ORIF through Kocher-Langenbeck
1. General considerations
Sequence of the treatment
For ORIF of posterior column fractures with Kocher-Langenbeck approach, the following surgical sequence is common:
- Joint distraction and removal of incarcerated fragments
- Reduction of femoral head dislocation if not achieved closed on admission
- Reduction
- Assessment of reduction
- Fixation of the posterior column fragment with a interfragmentary screw and a reconstruction plate
Planning/templating
Preoperative templating is essential for understanding the complexity of an acetabular fracture.
When using implants on the innominate bone, it is important to know the best starting points for obtaining optimal screw anchorage (see General stabilization principles and screw directions).
Patient positioning
The Kocher-Langenbeck approach for posterior column fractures can be performed in either the prone or lateral position.
If a hip dislocation is expected, then the patient should be placed in the lateral position to allow sufficient freedom of movement of the leg. If the hip is only to be subluxed, then the prone position may also be utilized.
The following sections represent the approach in the prone position.
The maintenance of knee flexion (at 90°) and hip extension throughout the procedure reduces tension on the sciatic nerve.
Sciatic nerve injury
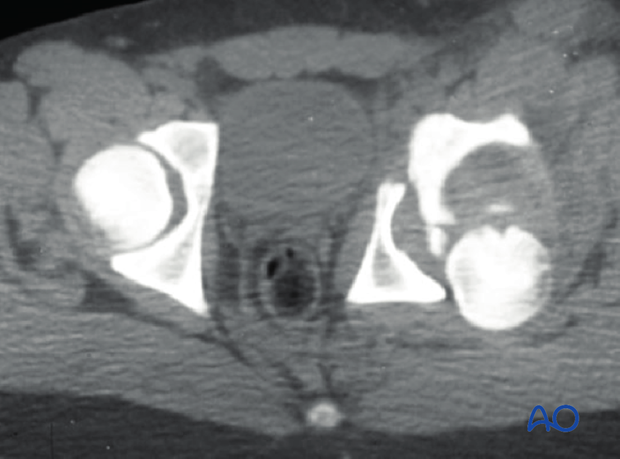
Posterior wall fractures, elemental and associated, usually result from posterior hip dislocation. The sciatic nerve may be injured. Post reduction CT will be used to evaluate the fracture characteristics.
Indirect visualization
Unusually for a significant joint, articular reduction of acetabular fractures is indirect. The articular surface of the hip joint is not seen directly. Reduction must be assessed by the appearance of the extraarticular fracture lines and intraoperative fluoroscopic assessment. Some fracture lines are palpated manually but not seen directly such as transverse fracture lines on the quadrilateral plate.
Quality of reduction
Posttraumatic arthrosis is directly related to the quality of reduction - the better the reduction, the greater the chance of a good or excellent result.
2. Joint distraction
Application of traction
Traction on the femur, laterally or distally, increases the joint space.
This will help:
- Expose the joint
- Remove loose fragments
- Reduce some marginal impaction fractures
Traction can be applied in several ways, including:
- Lateral manual traction applied via the greater trochanter (as demonstrated)
- Distal manual traction applied via a distal femoral traction pin
- With a femoral distractor (see below)
- With a fracture table
In some surgeon’s experience, the use of a traction table post or other traction frame is helpful during this operation.
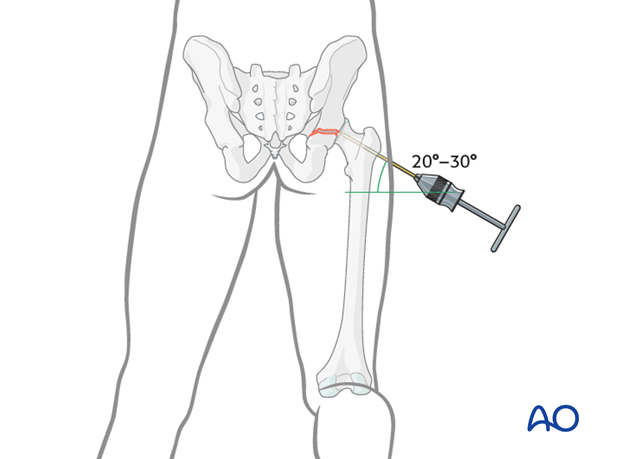
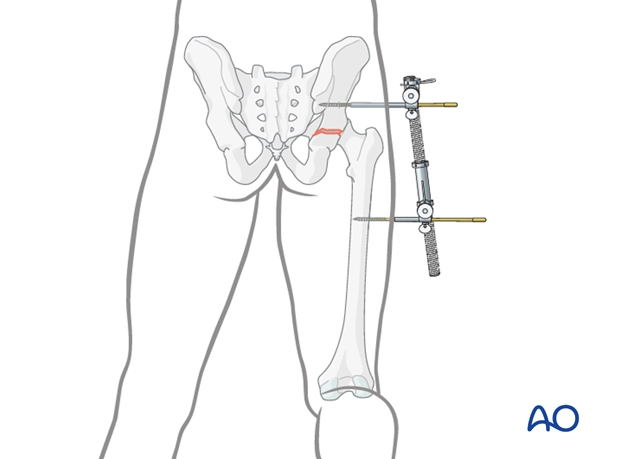
Traction with a femoral distractor
One way to apply traction is with a large distractor. This avoids both constant pulling and use of the fracture table, but does limit mobility of the hip. Properly placed, the distractor may properly realign the femoral head.
