Closed treatment
1. Principles
Elevation of the arch is required if the fractured arch is impinging on the coronoid process of the mandible.
Closed reduction may also improve the patient’s cosmetic appearance in cases where significant depression of the zygomatic arch is present.
The drawback of closed reduction is that is difficult to know whether adequate reduction has been achieved without intraoperative radiographic imaging.
2. Intraoperative imaging
Intraoperative imaging has greatly improved the management of craniomaxillofacial trauma. Whenever available, an intraoperative CT scan should be obtained to verify the proper reduction of the fracture.
Read more about intraoperative CT scans here.
3. Reduction through indirect approaches
Closed reduction of isolated zygomatic arch fractures can be approached by either a percutaneous hook approach, a transoral (Keen) approach, or a temporal (Gillies) approach.
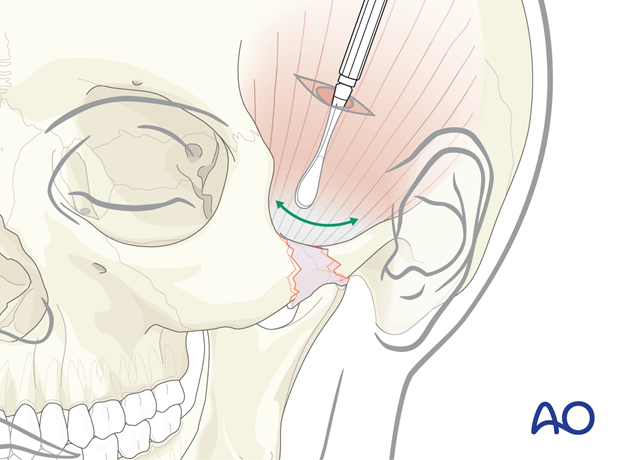
4. Percutaneous hook approach
A percutaneous hook is placed through a small incision in the skin.
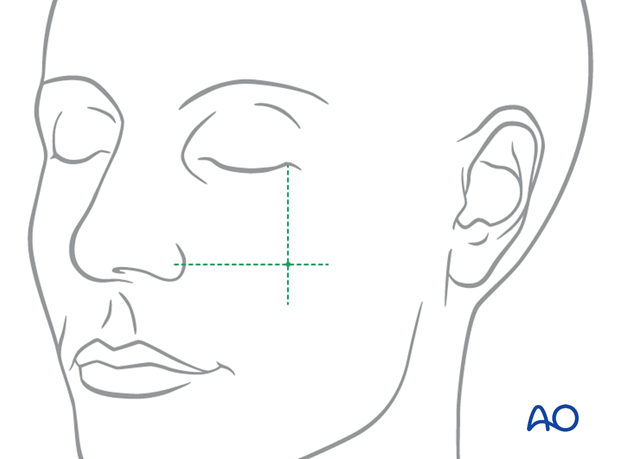
Two intersecting lines are drawn on the face to determine the proper location for applying the bone hook. The first line is vertical, dropped down from the lateral cantus of the eye (on the involved fracture side).
The second line is horizontal, drawn laterally from the ala of the nose.
The percutaneous bone hook is placed through the skin around the depressed zygomatic fracture segments and pulled laterally.
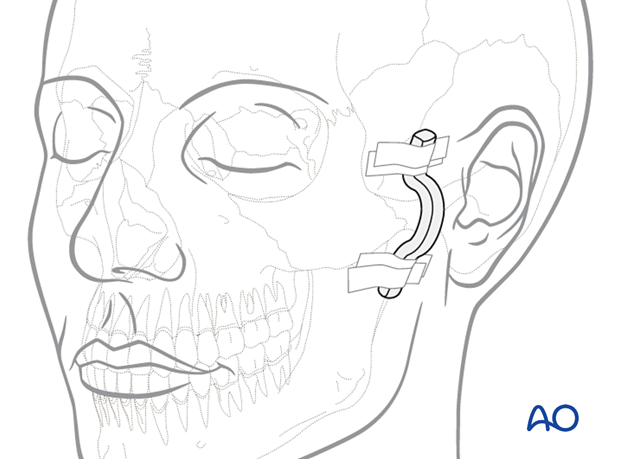
Protection of reduction
The force of the weight of the head resting on a pillow or further injury may be sufficient to displace even a properly reduced zygomatic fracture if the periosteum has been torn by repeated reduction movements. To prevent postoperative displacement of the reduced zygomatic arch, protection can be applied on the side of the face over the zygoma.
Many materials can be taped to the side of the head in the zygomatic arch fracture area to protect the reduced segment (eg, metal eye patches or aluminum finger splints bent in a staple configuration). Ideally, they should be left in place for 2–3 weeks.
