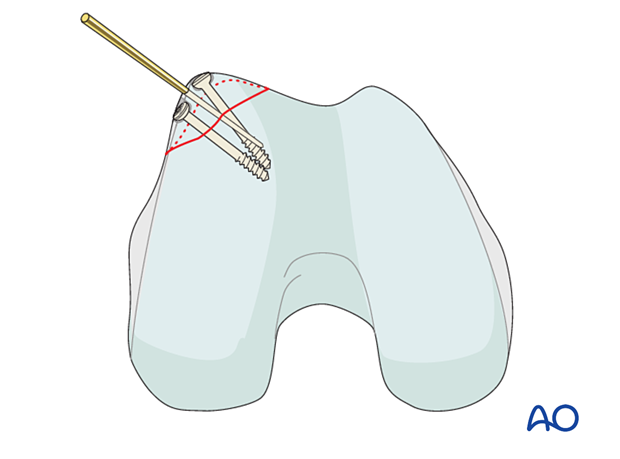
Temporary fixation
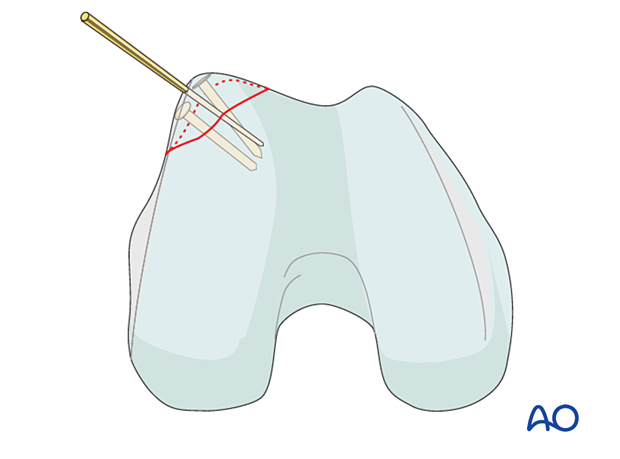
Insert a K-wire to secure the reduction. Make sure that it does not interfere with the intended implant position.
If possible K-wires should be inserted outside of the cartilage surface.

4. Fixation outside of the articular surface
Lag screws are inserted using the standard technique before removing the K-wires.
5. Fixation through articular surface
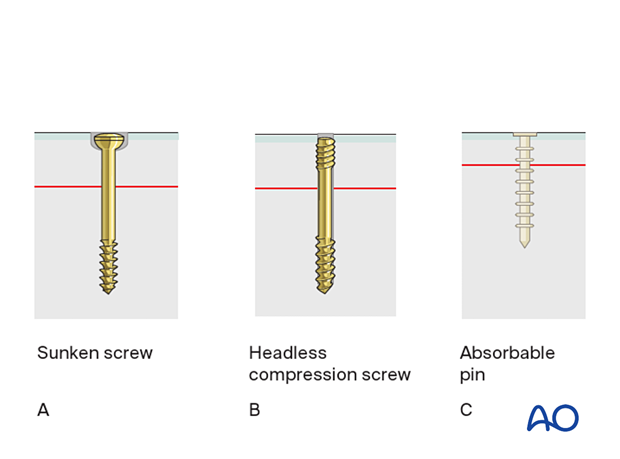
General consideration
Fixation can be achieved using a small fragment screw system (A or B), or absorbable pins (C). In general screws provide a better compression of the fracture, but need a certain thickness of the osteochondral flake due to the screw head dimension.
Absorbable pins (C) are preferable for thin and small fragments.
Two screws, or pins, should be used in order to prevent fragment rotation.
None of the implants is allowed to project above the articular surface.
Guide-wire placement
Place the guide wires as perpendicularly as possible to the fracture plane.
Check correct guide-wire placement under image intensifier control.