Insert a 5 mm Schanz screw into the sciatic buttress well above the level of the fracture. Place a second Schanz screw into the femur at the level of the lesser trochanter.
Tension on the distractor can be adjusted as needed for visualization or reduction.
Teaching video
AO teaching video: Use of the distractor on the pelvis
3. Cleaning of the fracture site
Cleaning and irrigation
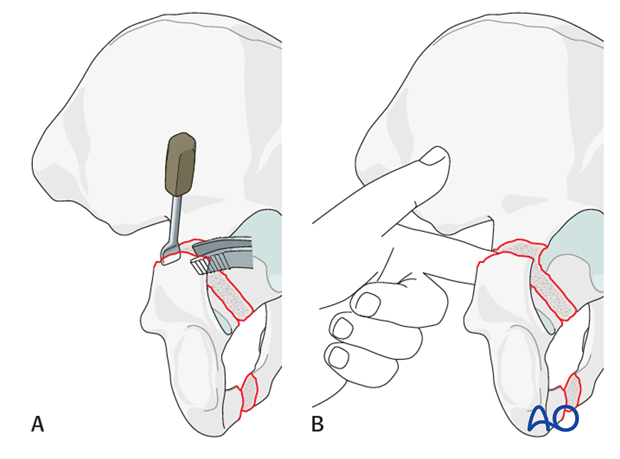
Exposure is completed subperiosteally at the fracture site on the retroacetabular surface. The fracture can be distracted carefully with a lamina spreader or with distal fragment manipulation via a Schanz screw applied to the ischial tuberosity.
The periosteum along the quadrilateral surface can be cleaned from the fracture site either through the distracted fracture (A) or with a finger or periosteal elevator applied through the sciatic notch (B).
Clean and irrigate the fracture site in preparation for the direct reduction.
Removal of incarcerated fragments
Incarcerated fragments should be identified on the preoperative CT scan. Their removal and cleaning of the joint is mandatory. This requires the previously described traction.
In the situation of an isolated PC fracture, without a posterior wall component, it may be difficult to visualize the intraarticular environment. Inspection of the joint may be obtained by distracting the fracture and working through the fracture edges.
4. Reduction
Femoral head dislocation
A posterior dislocation of the femoral head is typically associated with the posterior column acetabular fracture. This should have been reduced provisionally as part of initial management. The hip may re-dislocate during exposure and re-reduction will be necessary.
During definitive posterior column reduction, the femoral head must be properly reduced against the superior-anterior stable portion of the acetabulum. The femoral head thus becomes a template for proper posterior column reduction. Improper position of the head prevents satisfactory fracture reduction.

With the femoral head properly reduced, the mobile inferior portion of the posterior column must be repositioned. This requires correction of its medial and distal displacement and internal rotation. Direct manipulation and provisional stabilization with clamps are to be used. Once a satisfactory provisional reduction is achieved and confirmed, definitive fixation is applied.
