Open reduction - Ligament repair
1. General considerations
As the injury will be unstable after closed reduction, the goal of the treatment is stabilization by open reduction and ligament repair with K-wire fixation.
Sometimes, combined surgical approaches facilitate comprehensive repair of the multiple ligament disruptions.
The scapholunate and lunotriquetral ligaments are repaired, eg, with suture anchors and temporary K-wire joint transfixation.
Concomitant fracture of the distal radius, eg, radial styloid fracture, should be treated simultaneously.
2. Preliminary treatment
Closed reduction of the lunate
Closed reduction is preliminary to operative treatment and has the following benefits:
- Reducing the risk of median nerve injury
- Restoration of carpal alignment
- Pain relief
- Facilitating surgical repair
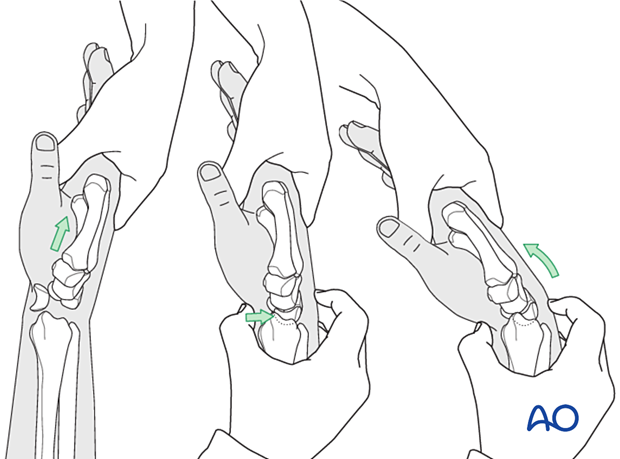
The displaced lunate is reduced by distracting and slightly extending the wrist and then applying direct thumb pressure over the lunate from palmar to dorsal.
The wrist is then flexed slightly. The reduction is felt as the lunate relocates. The distraction is then released.
Confirm the lunate relocation with an image intensifier.
If closed reduction is not successful, open reduction via a palmar approach is necessary as soon as possible (due to the risk of median nerve injury).
Splint immobilization
After emergency reduction, the wrist is immobilized in a palmar plaster splint in the neutral position.
3. Patient preparation
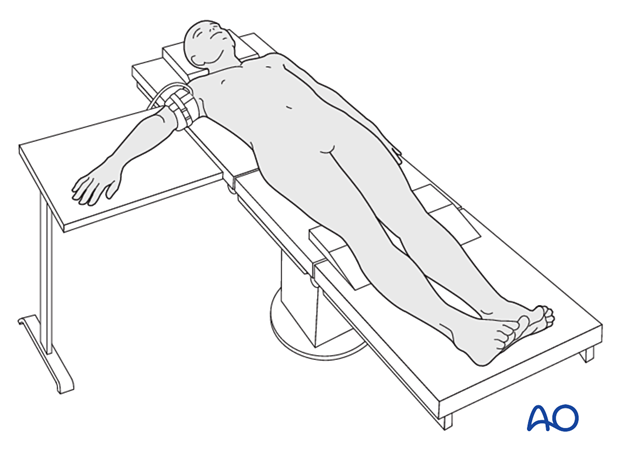
The patient is usually supine with the arm on a radiolucent side table.
4. Approaches
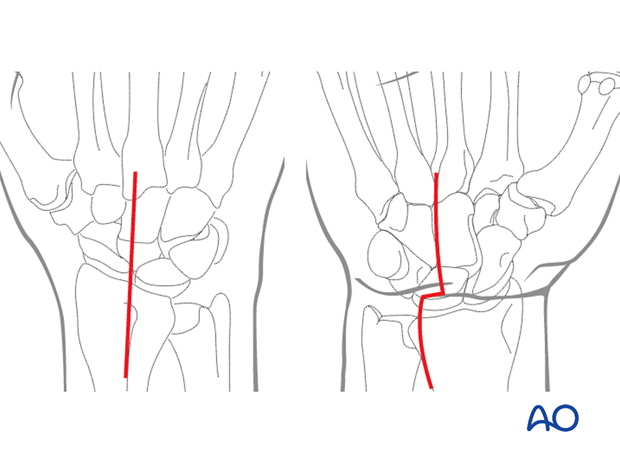
For this procedure, a dorsal approach may be used.