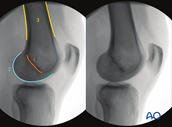
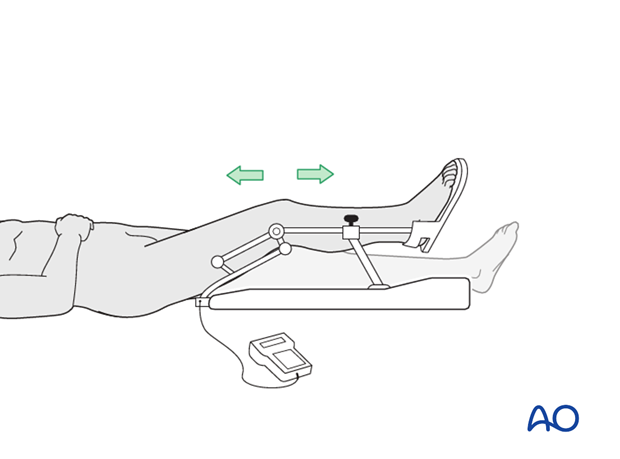
Optimal views and anatomical landmarks
Intraoperative imaging of the knee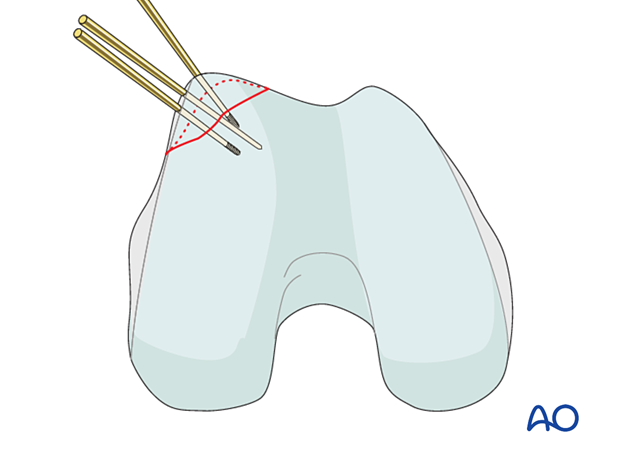
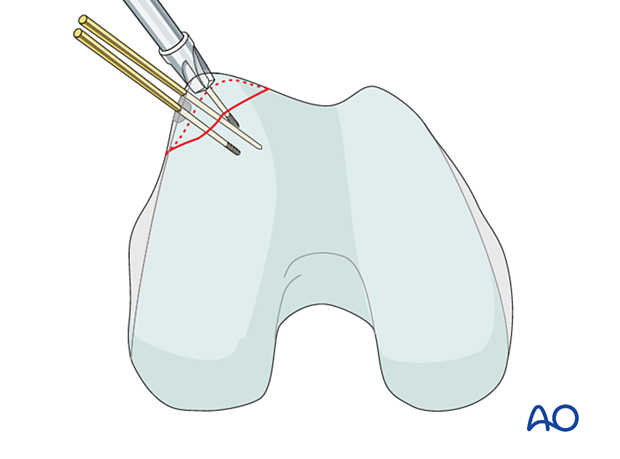
Countersinking
Countersink manually, deep enough to allow for fully buried screw heads.
Be aware of countersinking too deeply into the cancellous bone, which often happens using a power tool.
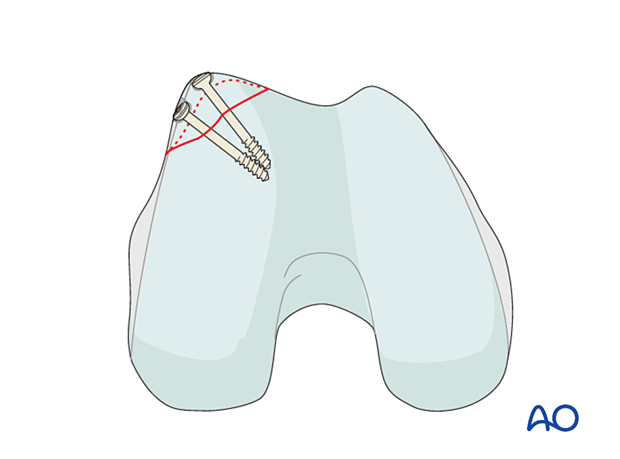
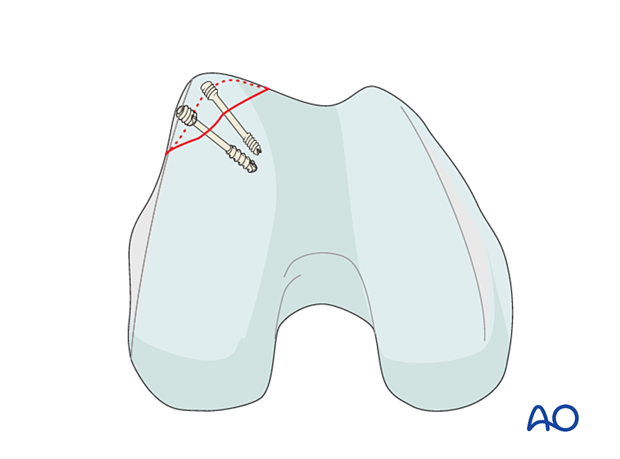
Sunken screws
In screw fixation, the lag screw principle is followed. Use partially threaded lag screws so that no gliding hole needs to be drilled. It is imperative to countersink for the screw head.
