ORIF - blade plate
1. Principles
Introduction
The angled blade-plate devices are strong and can provide very stable fixation, even in a poor quality bone. Their correct insertion requires a high degree of surgical discipline and skill. A detailed preoperative plan and a step-by-step tactic are mandatory. Careful adherence to the exact conduct of each step of the procedure is essential for a satisfactory outcome.
The angle blade plate is versatile and can be applied in a bridging mode (wedge or multifragmentary supracondylar fracture component) and with compression (simple supracondylar fracture component).
Alignment of the main shaft fragments can then be achieved indirectly, using various aids before the application of the plate. Alternatively, the plate is applied to the articular block and then the plate is used as a reduction aid for the shaft.
Bridging mode
When used in bridging mode, the plate is an internal fixator used as an extramedullary splint, fixed to the two main fragments, leaving the intermediate fracture zone untouched. Anatomical reduction of intermediate fragments is neither sought nor necessary.
Direct manipulation of intermediate fragments would risk disturbing their blood supply. If the soft-tissue attachments to these fragments are preserved, and the fragments are generally aligned, healing is unimpaired.
Alignment of the main shaft fragments can be achieved indirectly with the use of:
- traction
- reduction tools
- the implant itself
Mechanical stability, provided by the blade plate, is adequate for gentle functional rehabilitation and results in satisfactory indirect healing (callus formation). Occasionally, a larger wedge fragment might be approximated to the main fragments with a lag screw.
Compression mode
This implant is particularly useful for obtaining metaphyseal compression. If a fracture pattern can be reduced to a "simple" metaphyseal fracture pattern (such as an intact wedge fracture where the wedge is fixed to the main fragment), then compression can be used for the metaphyseal "simple" fracture.
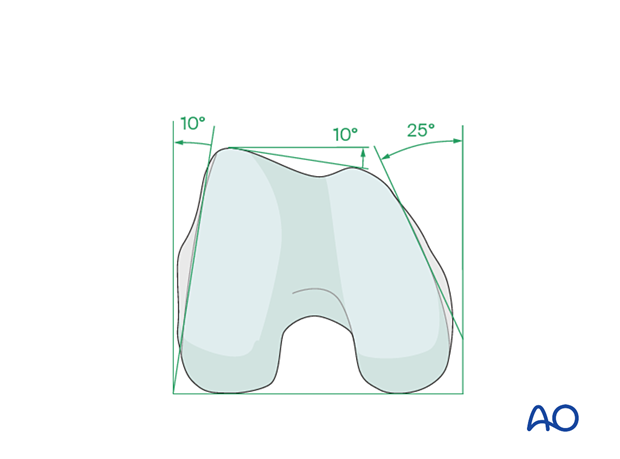
Anatomy of the distal femur
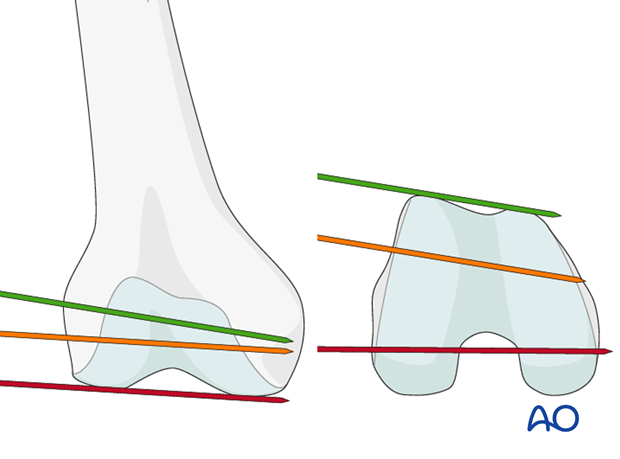
The distal femur has a unique anatomical shape. Seen from an end-on view, the lateral surface has a 10° inclination from the vertical, while the medial surface has a 20–25° slope.
A line is drawn from the anterior aspect of the lateral femoral condyle to the anterior aspect of the medial femoral condyle (patellofemoral inclination) that slopes approximately 10°. These anatomical details are important when inserting screws. In order to avoid joint penetration, these devices should be placed parallel to both the patellofemoral and femorotibial joints planes.
The muscle attachments to the distal femur are responsible for the typical displacement of the distal articular block following a supracondylar fracture, namely shortening with varus and extension deformity. Shortening is due to the pull of the quadriceps and hamstring muscles, while the varus and extension deformity is caused by the unopposed pull of the adductors and gastrocnemius, respectively.
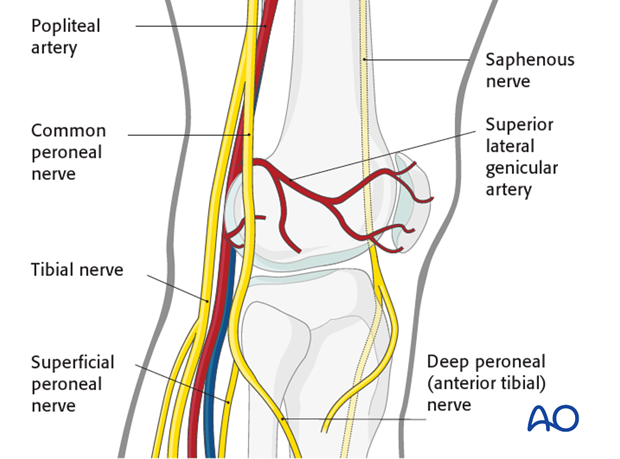
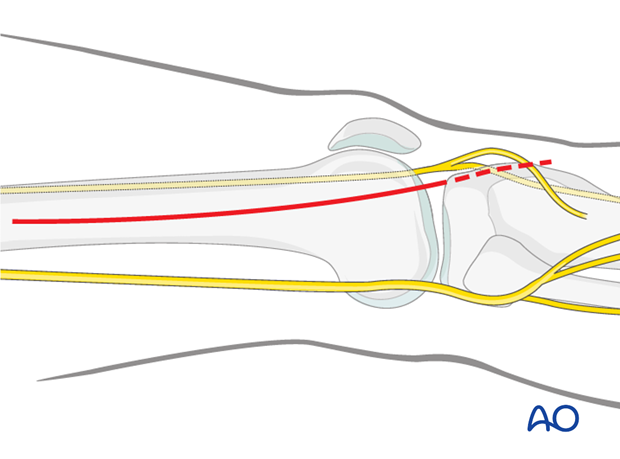
The popliteal vessels, the tibial nerve, and the common peroneal nerve lie near the posterior aspect of the distal femur. Because of this, vascular injuries occur in about 3% and nerve injuries in about 1% of fractures of the distal femur.
