ORIF 1-point fixation (without orbital reconstruction)
1. Principles
Each fracture case should be individualized for treatment planning and execution because fixation requirements differ from one fracture to another. There are some general principles for fixation of zygomatic complex fractures when plate and screw fixation is used:
- Self-threading screws are utilized.
- Plate selection: titanium plates and screws have reduced scatter in postoperative CT scans. Selecting an L-, T-, or Y- shaped plate for zygomaticomaxillary buttress region fixation allows greater flexibility in positioning screws to avoid tooth roots in the alveolar process.
- Use a thin plate at, or preferably below, the infraorbital rim to minimize visibility and palpability. The skin and muscles overlying the infraorbital rim are thin and may atrophy with open reduction procedures.
- In cases that have concomitant fractures of other midfacial bones, it may be necessary to use additional points of fixation. Maxillomandibular fixation (MMF), should be completed before reduction and fixation are begun.
- Areas of bone loss: span the gap after initial reduction with a bone plate stabilized at either end of the defect. Alternatively, the comminuted fragments can be provisionally reassembled, stabilized with inter-fragment wires, their position improved, and the entire structure then stabilized with rigid fixation. In the case of extensive comminution with or without bone loss, judgment is required to fix the bone in the proper position without spanning the gap, or the pieces can be reassembled provisionally to confirm proper zygoma positioning. Generally, gaps over 5 mm can be bone grafted if native bone is unavailable. Grafts or comminuted fragments should be stabilized to the bone plate with individual fixation screws, the number of which is left to the operator’s judgment. This technique allows optimal osseous healing throughout the defect.
A correct anatomical reduction is required to reproduce the original structure of the zygomaticomaxillary complex and the proper alignment of the orbital walls. Fragments of the greater wing of the sphenoid and the orbital process of the zygoma should be appropriately aligned in a straight line to achieve an adequate contour in reduction of the lateral orbital wall.
The aim is to restore the orbital volume, the facial width, AP projection, and height of the midface. Proper reduction of the zygoma addresses the issues of AP projection and width of the midface.
Forced duction tests should be performed before and after reducing the zygoma to confirm that the extra-ocular muscle system has full and free excursion without entrapment.
Pre- and postoperative ophthalmologic examinations should be considered in all patients who have sustained periorbital trauma.
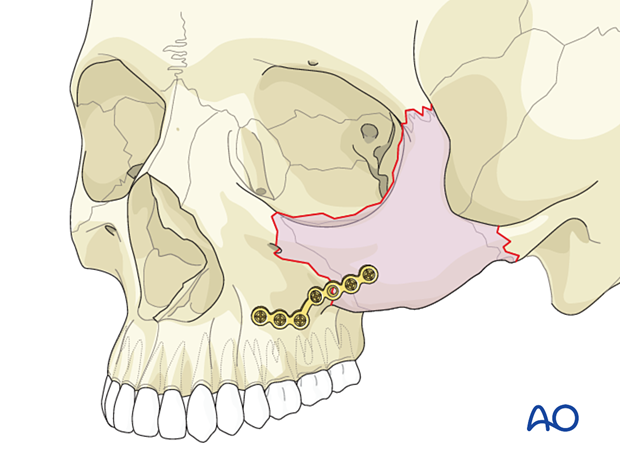
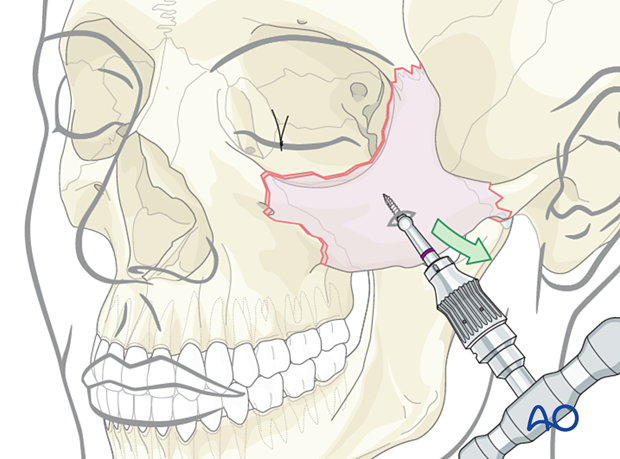
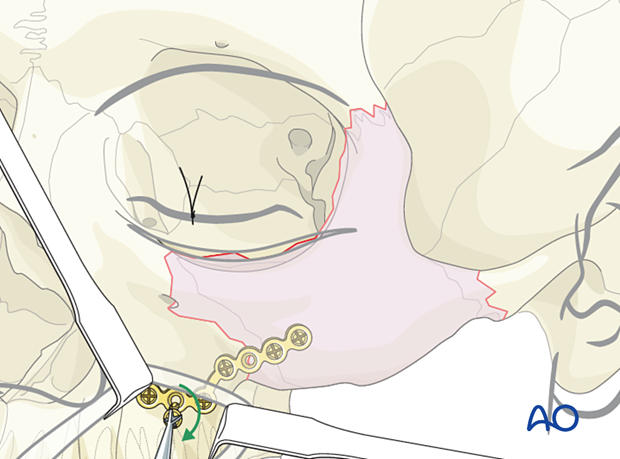
This illustration demonstrates a 1-point fixation technique of the zygomatic complex using a large L-shaped plate placed on the zygomaticomaxillary buttress.