If the reduction is not anatomical or the median nerve needs to be explored (carpal tunnel decompression), a combination with a palmar approach is necessary.
5. Open reduction
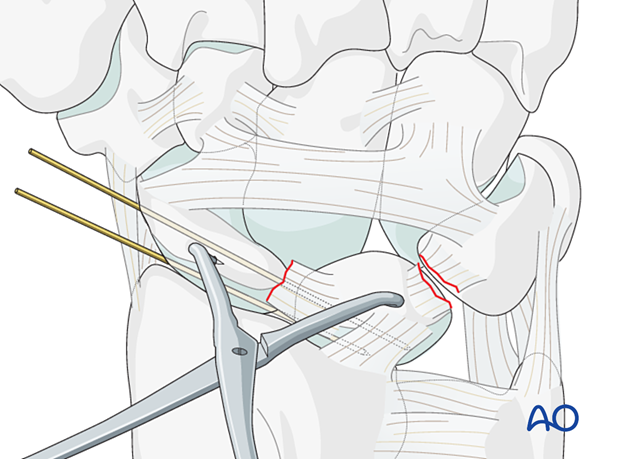
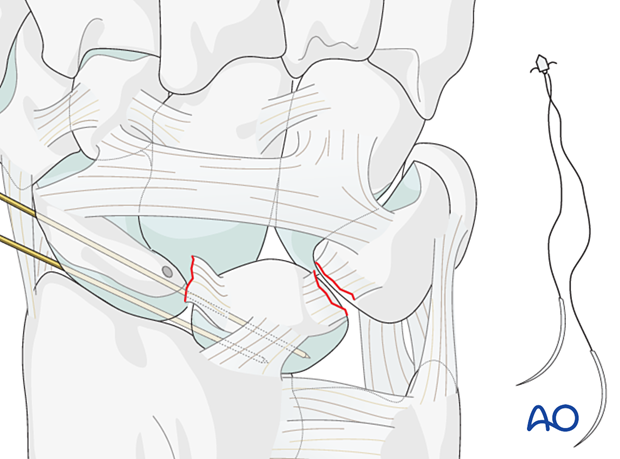
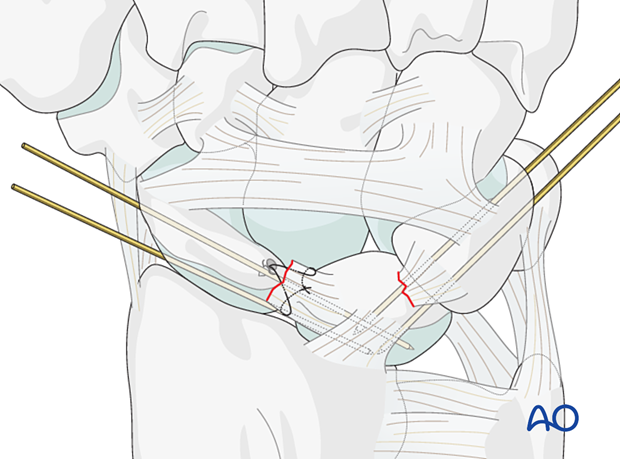
At the subsequent surgery, insert a joystick K-wire into both the scaphoid and the lunate.
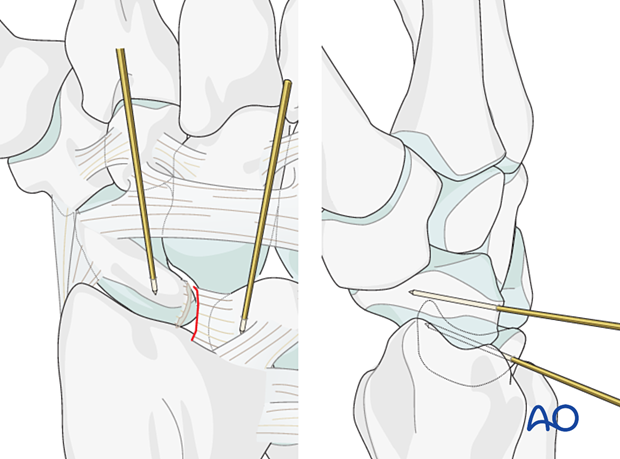
To reduce the scapholunate joint, extend the scaphoid, flex the lunate, and then close the gap.