There are no significant arteries, veins, or nerves on the lateral side of the knee.
There may be bleeding from the lateral genicular arteries, which will need to be controlled using diathermy.
At the posterior aspect of the knee lie the popliteal artery, nerve, and vein. It must be borne in mind that these structures can be damaged by the injury or can be damaged by the surgeon during the reconstruction.
Teaching videos
The blade plateAO Teaching video about the blade plate on the distal femur.
AO Teaching video about condylar blade fixation.
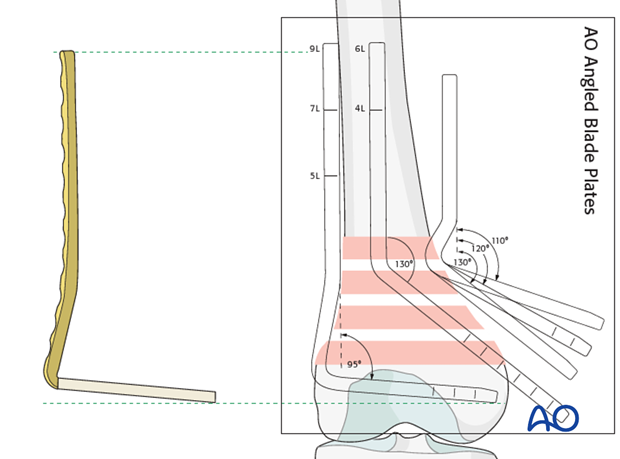
2. Plate length determination
Determine the plate length by measuring from the template.
It should be remembered that the medial aspect of the femur is angled 20°-25° inwards and 15 mm should be subtracted from the apparent length to ensure that the blade does not perforate the medial aspect of the femur.
Conventional templating has in the past been performed with plain x-rays. 3D-CT reconstructions are currently the most accurate representation of the fracture.
3. Patient preparation and approach
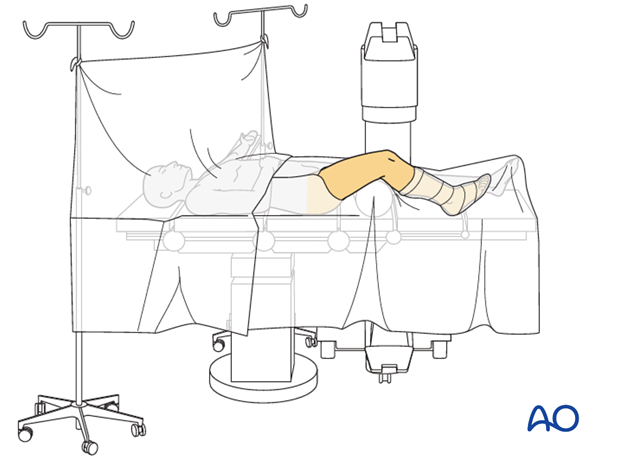
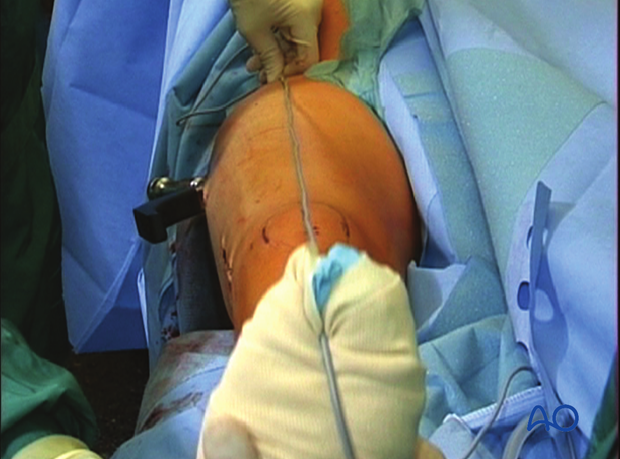
Positioning
This procedure may be performed with the patient in one of the following positions:
- Supine position knee flexed 30°
- Supine position knee flexed 90°
- Lateral decubitus (particularly in obese patients)
Approach
For this procedure, the lateral/anterolateral approach is used.
4. Reconstruction of the articular block
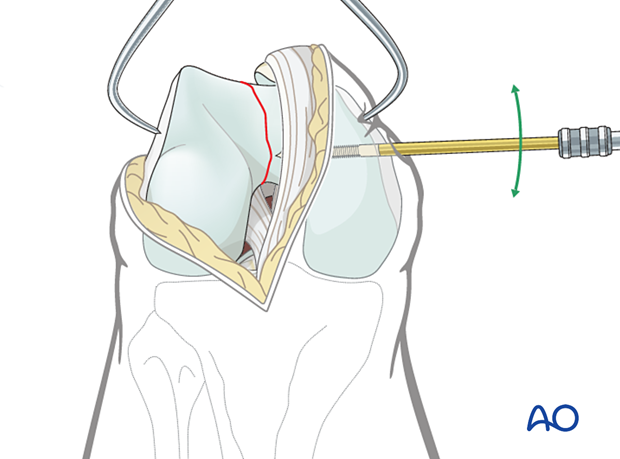
Reduction of the articular block
The approach must adequately expose the articular surface of the distal femoral condyle. Reduction aids that are helpful include:
- A 5.0 mm or 6.0 mm Schanz pin in the medial and/or lateral femoral condyle to act as a joystick.