2. Computer assisted surgery
Computer assisted surgery (CAS) has greatly improved the management of craniomaxillofacial trauma. Whenever available, an intraoperative CT scan should be obtained to verify the proper reduction of the fracture.
Read more about CAS here.
3. Approach
Maxillary vestibular approach
In certain simple noncomminuted zygomatic complex fractures, which snap into a perfect reduction after manipulation and are amenable to 1-point fixation, a maxillary vestibular approach can be used for the placement of the internal fixation device. This approach allows visualization of the lateral maxillary buttress, anterior wall of the maxillary sinus, and the infraorbital rim.
Alternatively, an approach through an existing laceration may be used, but converting to standard approaches for exposure is often preferable to extending existing lacerations.
Upper eyelid approaches
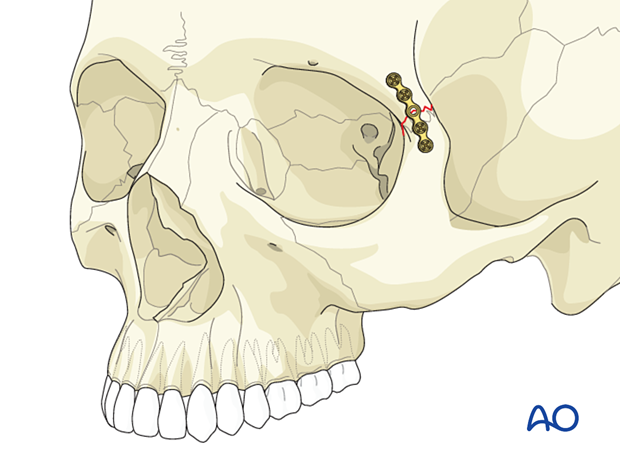
There are rare situations when a zygoma fracture can be stabilized with a single plate at the zygomaticofrontal suture.
One-point fixation can be performed at the zygomaticofrontal fracture in cases where confirmation of the alignment of the zygoma is confirmed at other fracture sites. A single bone plate may stabilize the zygoma when applied to the zygomaticofrontal suture through one of the upper eyelid approaches. The lateral aspect of an upper blepharoplasty is the preferred approach to the zygomaticofrontal suture. In this location, a 1.5 cm incision is all that is needed to apply the fixation plate. The incision is mobilized to visualize various portions of the plate in sequence, allowing for screw placement.
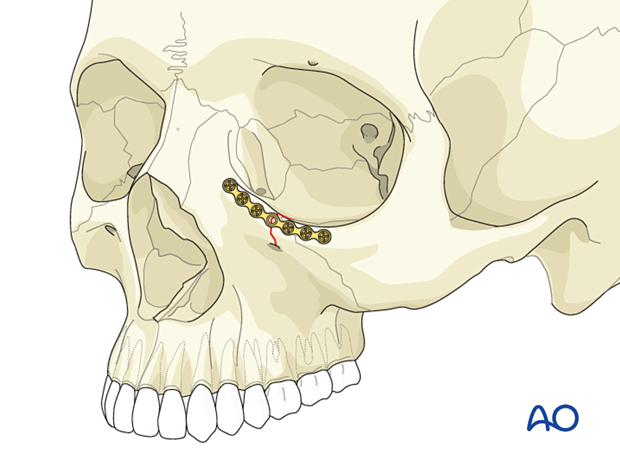
Lower eyelid approaches
Isolated fractures of the lower orbital rim, whether simple or comminuted, are frequent and may not involve the rest of the zygomatic complex. The inferior orbital rim and orbital floor may be affected. These injuries are adequately treated with a lower eyelid approach alone. One-point fixation can be performed at the infraorbital rim through a lower eyelid transcutaneous or a lower eyelid transconjunctival approach. Less commonly, an intraoral approach can be used for isolated rim fractures without significant internal orbital involvement.