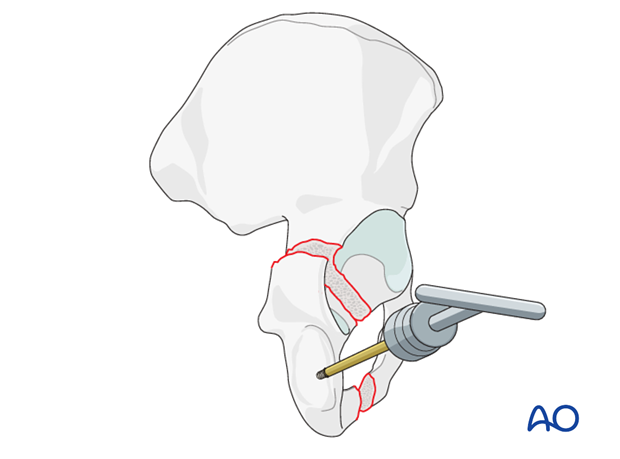
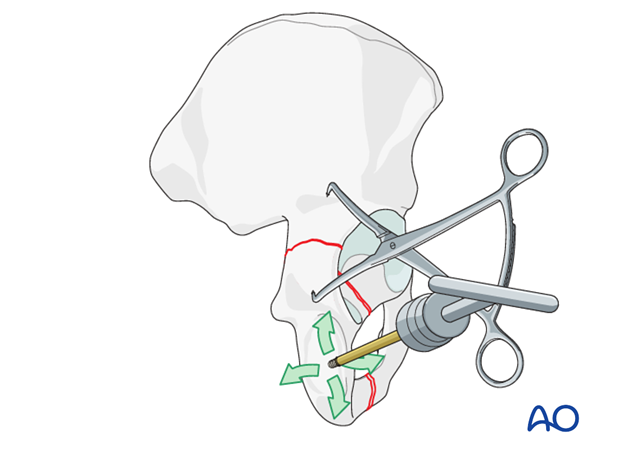
Ischial Schanz screw as a handle
A Schanz screw is placed into the ischial tuberosity to act as a handle or joystick. This is a key aid for manipulating the posterior column fragment.
The orientation of the screw is directed from lateral to medial and is typically applied through the muscular insertions overlaying the tuberosity. The muscles do not need to be elevated from the bone to allow screw placement.
Care should be taken to avoid blocking the fracture environment with this screw. A proximal to distal trajectory should be avoided, as the Schanz screw will block subsequent adjuncts for fracture reduction at the retroacetabular surface.
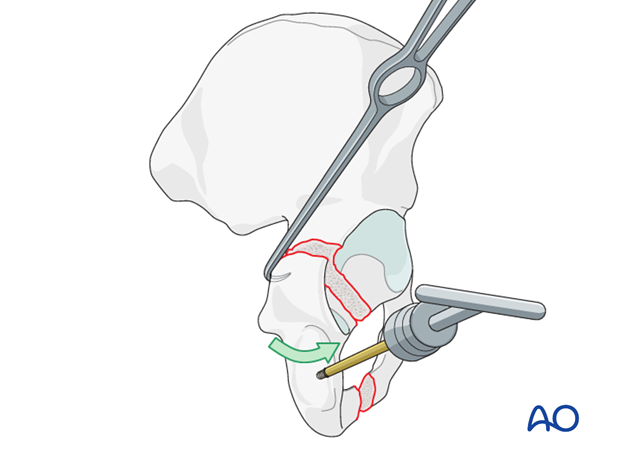
Use of pointed push pull devices
Fracture adjustment requires fine manipulation at the fracture itself. There are several adjuncts that can accomplish this fine adjustment.
Rotation and fine adjustment of this fragment is aided with a bone hook, sharp dental hooks, and/or ball spike pusher.
Manipulation with a hook placed as shown demonstrates mobility of the posterior column, and helps in the reduction. If reduction is difficult, check the fracture site for interposed debris.
