ORIF, 1-point fixation (without orbital reconstruction)
1. Principles
In some situations a surgeon may have a simple noncomminuted zygomatic-complex fracture which with open manipulation snaps into a perfect reduction. This has often been achieved with a maxillary vestibular approach. This approach allows visualization of both the lateral maxillary buttress and the infraorbital rim. Particularly in patients where CT has revealed no separation at the fracture of the zygomaticofrontal suture, and with good intraoperative visualization, and reduction of the lateral maxillary buttress and the inferior orbital rim, 1-point fixation with a plate between the maxilla and zygoma may be adequate. An existing laceration may also be used.
Correct anatomical reduction is required to reproduce the original structure of the zygomaticomaxillary complex and the proper alignment of the orbital walls. In order to achieve proper reduction of the lateral orbital wall the greater wing of the sphenoid and the zygoma must be properly aligned.
The aim is to restore the proper orbital volume and to restore proper width, AP projection, and height of the midface. Proper reduction of the zygoma addresses the issues of AP projection of the width of the midface.
It is possible that the periorbital contents may have been affected by the reduction of the zygomatic-complex fracture. Forced duction tests should be performed before and after reduction of the zygoma to make sure that the patient does not have entrapment of the soft tissues. Pre- and postoperative ophthalmologic exams should be considered in all patients who have sustained periorbital trauma.
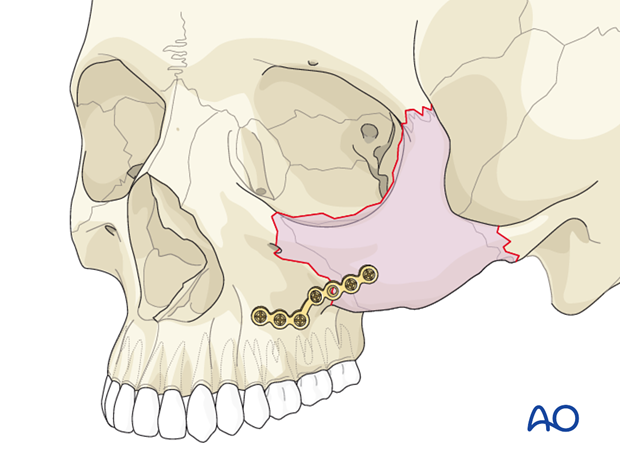
For the purpose of this discussion of the 1-point fixation technique for the zygomatic complex, the plate has been placed on the zygomaticomaxillary buttress.
2. Zygoma reduction methods
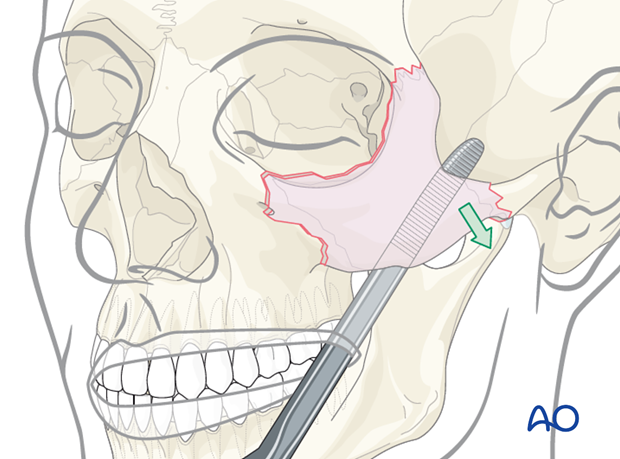
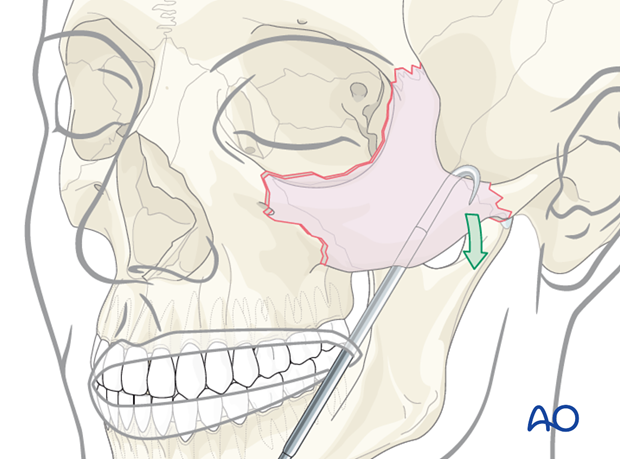
The first step is to obtain proper 3-D reduction of the zygoma using an elevator, hook, screw, or Carroll-Girard type device to mobilize the zygoma into its proper position.