4. Zygoma reduction methods
Reduction maneuvers
Mobilization and reduction of the zygomatic complex is achieved using a variety of instruments including elevators, hooks, screws, or Carroll-Girard type devices.
The reduction can be performed via a maxillary vestibular incision (Keen approach) using a Dingman elevator.
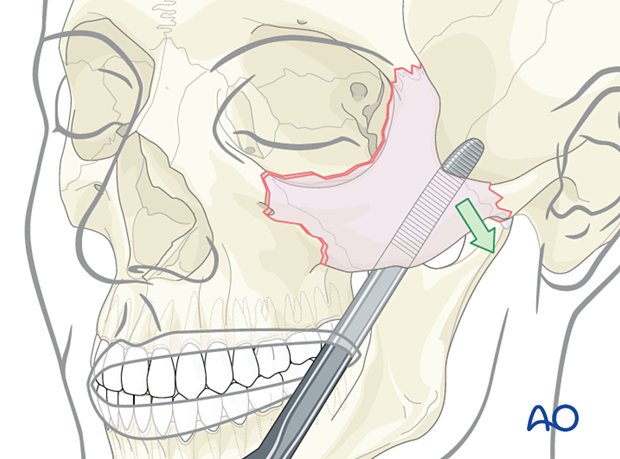
The reduction can also be performed using a hook.
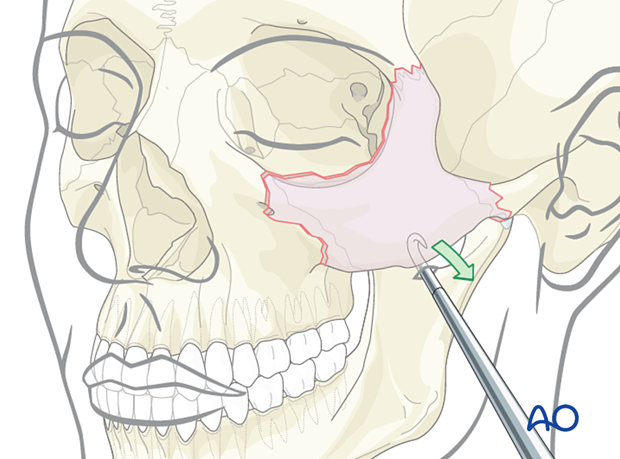
A Rowe zygoma elevator can also be used.
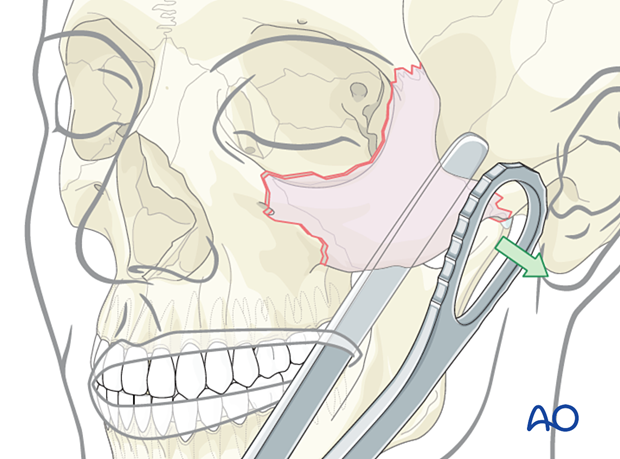
Threaded reduction tool
A threaded reduction tool (Carroll-Girard screw) can be inserted into the zygoma through the lower eyelid incision or directly through the skin and used for reduction.
5. Placement and fixation
The fracture of the zygomaticomaxillary buttress is aligned.
A thick L-shaped plate is ideal for the fixation of this fracture.
The leg of the L-plate must be placed on the most lateral portion of the lateral maxillary buttress, where the bone is fairly thick.
The foot of the L-plate must be placed along the alveolar bone. Each screw must be placed carefully, to avoid the dental roots.