- Pointed reduction forceps, or large pelvic reduction clamps, to clamp from medial to lateral across the intercondylar split.
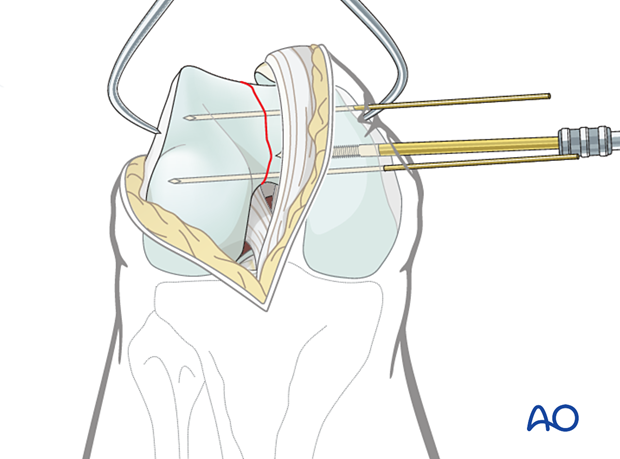
Provisional fixation
Before definitive fixation is undertaken, more than one foreceps is applied. Usually, one to two additional K-wires are inserted, either from medial to lateral, or lateral to medial.
If the K-wires are inserted from medial to lateral, they may either go through small stab incisions in the skin or through the parapatellar retinaculum.
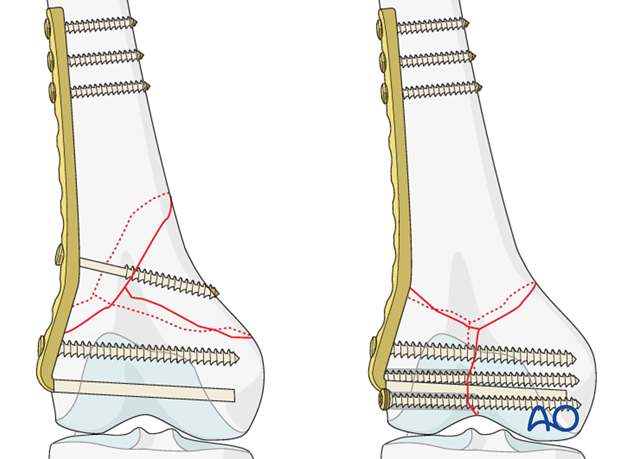
Definitive articular surface fixation
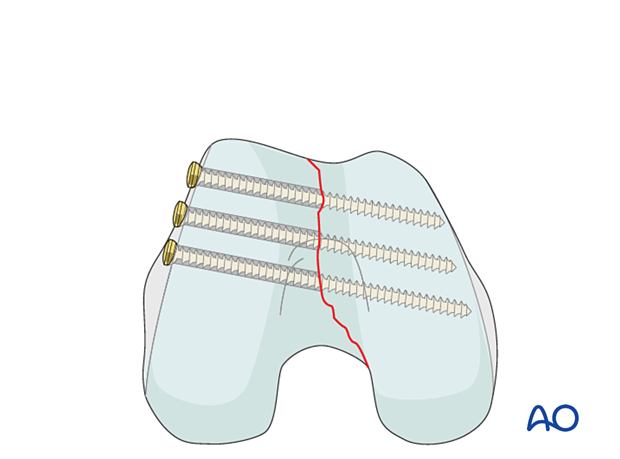
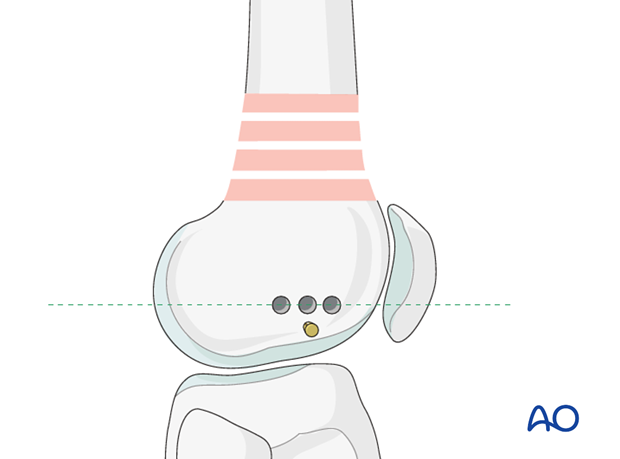
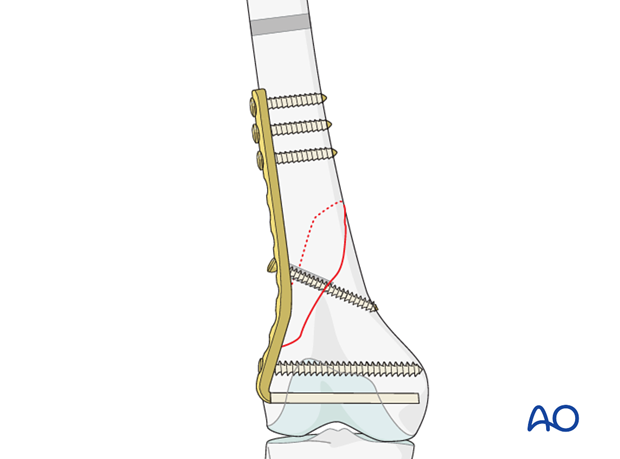
Screws are inserted along the periphery of the articular surface of the lateral femoral condyle going from lateral to medial or from medial to lateral to compress the intercondylar split.