Reduction using the transoral (Keen) approach
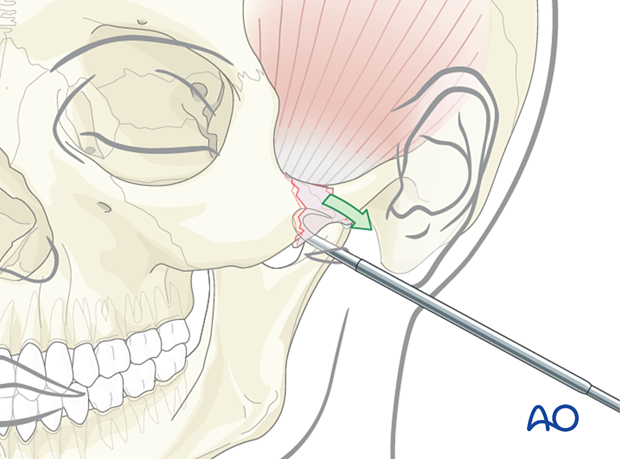
Because of the proximity of the intraoral incision, the surgeon can use a finger to direct the elevator and eventually palpate to check whether proper reduction has been achieved.
An elevator is used to elevate the zygomatic arch into its proper position.
Intraoperative imaging for confirmation of proper reduction can be used.
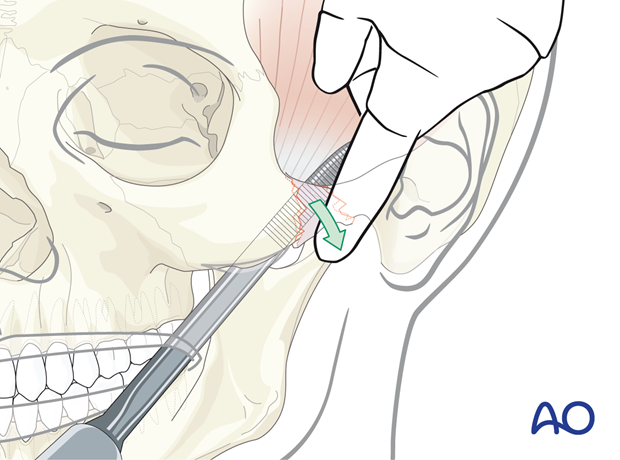
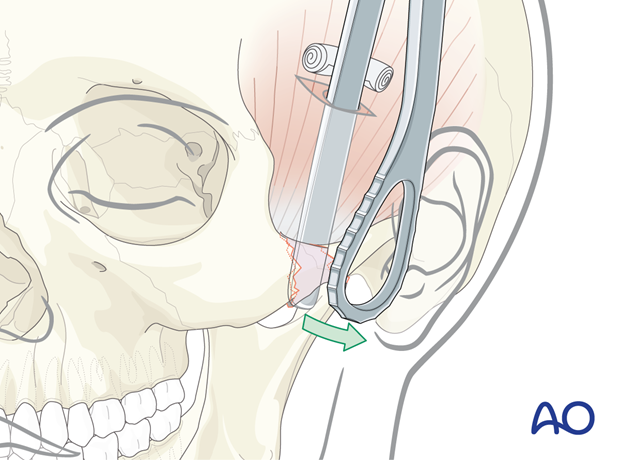
Reduction through the temporal (Gillies) approach
Through the temporal (Gillies) incision, a tunnel is created to pass an instrument deep to the deep layer of the temporalis fascia, superficial to the temporalis muscle and finally, deep to the zygomatic arch.
An elevator is used to elevate the zygomatic arch to its proper position.
The elevator passes between the temporalis muscle and the deep layer of the temporalis fascia.