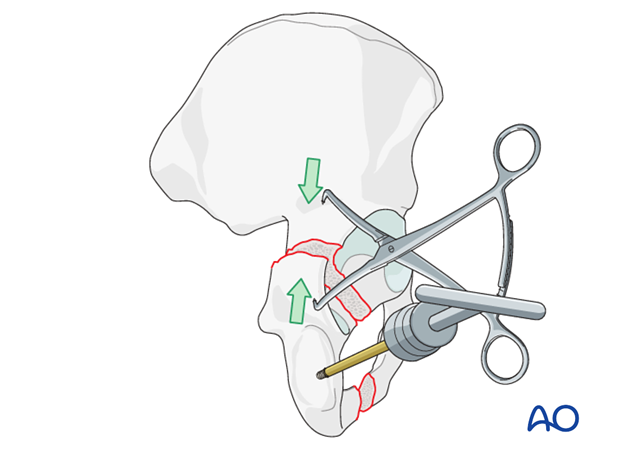
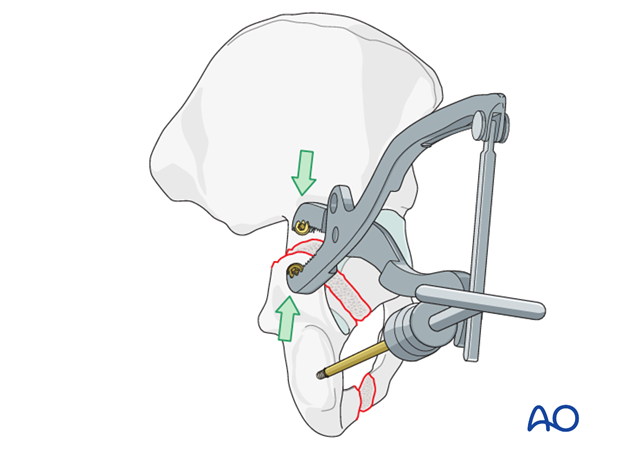
Use of pointed reduction forceps
The pointed reduction forceps is a very powerful way of manipulating the reduction along the fracture line and applying compression.
Due to the convexity of the bone, small holes may need to be drilled into the cortex to allow clamp application, and to prevent the points from slipping.
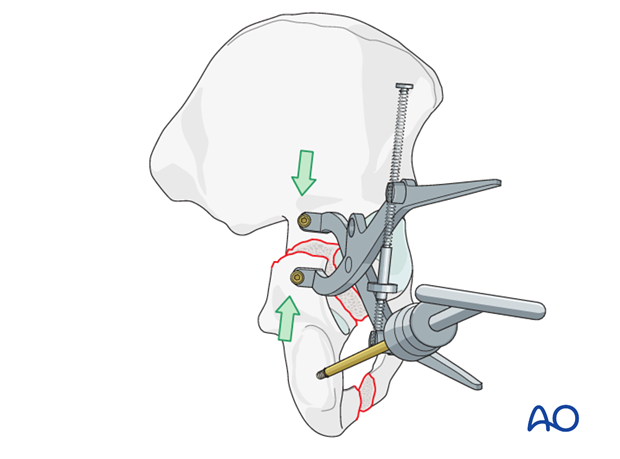
Use of a Farabeuf clamp
This clamp has jaws shaped to fit around screw heads. It can be used to compress fracture surfaces with two properly placed 3.5 mm cortical screws. They should be securely placed, and a little prominent, to be grasped by the clamp.
Properly placed, this clamp can both de-rotate the posterior column, and approximate the fracture fragments.
Care should be taken, as poor clamp placement may pressure the sciatic nerve.
Use of a Jungbluth clamp
The Jungbluth pelvic reduction clamp is a similar alternative, which requires a larger exposure and also depends upon proper screw placement so that the forces applied by the clamp correctly realign the fracture.
A proximal screw is placed in the superior portion of the iliac wing above the acetabulum.
A distal screw is placed in the posterior column above the ischial tuberosity.
Their positions determine the direction of applied force, and this must be perpendicular to the fracture plane.
The use of the screw-dependent clamps (the Jungbluth and Farabeuf) creates the potential problem of screw traffic. Care must be taken to avoid placing these screws in the way of provisional and definitive fixation screws.
Articular surface reduction
In the elementary posterior column fracture, the articular surface cannot be easily visualized once the fracture has been reduced. This is different than the associated posterior column/wall fracture, in which the posterior column articular reduction can be assessed through the displaced posterior wall fragment.
Intraarticular inspection may be possible by opening the hip capsule with an incision parallel to the acetabular border, avoiding damage to the labrum. Inspection of the joint surface demonstrates reduction.
The reduction of the cortical surfaces of the fracture acts as a surrogate for articular reduction. Visualization of the fraction line along the cortical retroacetabular surface and palpation of the fracture along the quadrilateral surface together indicate the quality of the obtained reduction.
Examine the reduction by inserting a finger or an appropriate instrument along the quadrilateral plate. With a satisfactory reduction, the quadrilateral surface should have no palpable gap or step-off.