These screws may be fully threaded 2.7 or 3.5 mm lag screws (shown with gliding hole), 6.5mm partially threaded lag screws, or 4.0/4.5 mm cannulated, partially threaded lag screws.
Insertion of screws in this manner leaves an area free of screw traffic or a "free-zone" of bone into which a laterally based plate system can be inserted (dotted circle).
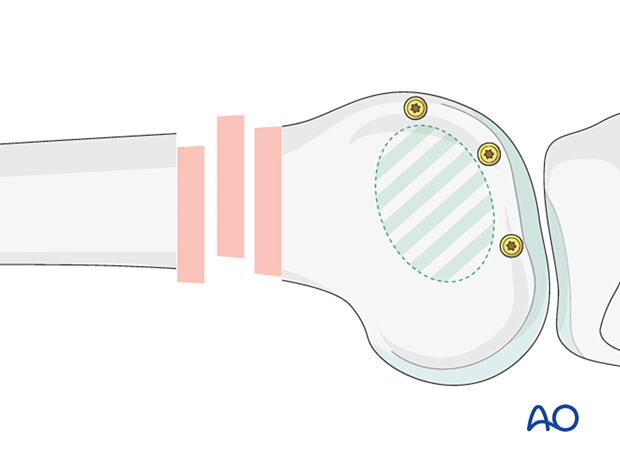
This end-on view demonstrates the screw trajectories from lateral to medial.
On occasions, it is acceptable to insert screws through the articular surface, when no other option is available. These screws must be countersunk and recessed beneath the articular surface.
5. Reduction
Reduction techniques
Depending on the fracture morphology, there are two basic methods to reduce the metaphysis/diaphysis when utilizing a blade plate.
In a single plane short spiral or oblique fracture, the direct reduction is performed followed by plate application.
Direct reduction instruments include:
- Large pointed reduction forceps
- Bone repositioning forceps
- Bone hook

In a single plane short spiral or oblique fracture, the direct reduction is performed followed by plate application.
Direct reduction instruments include:
- Large pointed reduction forceps
- Bone repositioning forceps
- Bone hook
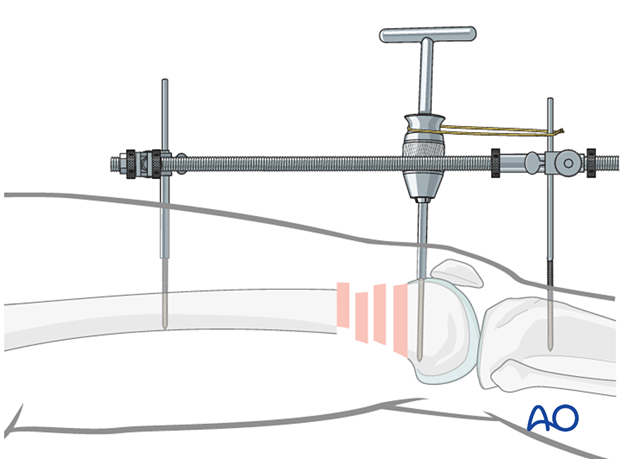
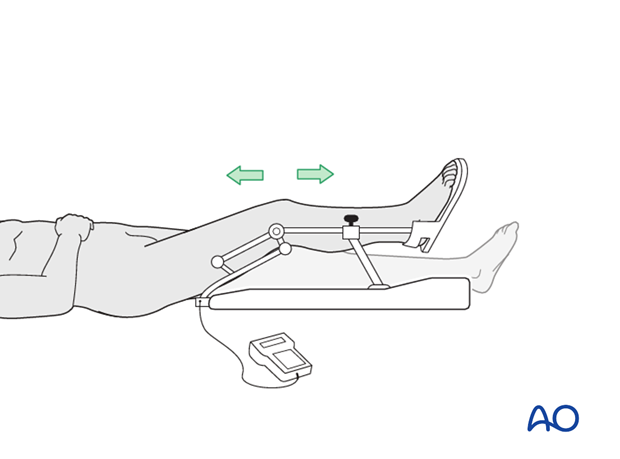
In fragmented metaphyseal/diaphyseal fractures, the blade plate is first inserted into the correct position in the distal articular block of the femur. Then, after manual traction is used to restore the appropriate length and rotation, the bone is drawn down to the plate and the proximal screws are inserted. This type of reduction is very helpful in multifragmentary metaphyseal/diaphyseal fractures.
Indirect reduction techniques are:
- Manual traction
- External fixator/distractor (illustrated)
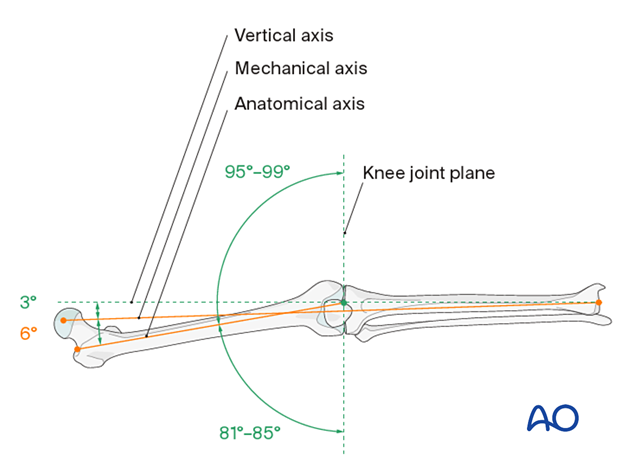
Verification of successful reduction
It is very important to restore the biomechanical axis of the lower limb. The normal biomechanical axis follows a line from the center of the femoral head, through the center of the proximal tibia and then through the center of the ankle joint. This axis can be checked intraoperatively by using a piece of cable, such as the diathermy cord. The cord is stretched from the iliac spine across the patella to the cleft between the first and second toes.