Illustration shows reduction being performed via a transoral (Keen) approach placed through the maxillary vestibular incision using an elevator …
… or using a hook.
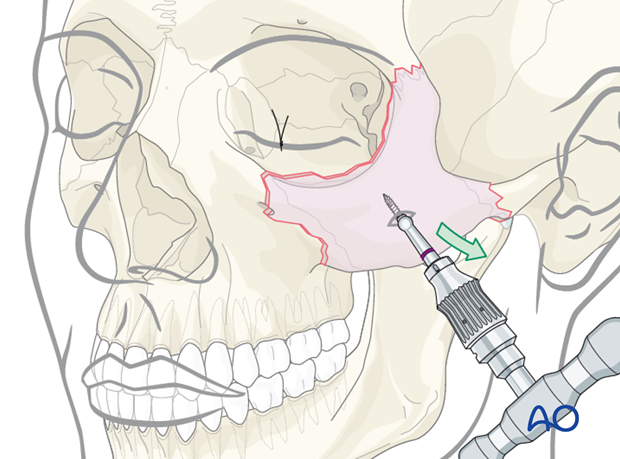
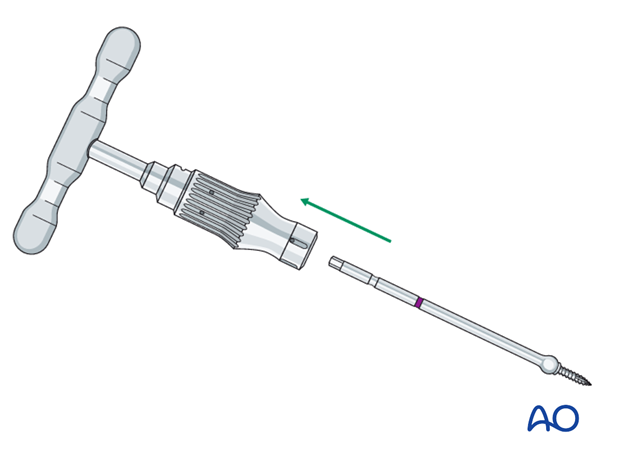
Threaded reduction tool
A threaded reduction tool (Carroll-Girard screw) is inserted into the zygoma through the lower eyelid incision or directly through the skin of the face and used for reduction.
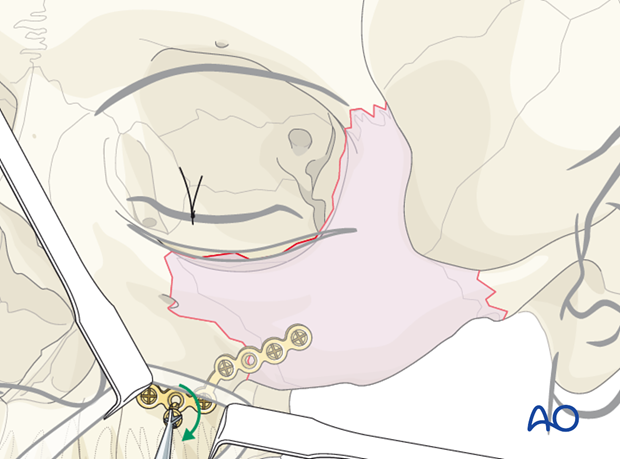
3. Placement and fixation
Looking through the maxillary vestibular approach, the fracture of the zygomaticomaxillary buttress is aligned. A larger L-shaped plate is ideal for the fixation of this fracture. This is the most difficult plate to properly adapt in a zygoma fracture. It is important that the leg of the L-plate be placed on the most lateral portion of the lateral maxillary buttress, where the bone is fairly thick.