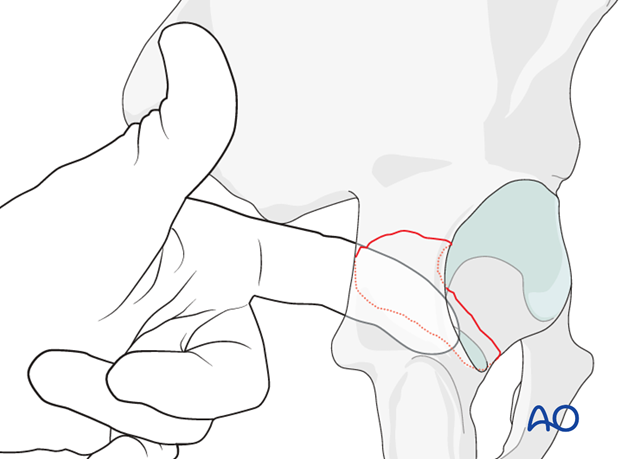
Additional manipulation of translation and rotation of the posterior column fragment should occur until both the internal palpation and external visualization demonstrate an anatomical reduction.
To mobilize the posterior column in cases older than 3 weeks, cut the sacrospinous ligament at its insertion on the ischial spine to aid mobilization of the fragment.
5. Fixation
Preliminary fixation
Once an anatomic reduction is obtained, provisional fixation is added to augment the clamp acquired reduction.
K-wires spanning the fracture are used with care taken to avoid intraarticular penetration. Provisional small fragment plates (2.4 mm, 2.7 mm) can be applied.
Care should be taken to place all provisional fixation outside the region required for the definitive fixation strategy.
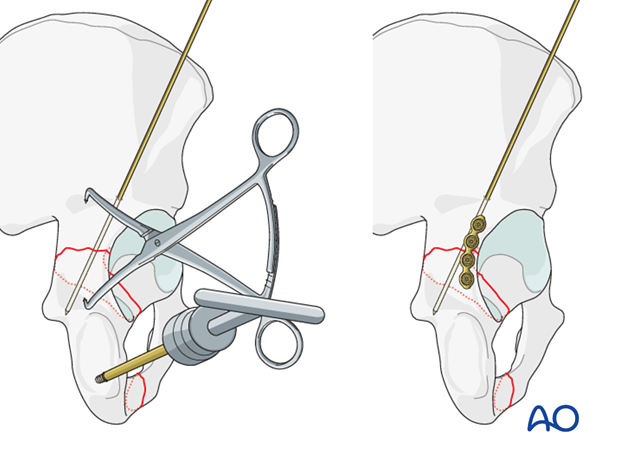
Interfragmentary lag screw
If possible, begin definitive fixation with an interfragmentary lag screw, placed from the distal fragment, into the posterior buttress of the ilium. The trajectory of this screw often requires a percutaneous insertion through the posterior gluteus musculature. Great care must be taken not to compromise the sciatic nerve.
The gliding hole may be drilled before reduction to ensure its proper placement.
Screw placement must allow optimal plate positioning as described below.
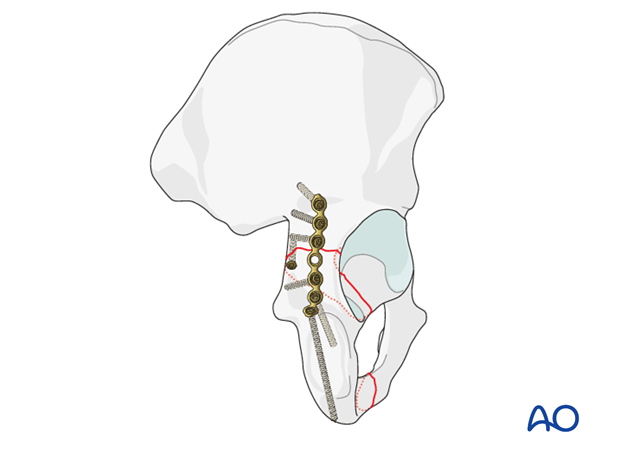
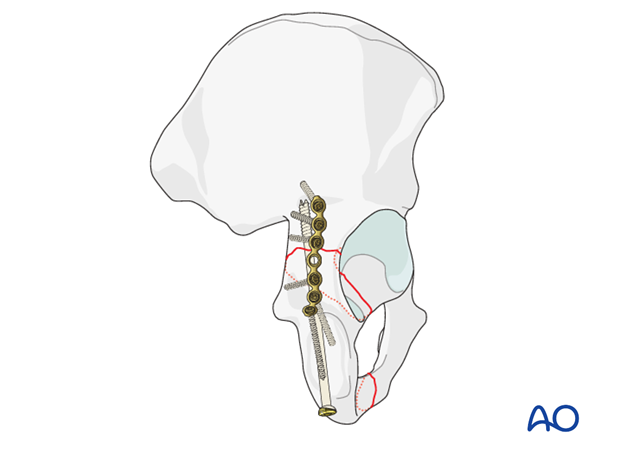
Contouring of the plate with a template
In addition to the lag screw, a reconstruction plate will be applied. The two points of fixation will provide torsional stability to the ultimate construct. In cases where a lag screw cannot be utilized, a second plate is used to provide the torsional stability.
