ORIF
1. General considerations
Dislocation of the carpometacarpal (CMC) joint, especially with the 4th and 5th, may be associated with a coronal fracture of the hamate, which also needs reduction to achieve joint stability. If the 3rd CMC joint is involved too, then usually the capitate is also fractured.
If the coronal fragment can be reduced anatomically with joint congruity, there is often no need for fixation of the fracture. If reduction is not successful (without congruity), an open reduction and screw or K-wire fixation is necessary. This is also recommended in noncompliant patients.
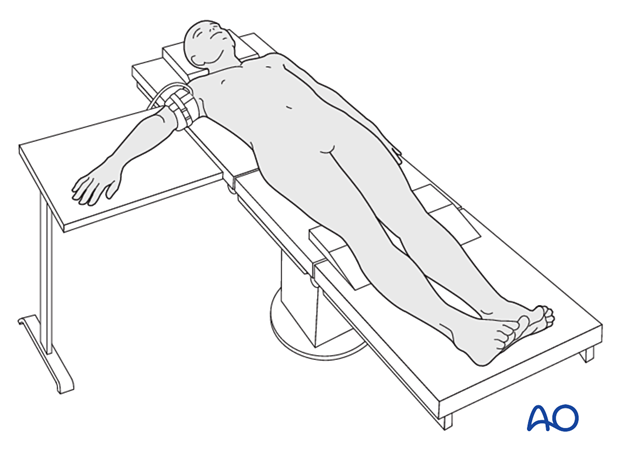
2. Patient preparation
The patient is usually supine with the arm on a radiolucent side table.
Local or regional anesthesia may be applied.
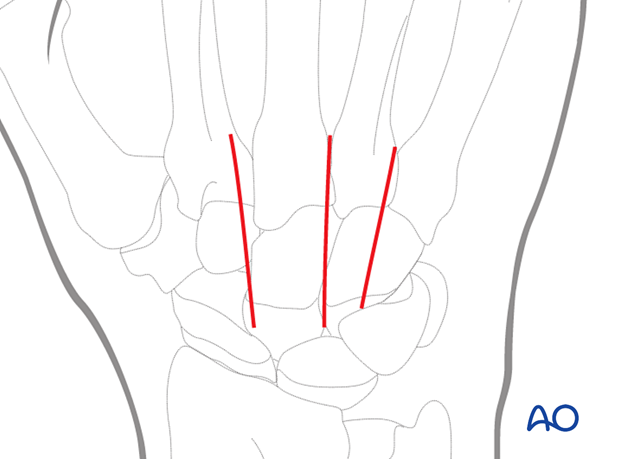
3. Approach
A dorsal approach to the affected CMC joints may be used.
Protect the dorsal sensory nerve branches (radial and ulnar).
4. Reduction
Closed reduction
Dislocation is usually dorsally and may be reduced manually in a closed manner.
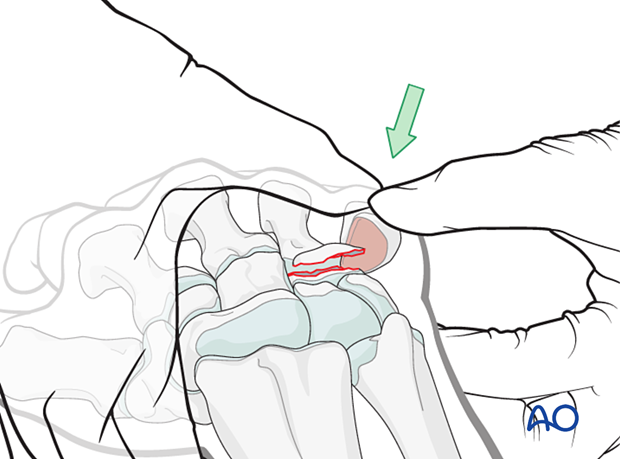
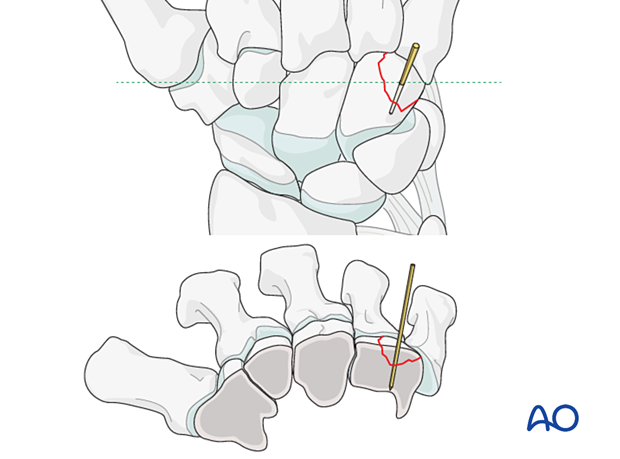
The coronal fragment of the hamate is displaced with the dorsally dislocated 4th and/or 5th metacarpal base. Manual reduction of the dislocation may also reduce the fracture.