If rotation is correct, this cord will pass over the midline of the patella, and slightly medial to the tibial eminence. The radiological landmarks of the center of the femoral head, the center of the knee and the center of the ankle joint should all be in line if the mechanical axis of the femur is correct.
Another method of assessing rotational reduction is to compare the cortical thickness above and below the fracture. If a shaft fracture is multifragmentary, the image intensifier cannot be used to compare cortical diameters on each side of the fracture.
Not only must the biomechanical axis be restored, but care should be taken to ensure that there is no malrotation of the distal femur on the proximal femur.
This illustration shows the longitudinal axes of the lower limb.
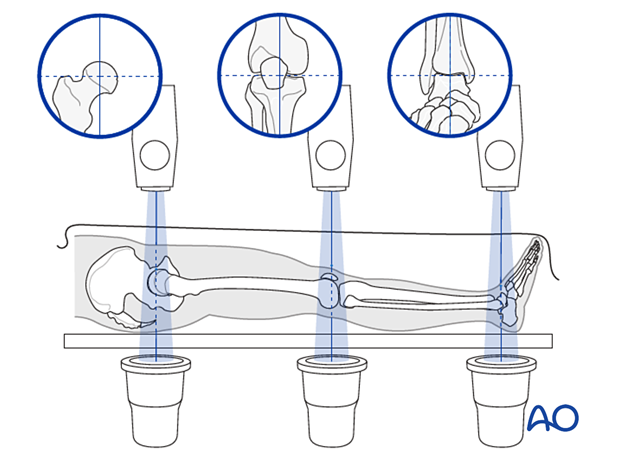
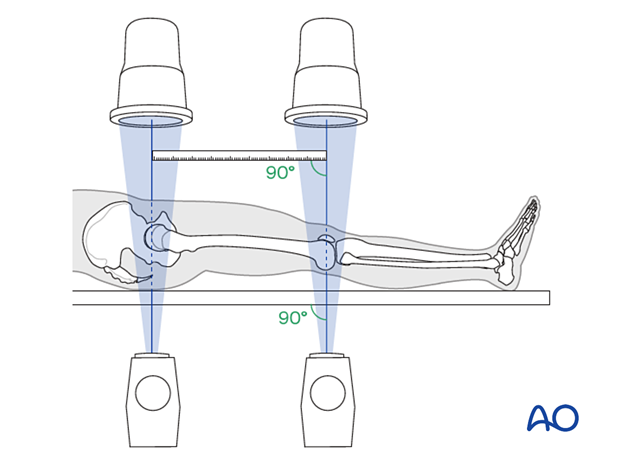
Confirmation of length
To ensure that femoral length has been restored, many options exist:
- One option involves reducing the fracture fragments anatomically, either directly or indirectly with fluoroscopic control.
- Even in multifragmentary fractures, there are usually a few main fracture segments that can assist the surgeon in ensuring that the appropriate length has been obtained.
- Another option involves taking radiographic images of the contralateral distal femur for comparison.
- A radiographic ruler can be used to measure the length of both femora. In this technique, it is important that the x-ray beams are perpendicular to the OR table and that the ruler is parallel to the OR table.
6. Planning of plate insertion
Correct blade trajectory
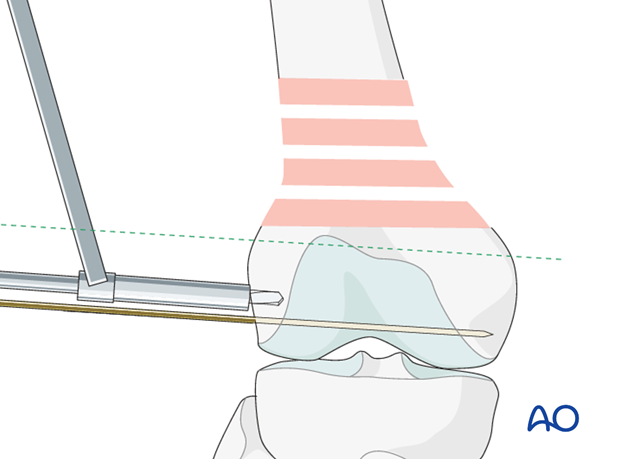
Determine the correct blade plate trajectory with the help of guide wires around the joint.
Under image intensifier control, pass one guidewire lateral to medial along the tibiofemoral joint line (red).
Pass a second guidewire over the anterior surface of the femur to indicate the plane of the patellofemoral joint (green).
The ideal position of the blade plate is shown by the yellow wire. Note that this is parallel to the red wire in the frontal plane (and thus leads to the appropriate varus/valgus) and is parallel to the green line on the end-on view on the femur. This latter parameter ensures that the plate is flush with the lateral cortex.
Correct blade insertion point
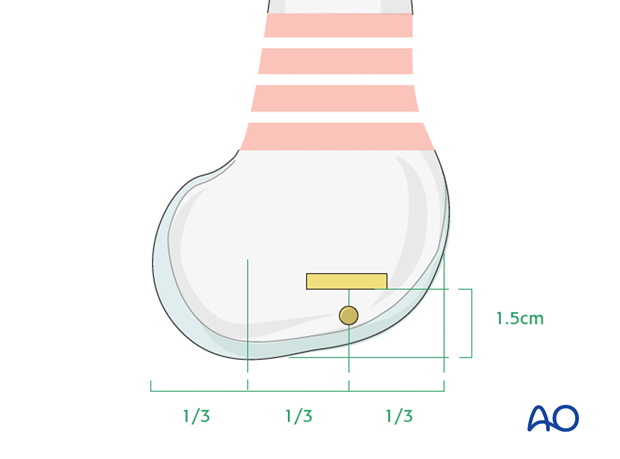
The ideal insertion point for the blade plate is crucial and shown in the diagram.