Use pointed reduction forceps to hold the reduction.
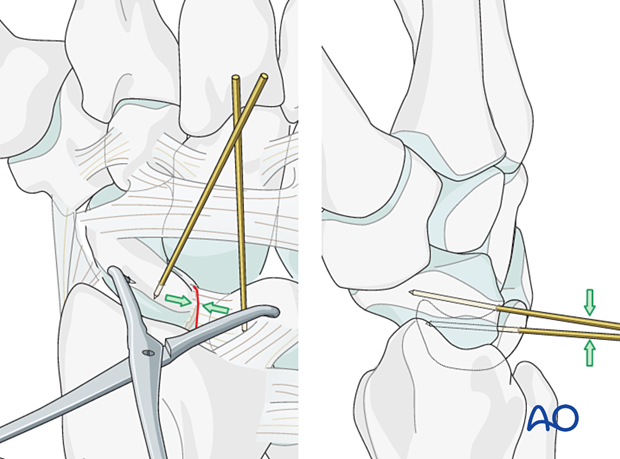
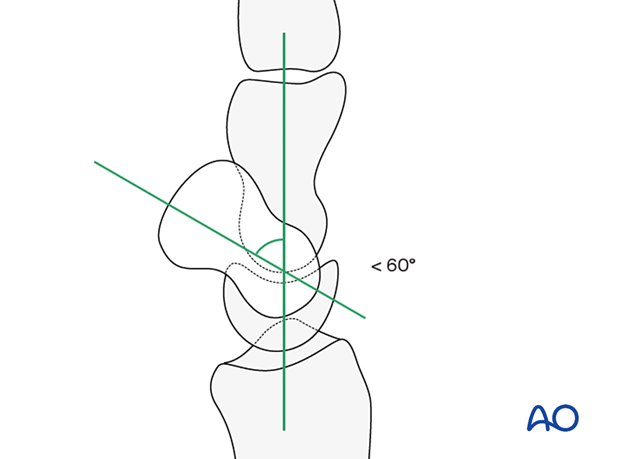
Check the correct scaphoid and lunate alignment on a lateral view. The lunate should be in neutral position. The angle between the long axes of the scaphoid and lunate should be less than 60°.
6. Transfixation of the scapholunate joint
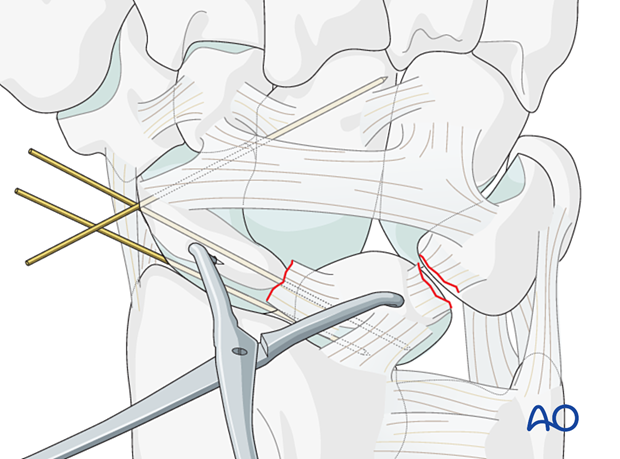
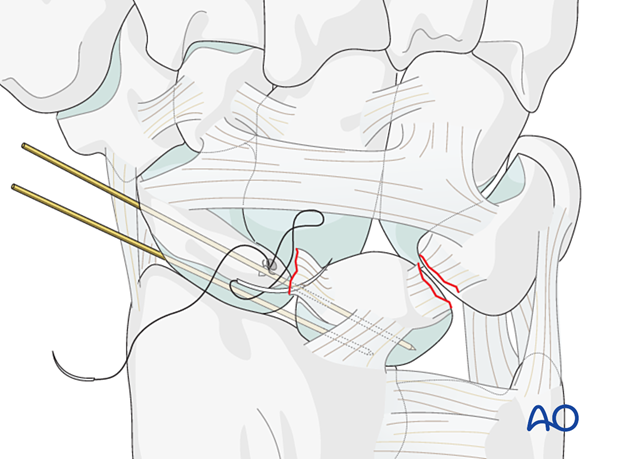
Under image intensification, advance two K-wires percutaneously from the scaphoid into the lunate.