It is similarly important that the foot of the L-plate is placed along the alveolar bone in a manner that the screws will not be placed into the dental roots. A common problem with this third plate is failure to properly adapt the L-plate, resulting in screw placement into the thin wall of the anterior maxillary sinus. It is not uncommon for the lateral maxillary buttress to be comminuted. In this instance using a longer L-plate with multiple screw holes may be ideal.
A stronger plate is recommended for the zygomaticomaxillary buttress.
4. Aftercare
Evaluation of the patients vision is performed as soon as they are awakened from anesthesia and then at regular intervals until they are discharged from the hospital.
A swinging flashlight test may serve in the unconscious and/or noncooperative patient; alternatively electrophysiological examination has to be performed but is dependent on the appropriate equipment (VEP).
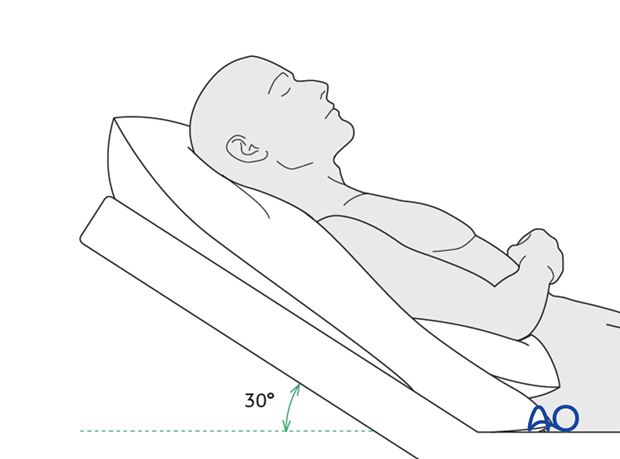
Postoperative positioning
Keeping the patient’s head in an upright position both preoperatively and postoperatively may significantly improve periorbital edema and pain.
Nose-blowing
To prevent orbital emphysema, nose-blowing should be avoided for at least 10 days following orbital fracture repair.
Medication
The use of the following perioperative medication is controversial. There is little evidence to make strong recommendations for postoperative care.
- No aspirin or nonsteroidal antiinflammatory drugs (NSAIDs) for 7 days
- Analgesia as necessary
- Antibiotics (many surgeons use perioperative antibiotics. There is no clear advantage of any one antibiotic, and the recommended duration of treatment is debatable.)
- Nasal decongestant may be helpful for symptomatic improvement in some patients.
- Steroids, in cases of severe orbital trauma, may help with postoperative edema. Some surgeons have noted increased complications with perioperative steroids.
- Ophthalmic ointment should follow local and approved protocol. This is not generally required in case of periorbital edema. Some surgeons prefer it. Some ointments have been found to cause significant conjunctival irritation.
- Regular perioral and oral wound care has to include disinfectant mouth rinse, lip care, etc.
Ophthalmological examination
Postoperative examination by an ophthalmologist may be requested. The following signs and symptoms are usually evaluated:
- Vision (except for alveolar ridge fracture, palatal fracture)
- Extraocular motion (motility) (except alveolar ridge fracture, palatal fracture)
- Diplopia (except Le Fort I, alveolar ridge fracture, palatal fracture)
- Globe position (except Le Fort I, alveolar ridge fracture, palatal fracture)
- Perimetric examination (except Le Fort I, alveolar ridge fracture, palatal fracture)
- Lid position
- If the patient complains of epiphora (tear overflow), the lacrimal duct must be checked.