The blade enters 1.5 cm above the distal end of the femur.
To locate the correct anterior/posterior entry point, divided the distal femur into thirds. The center of the blade plate entry site is at the junction of the anterior one third and middle one third.
Insert the third guide wire just distal to the intended place of plate insertion. This guide wire is parallel to the distal femoral articular surface in the frontal plane, is perpendicular to the lateral femoral cortex, and parallel to the plane of the patellofemoral joint.
7. Preparing the channel
Cutting the channel
To prepare for opening the entry site for the blade, three 4.5 mm holes are drilled in the lateral cortex of the femoral condyle. They only need to penetrate 1 cm, except in young, harder bone, when the surgeon may need to drill almost the full depth of the chosen blade length. A hole is drilled at the center of the slot to be prepared. Two additional holes are drilled on either side of the central hole.
A triple drill guide is available, but this has been designed for the proximal femur and use with 130° angled blade plates: this makes it a little cumbersome at the distal femur.
It is easier to drill the holes freehand, using the 4.5 mm single drill sleeve, in an anteroposterior configuration. Drill them as parallel to the third guidewire as possible.
Connect the drill holes with a router
Take care not to damage or displace the guidewire. Then connect the drill holes with a router.
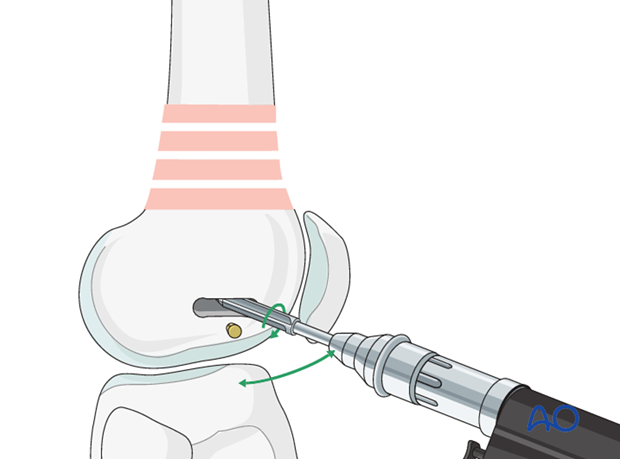
Round the proximal shoulder of the slot off with a chisel to enable the plate to be seated fully on the bone.
It may be necessary to use the 4.5 mm drill to deepen the channel into the femoral condyles in the correct planes.
The seating chisel is meant to be driven exactly parallel to the guidewire in both planes. The seating chisel is hammered into the distal femur with a mallet. Particularly in the young, the seating chisel is “back-slapped” using the slotted hammer. For each 15 mm of insertion, this back-slapping should be performed. Otherwise, the seating chisel will become jammed in the bone. Repeatedly check parallelism with the guidewire.
In hard bone, it may become necessary to pre-drill the seating chisel track, but this requires great care to keep the 4.5 mm drill bit exactly parallel to the guidewire.
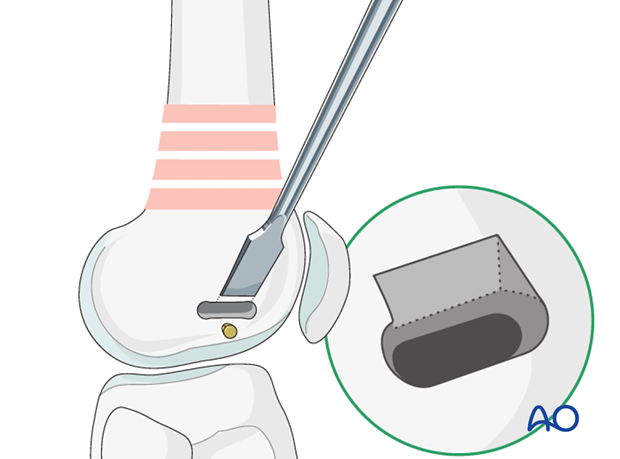
Seating chisel insertion
Insert the seating chisel through its guide into the distal femur. Use the slotted hammer to control the rotation of the seating chisel in the bone, so that the tongue of the guide lies in the anatomical long axis of the shaft.
An assistant may need to apply counter pressure on the medial side of the femur, especially if preliminary lag screw fixation of an intercondylar split has been performed.

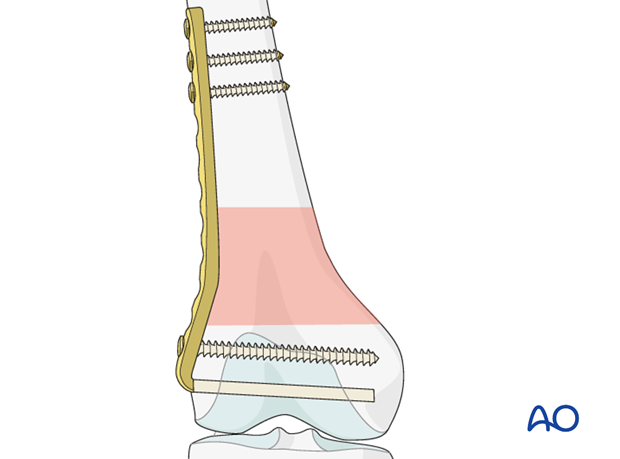
8. Plate insertion
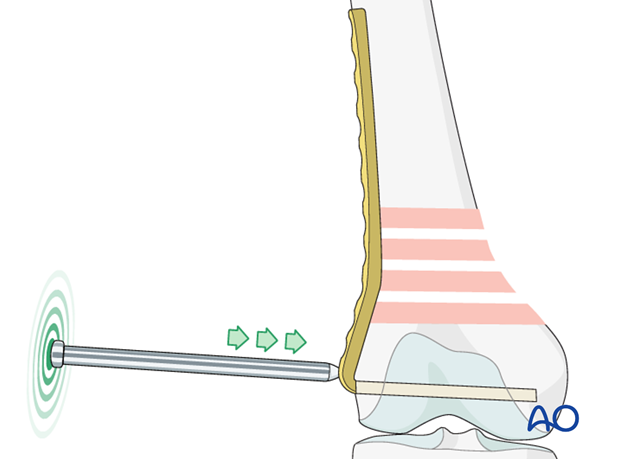
Plate insertion
Insert the blade plate using the blade plate insertion device, fitted so that the shaft of the device is parallel with the blade.