Option: transfixation of the scaphocapitate joint
The stability of the wrist can be enhanced by inserting a K-wire from the scaphoid into the capitate.
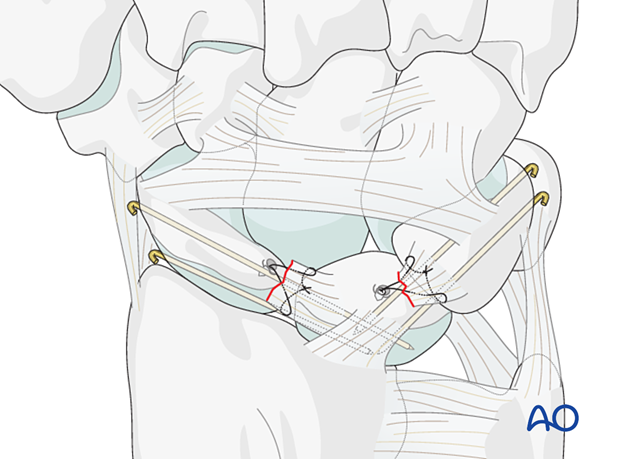
7. Scapholunate ligament repair
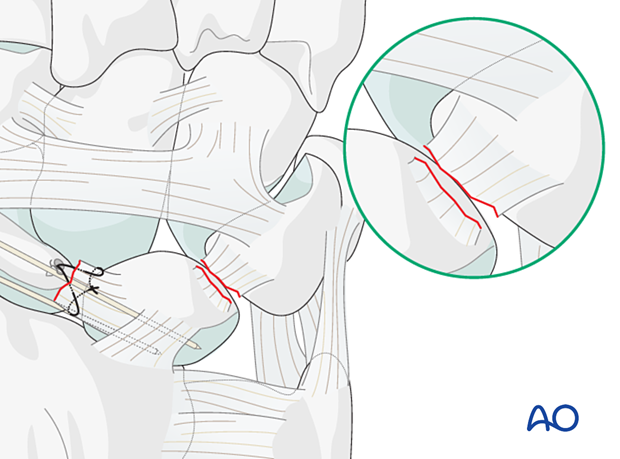
Assessment of dorsal and proximal ligament remnants
In most cases, the scapholunate ligament is avulsed from the scaphoid and remains attached to the lunate.
Freshen the avulsion site to improve contact and healing.
Insertion of a suture anchor
Insert the bone anchor dorsally into the debrided area of the scaphoid (or in the lunate if the ligament is avulsed from that bone).
The entry point for the anchor must be placed in such a position that the line of pull of the suture is slightly oblique to resist rotational forces between both bones.
Often, one anchor will be sufficient, but occasionally two anchors will be needed.
Insert the anchor suture into the torn end of the ligament and tie the anchor sutures in the ligament.
Direct suture fixation
If there is a mid-substance tear of the ligament, suture it directly.
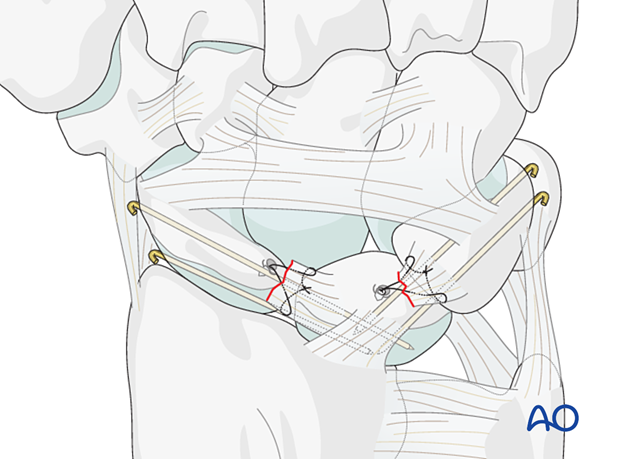