A reconstruction plate is chosen to reconstitute the structural stability of the native posterior column and the sciatic buttress. Ideally, it will be applied to the mid-column and contoured to obtain purchase in the strong bone of the sciatic buttress.
An aluminum template can be bent to fit the pelvis in the optimal location. The plate positioning will be limited cranially by the superior gluteal nerve and vascular pedicle. The distal end of the plate will be contoured to optimize screw positioning down the ischial ramus.
The plate contour should enforce the vectors required for the reduction.

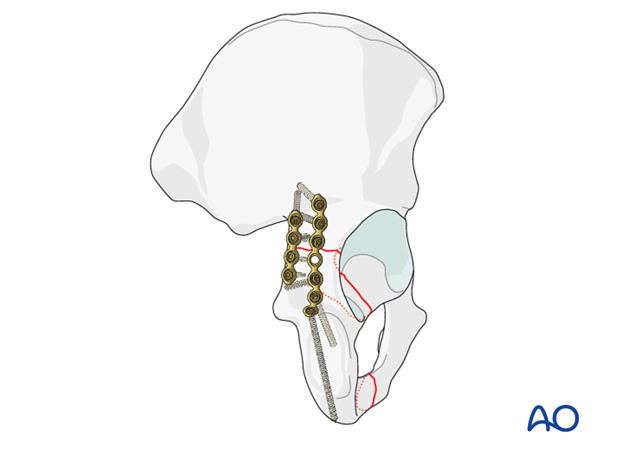
Application of the reconstruction plate
Definitive stabilization is obtained by adding the reconstruction plate spanning the posterior column and anchored securely to the ilium and ischium.
The screws placed in the periarticular portion of the plate must be positioned carefully to avoid intraarticular perforation. This becomes more probable as the plate is positioned laterally and closer to the acetabular rim.
Alternative definitive fixations
Medial plate
If a lag screw cannot be inserted satisfactorily, a short plate across the fracture can be applied along the posterior border of the bone at the margin of the sciatic notch. This will ensure torsional stability, not afforded by a single plate.
This often requires the reconstruction plate to be positioned slightly more laterally.
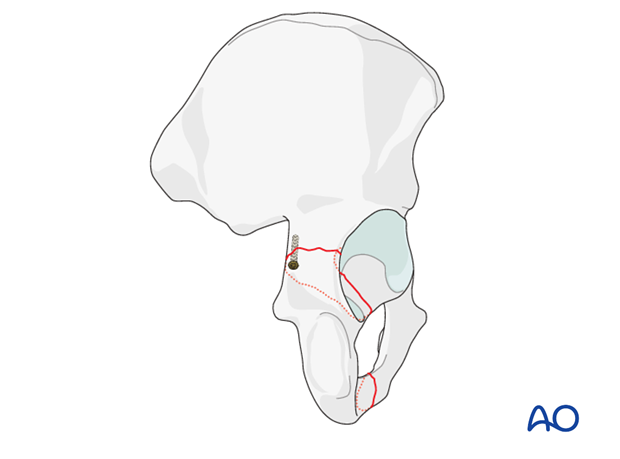
Posterior column screw
The posterior column may be well stabilized initially with the insertion of a 7.3 mm partially threaded cannulated screw. This is inserted through a separate stab incision in the buttock crease over a guide wire.
The starting point is at the ischial tuberosity, and a finger in the greater sciatic notch is used to guide the wire and screw up the posterior column, exiting at the pelvic brim.
Care should be taken to protect the sciatic nerve at the level of the ischial tuberosity.
The use of a screw aids the placement of the posterior wall plate as it increases the freedom of placement of the wall plate.