The blade should follow the path of the seating chisel precisely and remain parallel with the guidewire. The first half of the blade plate should be able to be pushed manually into the bone along the previous path of the seating chisel. If this is not possible the surgeon should question whether a false path is being developed. Frequent checks under fluoroscopy will ensure the proper path of the blade plate.
Take care to control the alignment of the blade plate to the longitudinal axis of the femur.
Maintain counter pressure on the medial side of the distal femur while inserting the plate.
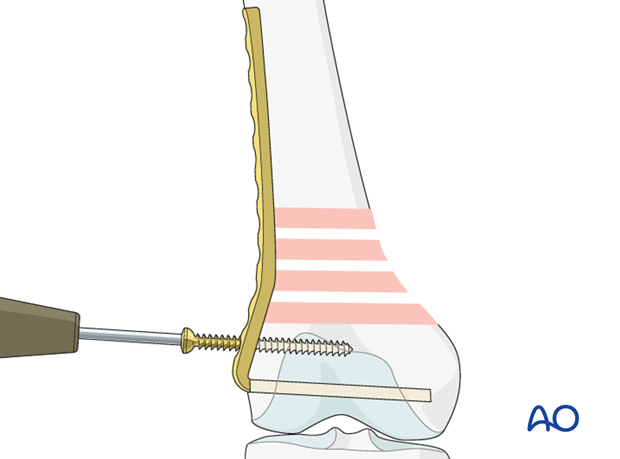
Impaction of plate to the bone
As the plate comes to within 1.5 cm of the lateral femoral cortex, the blade plate insertion device is removed. At this point, the final insertion of the blade is performed using the impactor.
Securing the plate to the distal femur
At least one additional screw is inserted into the distal femoral articular block. This provides sagittal plane stability.
9. Final reduction and fixation
Final reduction of metaphyseal component
The key concept in the reduction of the metaphyseal component of the fracture, when using a blade plate, is that correct insertion of the blade into the distal femur allows the surgeon to use the plate to achieve the metaphyseal fracture reduction.
When brought down to the lateral cortex of the femoral shaft the correct frontal plane alignment has been assured. The surgeon must then control for length and rotation.
Length can be aided by manual traction.
The sagittal plane deformity correction is determined by rotational control, using the slotted hammer, during seating chisel insertion. Small corrections of extension/flexion deformity can be achieved by moving the proximal end of the plate forward or backward on the lateral femoral cortex, but there is little room for maneuver.
Take care to restore the mechanical axis in all planes of the femur. Give consideration to fracture reduction in:
- Varus/valgus
- Flexion/extension
- Internal/external rotation
- Translation
- Lengthening/shortening
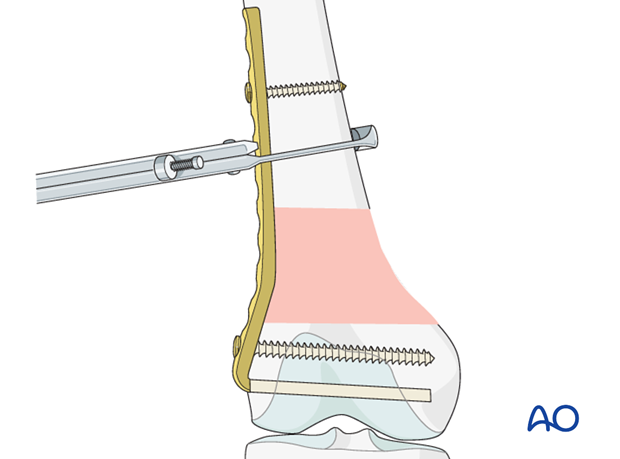
Secure the plate to the proximal femur with a bone holding forceps (Verbrugge forceps).
Compression vs bridging
Fixation with compression should be applied when possible in fracture patterns where there is contact between the proximal and distal main fragments.
It may not be used in situations of multifragmentary
fractures and/or osteoporosis. I these fractures, bridging mode is used.
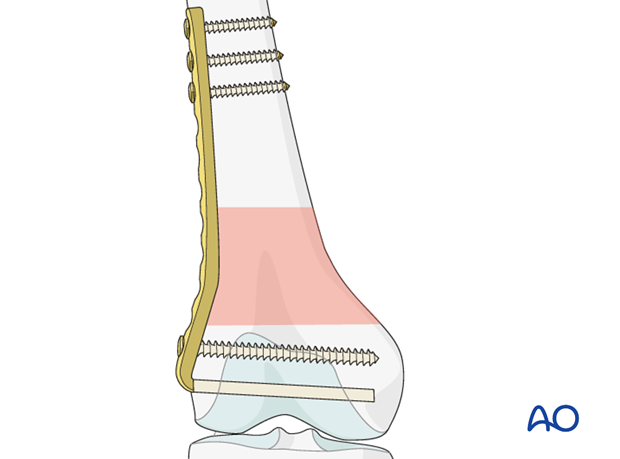
Fixation in bridging mode
Once adequate alignment is achieved, fix the plate to the proximal femur with at least 4 bicortical standard 4.5 mm screws.