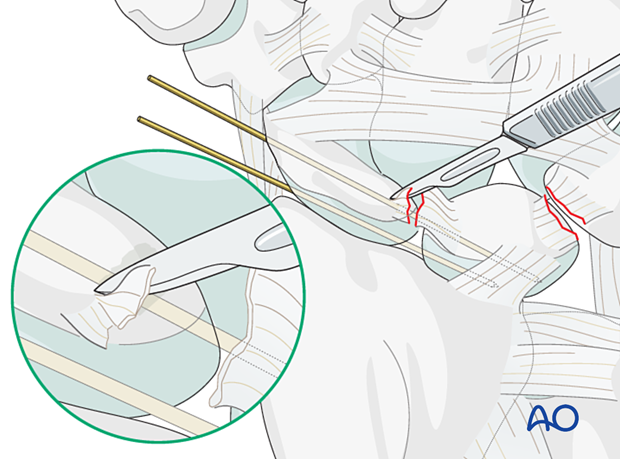
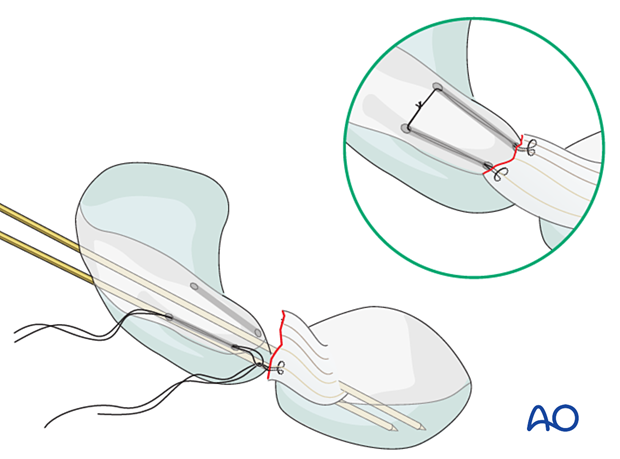
Option: transosseous ligament refixation
If bone anchors are unavailable, attach the avulsed ligament with sutures passed through small tunnels drilled into the proximal pole of the scaphoid, as illustrated.
There is a risk of cortical fracture of the scaphoid, which makes the treatment complicated.
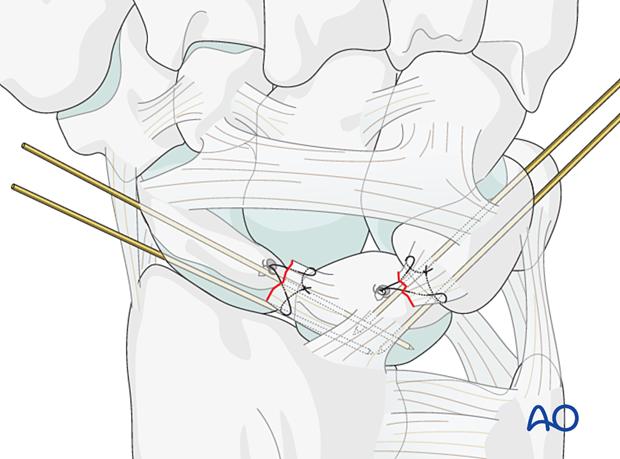
8. Lunotriquetral ligament repair
Principles
In most cases, the lunotriquetral ligament is torn from the lunate.
Usually, reduction and temporary fixation of the lunotriquetral relationship is all that is possible from the dorsal aspect.
K-wire transfixation
Reduce the lunotriquetral relationship and insert two 1.4 mm K-wires percutaneously from the triquetrum into the lunate.
Confirm the reduction using image intensification.
Ligament repair
If there is sufficient ligament remnant, repair with a bone anchor is possible. Insert a suture anchor into the debrided area of the avulsion.
If there is a larger bony avulsion of the lunotriquetral ligament from either bone, the fragment can be fixed with fine K-wires or a small screw.