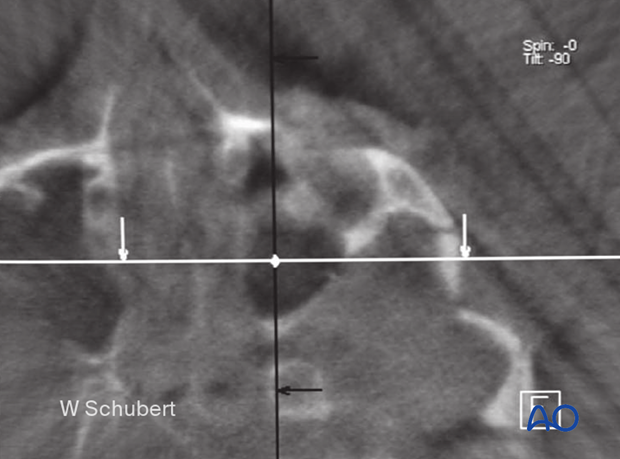
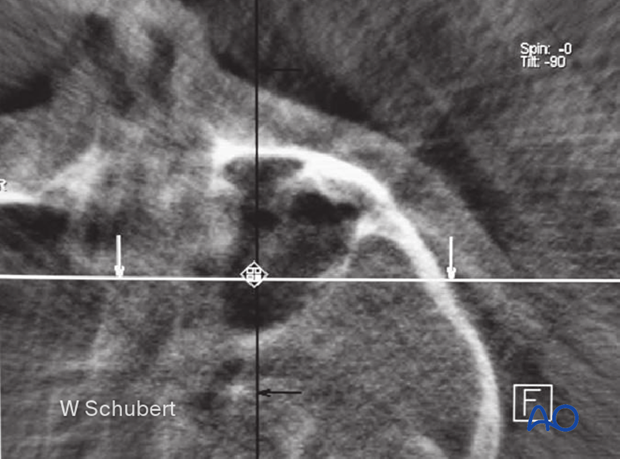
5. Case example
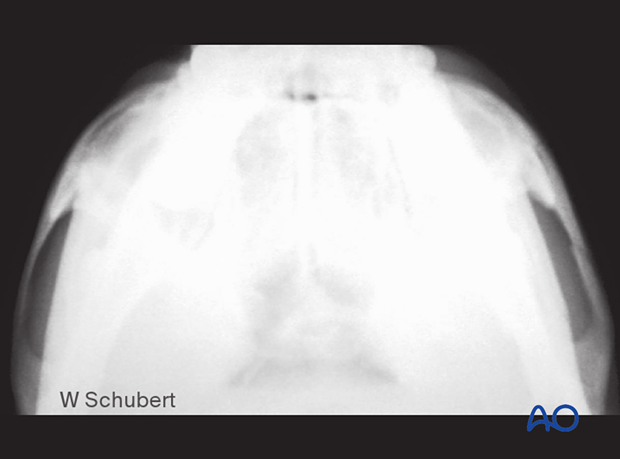
Intraoperative image before reduction of an isolated zygomatic arch fracture.
Intraoperative image after reduction of an isolated zygomatic arch fracture reduced via the transoral (Keen) approach.
6. Aftercare following closed treatment of zygomatic arch fractures
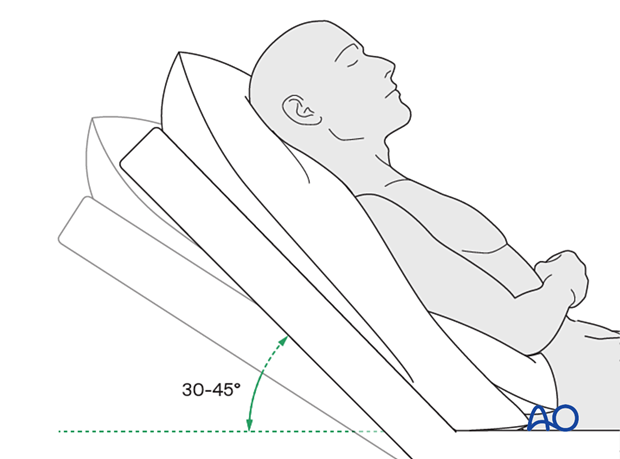
Postoperative positioning
Keeping the patient’s head in a raised position both preoperatively and postoperatively may significantly reduce edema and pain.
Medication
The use of the following perioperative medication is controversial. There is little evidence to make strong recommendations for postoperative care.
- Analgesia as necessary
- Antibiotics (Many surgeons use perioperative antibiotics. There is no clear advantage of any antibiotic, and the recommended duration of treatment is debatable.)
- Skin and intraoral wound care are used depending on the choice of incision. Regular oral wound care should include tooth brushing, disinfectant mouth rinses, and lip lubrication.
Postoperative imaging
Postoperative imaging, if performed, should be within the first few days after surgery. 3D imaging (CT, cone beam) is recommended to assess fracture reduction. An exception may be made for centers capable of intraoperative imaging.
A submentovertex view with standard plain x-ray can be used to visualize the reduction of the zygomatic arch fracture. These films may be obtained intraoperatively using a mobile x-ray unit.
Edema
Ice packs may be effective in the short term to minimize edema.
Diet
The patient can resume a normal diet the day following surgery.
A progressive diet should be considered for those with temporalis related injuries.
Clinical follow-up
Clinical follow-up may be performed after seven days from surgery to verify the following:
- Stability of the reduced fracture by gentle palpation of the zygomatic arch area
- Normal eye closure and upper lip function (to ensure no facial nerve injury)
- Resolution of trismus
Oral hygiene
Tooth brushing and mouth washes should be prescribed and used at least twice a day to help sanitize the mouth. Gently brushing the teeth occurs with a soft toothbrush (dipped in warm water to make the bristles softer).