This is commonly referred to as the “butt screw”.
Pitfall: Injury to gluteal vessels and nerve
Proximally, retraction and plate and screw placement may result in neurovascular injury. Careful retraction and attention to plate location are essential to protect these fragile structures.
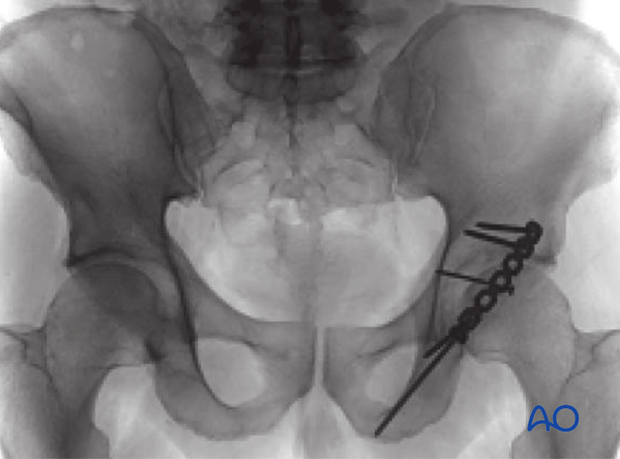
6. Radiographic assessment
Intraoperative confirmation of hardware position
Intraoperative fluoroscopic images (AP, obturator oblique, iliac oblique) should be obtained to confirm the fracture reduction quality and the congruence of the femoral head.
A true lateral or exaggerated obturator oblique should be obtained to ensure that all placed screws are extraarticular.

Final radiographic assessment
The final AP, obturator oblique and iliac oblique radiographs demonstrate:
- The anatomic reduction
- Lag screw positioning from the distal fragment into the intact ilium
- The optimal plate position utilizing the sciatic buttress and the ischial ramus for secure fixation
- The plate contour reinforcing the vectors required for reduction
- Concentric reduction of the femoral head
Postoperatively, obtain formal high-quality radiographs of AP and both oblique views.
7. Postoperative care
During the first 24-48 hours, antibiotics are administered intravenously, according to hospital prophylaxis protocol. In order to avoid heterotopic ossification in high-risk patients, the use of indomethacin or single low dose radiation should be considered. Every patient needs DVT treatment. There is no universal protocol, but 6 weeks of anticoagulation is a common strategy.
Wound drains are rarely used. Local protocols should be followed if used, aiming to remove the drain as soon as possible and balancing output with infection risk.
Specialized therapy input is essential.
Follow up
X-rays are taken for immediate postoperative control, and at 8 weeks prior to full weight bearing.
Postoperative CT scans are used routinely in some units, and only obtained if there are concerns regarding the quality of reduction or intraarticular hardware in others.
With satisfactory healing, sutures are removed around 10-14 days after surgery.
Mobilization
Early mobilization should be stressed and patients encouraged to sit up within the first 24-48 hours following surgery.
Mobilization touch weight bearing for 8 weeks is advised.
Weight bearing
The patient should remain on crutches touch weight bearing (up to 20 kg) for 8 weeks. This is preferable to complete non-weight bearing because forces across the hip joint are higher when the leg is held off the floor. Weight bearing can be progressively increased to full weight after 8 weeks.
With osteoporotic bone or comminuted fractures, delay until 12 weeks may be considered.
Implant removal
Generally, implants are left in situ indefinitely. For acute infections with stable fixation, implants should usually be retained until the fracture is healed. Typically, by then a treated acute infection has become quiescent. Should it recur, hardware removal may help prevent further recurrences. Remember that a recurrent infection may involve the hip joint, which must be assessed in such patients with arthrocentesis. For patients with a history of wound infection who become candidates for total hip replacement, a two-stage reconstruction may be appropriate.
Sciatic nerve palsy
Posterior hip dislocation associated with posterior wall, posterior column, transverse, and T-shaped fractures can be associated with sciatic nerve palsy. At the time of surgical exploration, it is very rare to find a completely disrupted nerve and there are no treatment options beyond fracture reduction, hip stabilization and hemostasis. Neurologic recovery may take up to 2 years. Peroneal division involvement is more common than tibial. Sensory recovery precedes motor recovery and it is not unusual to see clinical improvement in the setting of grossly abnormal electrodiagnostic findings.