Note: In case of postoperative double vision, ophthalmological assessment has to clarify the cause. Use of prism foils on existing glasses may be helpful as an early aid.
Postoperative imaging
Postoperative imaging has to be performed within the first days after surgery. 3-D imaging (CT, cone beam) is recommended to assess complex fracture reductions. An exception may be made for centers capable of intraoperative imaging.
Especially in fractures involving the alveolar area, orthopantomograms (OPG) are helpful.
Wound care
Remove sutures from skin after approximately 5 days if nonresorbable sutures have been used.
Apply ice packs (may be effective in a short term to minimize edema).
Avoid sun exposure and tanning to skin incisions for several months.
Diet
Diet depends on the fracture pattern.
Soft diet can be taken as tolerated until there has been adequate healing of the maxillary vestibular incision.
Intranasal feeding may be considered in cases with oral bone exposure and soft-tissue defects.
Patients in MMF will remain on a liquid diet until such time the MMF is released.
Clinical follow-up
Clinical follow-up depends on the complexity of the surgery, and whether the patient has any postoperative problems.
With patients having fracture patterns including periorbital trauma, issues to consider are the following:
- Globe position
- Double vision
- Other vision problems
Other issues to consider are:
- Facial deformity (incl. asymmetry)
- Sensory nerve compromise
- Problems of scar formation
Issues to consider with Le Fort fractures, palatal fractures and alveolar ridge fractures include:
- Problems of dentition and dental sensation
- Problems of occlusion
- Problems of the temporomandibular joint (TMJ), (lack of range of motion, pain)
Eye movement exercises
Following orbital fractures, eye movement exercises should be considered.
Implant removal
Implant removal is rarely required. It is possible that this may be requested by patients if the implant becomes palpable or visible. In some countries it will be more commonly requested. There have been cases where patients have complained of cold sensitivity in areas of plate placement. It is controversial whether this cold sensitivity is a result of the plate, a result of nerve injury from the original trauma, or from nerve injury due to trauma of the surgery. Issues of cold sensitivity generally improve or resolve with time without removal of the hardware.
Generally, orbital implant removal is not necessary except in the event of infection or exposure. Readmission might be indicated if long term stability of the orbital volume has not been maintained.
MMF
The duration and/or use of MMF is controversial and highly dependent on the particular patient and complexity of the trauma. In some cases where long-term MMF may be recommended, the surgeon may choose to leave the patient out of MMF immediately postoperatively because of concerns of edema, postoperative sedation, and airway. In these cases the surgeon may choose to place the patient in MMF after these concerns have been resolved.
The need and duration of MMF is very much dependent on:
- Fracture morphology
- Type and stability of fixation (including palatal splints)
- Dentition
- Coexistence of mandibular fractures
- Premorbid occlusion
Oral hygiene
Patients with arch bars and/or intraoral incisions and/or wounds must be instructed in appropriate oral hygiene procedures. The presence of the arch bars or elastics makes this a more difficult procedure. A soft toothbrush (dipped in warm water to make it softer) should be used to clean the surfaces of the teeth and arch bars. Elastics are removed for oral hygiene procedures. Chlorhexidine oral rinses should be prescribed and used at least 3 times a day to help sanitize the mouth.
For larger debris, a 1:1 mixture of hydrogen peroxide/chlorhexidine can be used. The bubbling action of the hydrogen peroxide helps remove debris. A Waterpik® is a very useful tool to help remove debris from the wires. If a Waterpik is used, care should be taken not to direct the jet stream directly over intraoral incisions as this may lead to wound dehiscence.
Special considerations for orbital fractures
Travel in commercial airlines is permitted following orbital fractures. Commercial airlines pressurize their cabins. Mild pain on descent may be noticed. However, flying in military aircraft should be avoided for a minimum of six weeks.
No scuba diving should be permitted for at least six weeks.