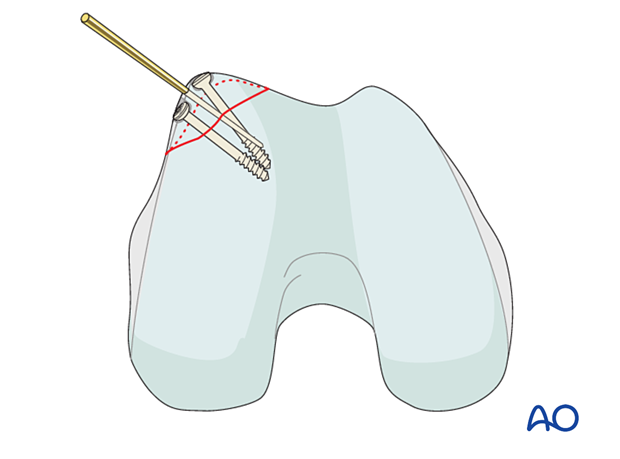
This illustration shows the completed osteosynthesis using sunken screws.
Headless compression screw
Insert 3.0 mm headless compression screws with predrilling, or over a guide wire. Neither gliding hole nor countersinking is required. It is imperative to insert the headless compression screw until the screw head has passed the cartilage surface completely.
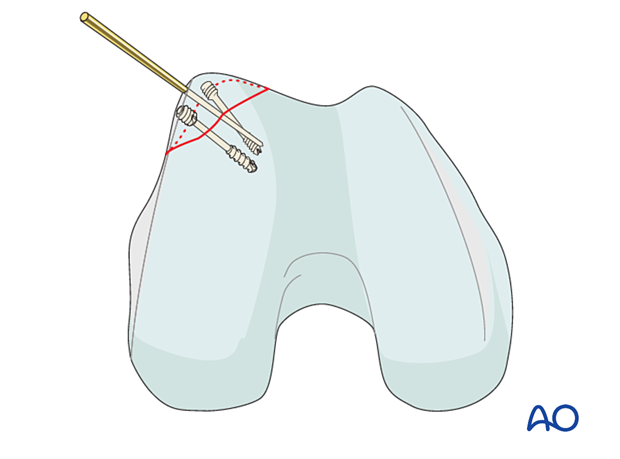
This illustration shows the completed osteosynthesis using headless compression screws.
Absorbable pins
Absorbable pins require predrilling. Use the insertion device to insert the pin with gentle hammer blows. Observe the pin insertion process carefully as the pins might deform during insertion.
In case the pin head does not completely sink into the cartilage use a scalpel to remove the projecting part of the head.
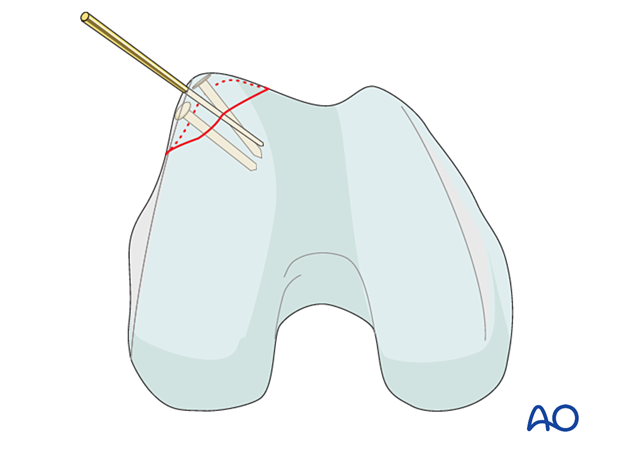
This illustration shows the completed osteosynthesis using absorbable pins.
6. Aftercare
Impediments to the restoration of full knee function after distal femoral fracture are fibrosis and adhesion of injured soft tissues around the metaphyseal fracture zone, joint capsular scarring, intra-articular adhesions, and muscle weakness.
Early range of motion helps restore movement in the early postoperative phase. With stable fracture fixation, the surgeon and the physical therapy staff will design an individual program of progressive rehabilitation for each patient.
The regimens suggested here are for guidance only and not to be regarded as prescriptive.
Functional treatment
Unless there are other injuries or complications, knee mobilization may be started immediately postoperatively. Both active and passive motion of the knee and hip can be initiated immediately postoperatively. Emphasis should be placed on progressive quadriceps strengthening and straight leg raises. Static cycling without load, as well as firm passive range of motion exercises of the knee, allow the patient to regain optimal range of motion.
Weight bearing
Touch-down weight-bearing (10-15 kg) may be performed immediately with crutches, or a walker. This will be continued for 6-10 weeks postoperatively. This is mostly to protect the articular component of the injury, rather than the shaft injury. Touch-down weight-bearing progresses to full weight-bearing gradually, over a period of 2 to 3 weeks (beginning at 6–10 weeks postoperatively). Ideally, patients are fully weight-bearing, without devices (e.g., cane) by 12 weeks.
Follow-up
Wound healing should be assessed at two to three weeks postoperatively. Subsequently 6-week, 12-week, 6-month, and 12-month follow-ups are usually made. Serial x-rays allow the surgeon to assess the healing of the fracture.
Thrombo-embolic prophylaxis
Thrombo-prophylaxis should be given according to local treatment guidelines.