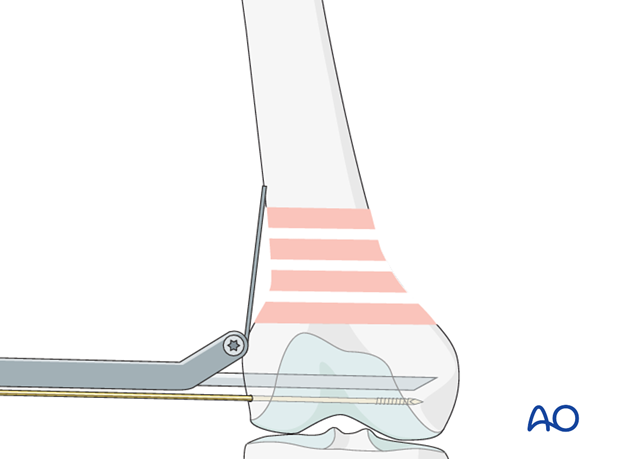
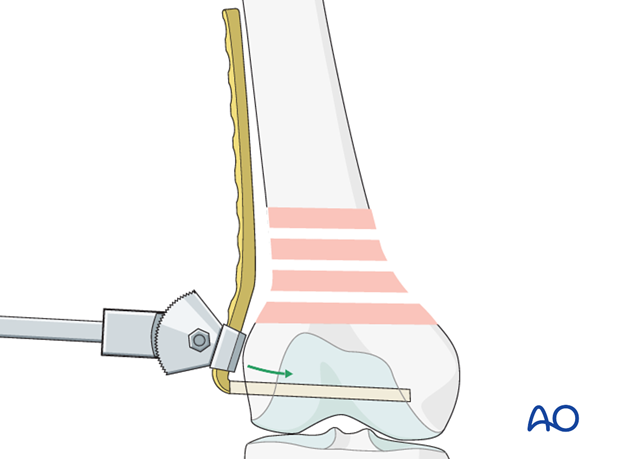
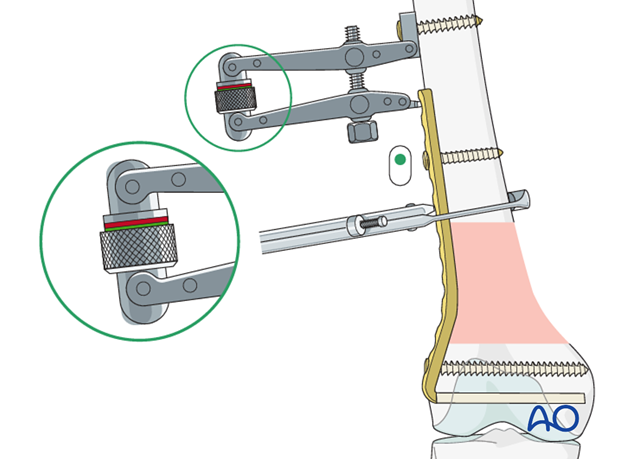
Fixation with compression
Secure the articulated tension device to the proximal femur with a bicortical screw. Tighten the articulated tension device with the spanner so that the indicator on the tension device is in the green zone, checking the fracture site carefully to ensure that no unwanted displacement occurs.
Insert a screw through the plate close to the compression device to secure the fixation. Insert the screw eccentrically in the plate hole to maintain the fracture compression.
Complete the fixation of the plate to the femur with sufficient screws, using neutral insertion of the screws in the plate holes.
Lastly, remove the articulated tension device and complete the fixation by inserting additional screws according to the preoperative plan.
In oblique, single-plane fractures, an interfragmentary lag screw should be inserted through the plate.
10. Wound closure, assessment of alignment and knee stability
Wound closure
End the procedure with the closure of the deep tissues and the skin.
Assessment of alignment and knee stability
Before the patient is moved from the fracture table, observe rotation of the leg clinically and compare it to the contralateral side.
With the femur now stable, it is possible to perform a thorough examination of the knee joint, in order to exclude associated ligamentous laxity.

11. Aftercare
Impediments to the restoration of full knee function after distal femoral fracture are fibrosis and adhesion of injured soft tissues around the metaphyseal fracture zone, joint capsular scarring, intra-articular adhesions, and muscle weakness.
Early range of motion helps restore movement in the early postoperative phase. With stable fracture fixation, the surgeon and the physical therapy staff will design an individual program of progressive rehabilitation for each patient.
The regimens suggested here are for guidance only and not to be regarded as prescriptive.
Functional treatment
Unless there are other injuries or complications, knee mobilization may be started immediately postoperatively. Both active and passive motion of the knee and hip can be initiated immediately postoperatively. Emphasis should be placed on progressive quadriceps strengthening and straight leg raises. Static cycling without load, as well as firm passive range of motion exercises of the knee, allow the patient to regain optimal range of motion.
Weight bearing
Touch-down weight-bearing (10-15 kg) may be performed immediately with crutches, or a walker. This will be continued for 6-10 weeks postoperatively. This is mostly to protect the articular component of the injury, rather than the shaft injury. Touch-down weight-bearing progresses to full weight-bearing gradually, over a period of 2 to 3 weeks (beginning at 6–10 weeks postoperatively). Ideally, patients are fully weight-bearing, without devices (e.g., cane) by 12 weeks.
Follow-up
Wound healing should be assessed at two to three weeks postoperatively. Subsequently 6-week, 12-week, 6-month, and 12-month follow-ups are usually made. Serial x-rays allow the surgeon to assess the healing of the fracture.
Implant removal
Implant removal is not essential but should be discussed with the patient if there are implant-related symptoms after consolidated fracture healing.
Thrombo-embolic prophylaxis
Thrombo-prophylaxis should be given according to local treatment guidelines.