Stability evaluation
Confirm reduction with an image intensifier and check the joint stability by passive flexion and extension of the fingers.
Open reduction
If the joint is unstable or reduction is unsuccessful, proceed with open reduction.
Often, the joint capsules are ruptured, and the joint space is easily exposed.
Remove any soft tissue or bony fragments and reduce the joint.
5. Fixation of the hamate fracture
According to the size of the coronal hamate fragment, fixation with a miniscrew is recommended:
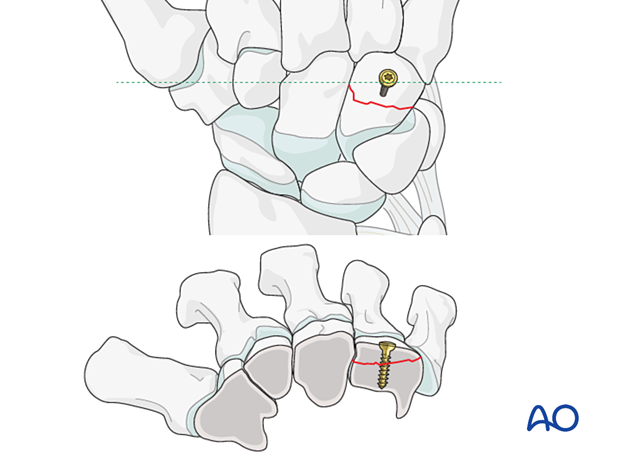
If a screw is unavailable or the fragment is small, a K-wire can be used instead.
6. Joint stabilization with temporary K-wire
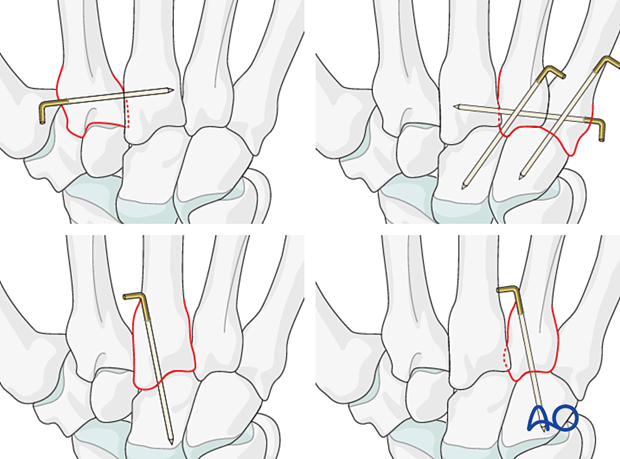
Often there is persistent instability, eg, subluxation or redislocation during the range of motion. In this case, add a temporary K-wire:
- Transverse fixation of the affected metacarpal base to an uncompromised neighboring metacarpal base
- Retrograde transfixation through the metacarpal base into the carpal bones
Repair the capsule.
Bend the end of the K-wire above the skin and cut it with enough length to avoid migration.
7. Aftercare
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.
Pain control
To facilitate rehabilitation, it is important to control the postoperative pain adequately.
- Management of swelling
- Appropriate splintage
- Appropriate oral analgesia
- Careful consideration of peripheral nerve blockade
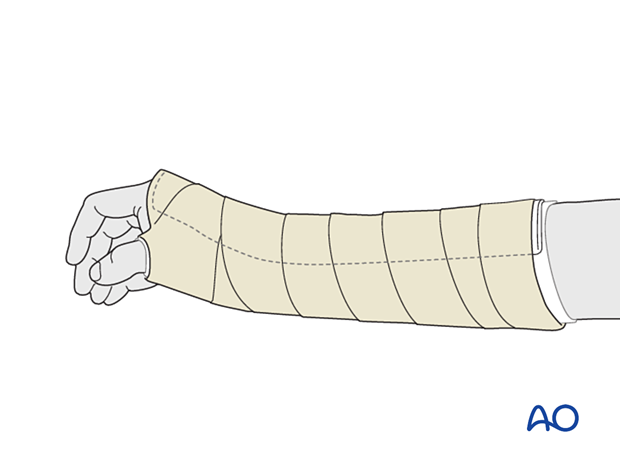
Immediate postoperative treatment
Rest the wrist with a well-padded below-elbow splint for about 2–4 weeks.
Splinting helps with soft-tissue healing.
Follow-up
X-ray checks of joint position have to be performed immediately after the splint has been applied.
Follow-up x-rays with the splint should be taken after 1 week and possibly every 2 weeks.
The K-wire can be removed 4–6 weeks after surgery.
Splint immobilization is continued until about 4 weeks after the injury. At that time, an x-ray without the splint is taken to confirm healing, and range of motion should be pain-free.