A common problem is the failure to properly adapt the L-plate, resulting in screw placement into the thin wall of the anterior maxillary sinus.
Furthermore, it is not uncommon for the lateral maxillary buttress to be comminuted. In this instance, a longer span L-plate with multiple screw holes may be suitable.
6. Aftercare
Patient vision is evaluated after awakening from anesthesia and then at appropriate intervals.
A swinging flashlight test may serve the same function in the unconscious or noncooperative patient. In some centers, an electrophysiological examination can be utilized if the appropriate equipment is available (VEP).
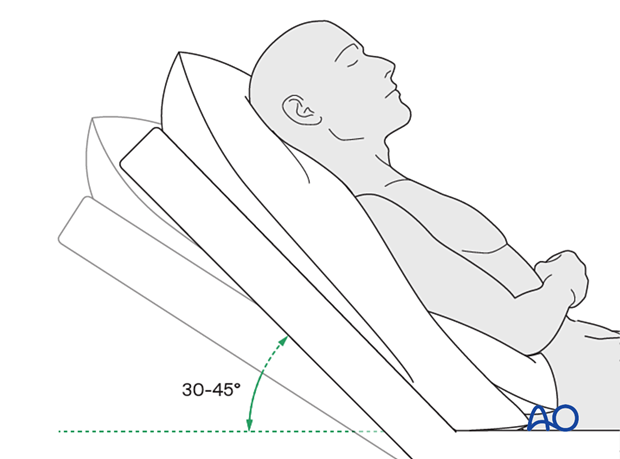
Postoperative positioning
Keeping the patient’s head in a raised position both preoperatively and postoperatively may significantly reduce edema and pain.
Nose blowing
Nose blowing should not involve pressing on the sides of the nose to increase intranasal pressure. Finger pressure on the nose should not accompany nose blowing for at least two weeks following orbital fracture repair to minimize the chance of orbital emphysema.
Medication
The use of the following perioperative medication is controversial. There is little evidence to make strong recommendations for postoperative care.
- No aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs) for seven days
- Analgesia as necessary
- Antibiotics (Many surgeons use perioperative antibiotics. There is no clear advantage beyond perioperative antibiotics, unless fracture repair has been delayed and there is maxillary sinus obstruction. Here the duration of treatment is dependent upon the circumstances.)
- Regular perioral and oral wound care must include disinfectant mouth rinse, lip care, etc.
Ophthalmological examination
Postoperative examination by an ophthalmologist may be requested if indicated. The following signs and symptoms are usually evaluated:
- Vision
- Extraocular motion (motility)
- Diplopia
- Globe position
- Perimetric examination
- Lid position
- If the patient complains of epiphora (tear overflow), the lacrimal duct must be checked
Postoperative imaging
Postoperative imaging should be performed within the first days after surgery. 3D imaging (CT, cone beam) is recommended to assess complex fracture reductions. An exception may be made for centers capable of intraoperative imaging.
Wound care
Ice packs may be effective in the short term to minimize edema.
Remove sutures from the skin after approximately five days.
Avoid sun exposure and tanning to skin incisions for several months.
Diet
Diet depends on the fracture pattern.
A soft diet can be taken as tolerated until there has been adequate healing of the maxillary vestibular incision.
Nasogastric feeding may be considered in cases with oral bone exposure and soft-tissue defects.
Patients in MMF will remain on a liquid diet until the MMF is released.
Clinical follow-up
Clinical follow-up depends on the complexity of the surgery and whether the patient has any postoperative problems.
With patients having fracture patterns including periorbital trauma, issues to consider are the following:
- Globe position
- Double vision
- Other vision problems
Other issues to consider are:
- Facial deformity (including asymmetry)
- Sensory nerve compromise
- Problems of scar formation
Implant removal
Generally, orbital implant removal is not necessary except in the event of infection or exposure. Readmission may be indicated if the long-term stability of the orbital volume has not been maintained.
Oral hygiene
Tooth brushing and mouth washes should be prescribed and used at least twice a day to help sanitize the mouth. Gently brushing the teeth occurs with a soft toothbrush (dipped in warm water to make the bristles softer).
Special considerations for orbital fractures
Travel in commercial airlines is permitted following orbital fractures. Commercial airlines pressurize their cabins. Mild pain on descent may be noticed. However, flying in military aircraft should be avoided for a minimum of six weeks.
No scuba diving should be permitted for at least six weeks.