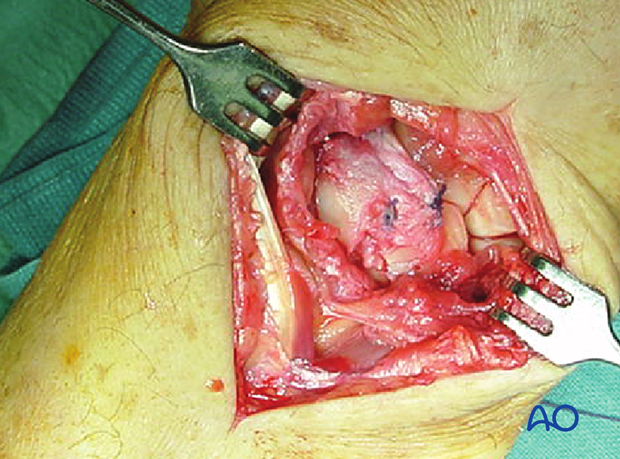
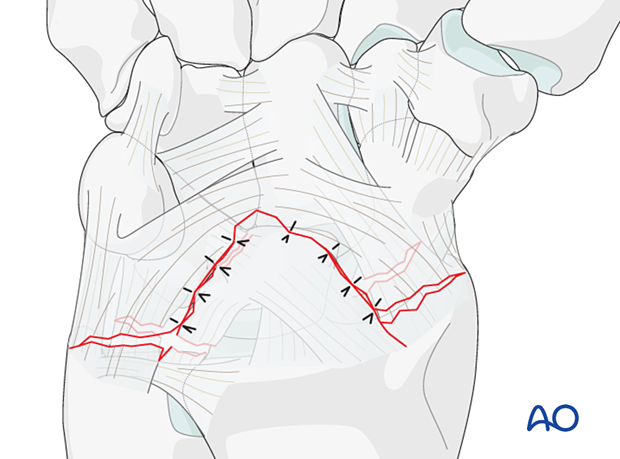
9. Revision through a palmar approach
If a palmar approach has been used for reduction or median nerve exploration, the soft-tissue tears may also be repaired.
A palmar approach demonstrates characteristic disruptions of the extrinsic palmar ligaments, which start in the space of Poirier and expose the midcarpal joint.
10. Final check
After final confirmation of accuracy of realignment, using image intensification, cut and bend over the K-wires, so they do not protrude through the skin.
11. Aftercare
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.
Pain control
To facilitate rehabilitation, it is important to control the postoperative pain adequately. To do so, the following should be considered:
- Management of swelling
- Appropriate splintage
- Appropriate oral analgesia
- Careful consideration of peripheral nerve blockade
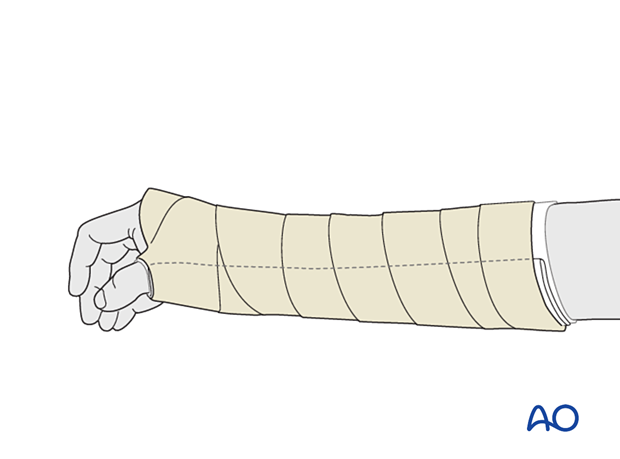
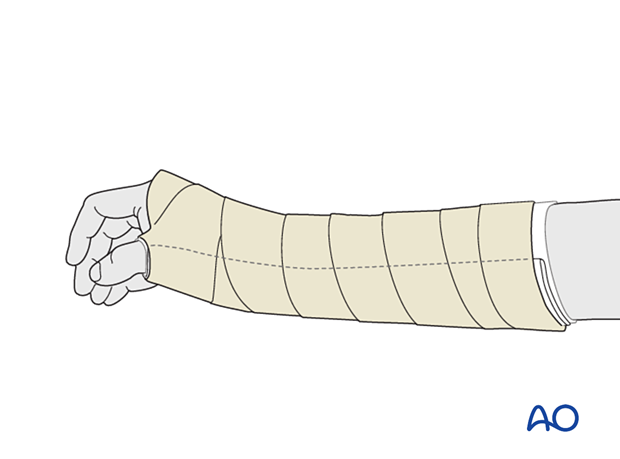
Immediate postoperative treatment
Immobilize the wrist with a well-padded below-elbow splint for 2 weeks.
Splinting helps with soft-tissue healing, especially of the ligaments cut during a palmar approach.
Follow-up
After 2 weeks, remove the sutures, check the skin over the K-wires, and apply a below-elbow scaphoid cast with slight dorsiflexion at the wrist for 6–8 weeks. Then the K-wires are also removed with appropriate pain control.
Check the skin regularly every 2 weeks in the outpatient clinic.