Open reduction internal fixation
1. Principles
General considerations
Open reduction internal fixation (ORIF) is an option. As with most treatment options, the surgeon should plan on placing arch bars and using MMF. A full arch bar is placed and ligated to the teeth. Depending on the nature of the fracture, the surgeon may or may not choose to keep the patient in MMF postoperatively.
The first option is to perform an ORIF of the palatal fracture using one or more plates on the palate through an existing laceration.
Alternatively, locking screw/plate systems allow for transmucosal application of the internal fixation hardware. A second plate may be placed on the facial aspect of the alveolar segment, with care being taken not to injure the tooth roots.
A second option is to reduce the fracture and use a palatal splint.
A third option combines the first two options.
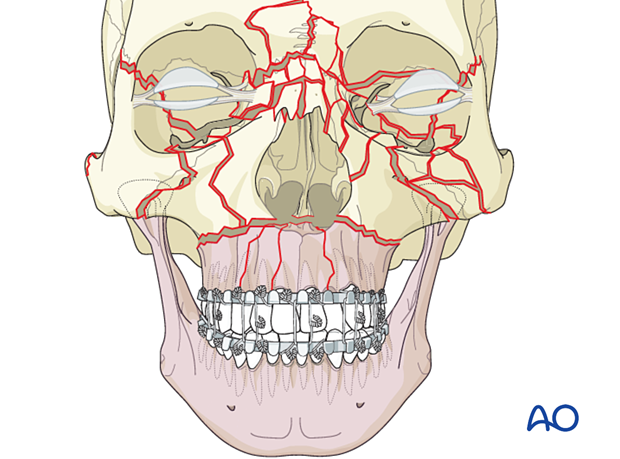
Panfacial trauma
In a panfacial trauma, the most typical situation where we see a palatal fracture, reestablishing the maxillomandibular unit should be a high priority. In such cases, a combination of ORIF and the use of palatal splints is common.
Teaching video
AO Teaching video on fixation of a complex midface fracture
2. Approach
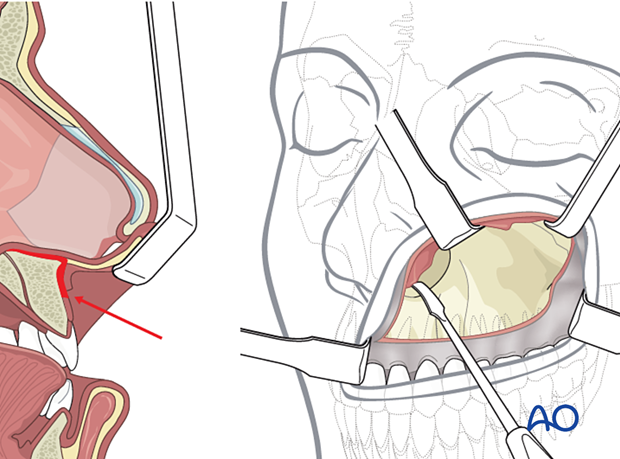
Standard approaches to the maxilla are used. However, if present, lacerations can be used for direct access to the fracture site.
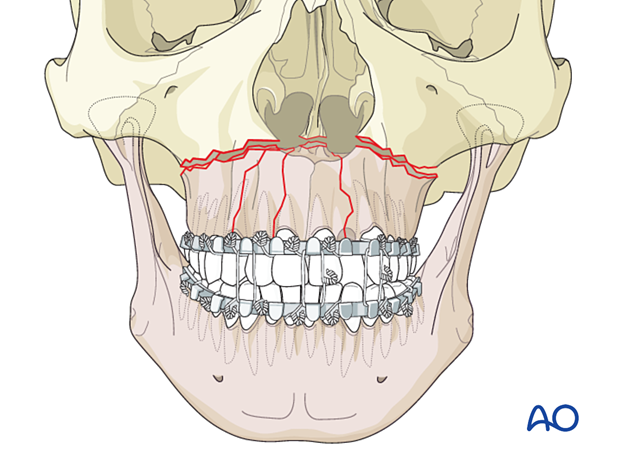
3. Reduction
Manual reduction
Perform the reduction by applying pressure laterally on the maxillary segments to reduce the splayed fracture.
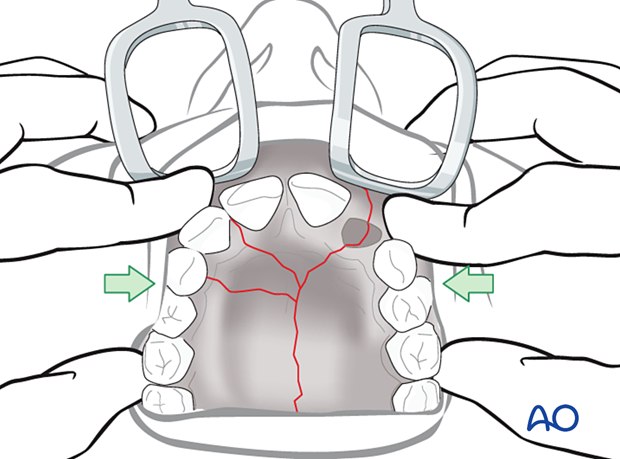
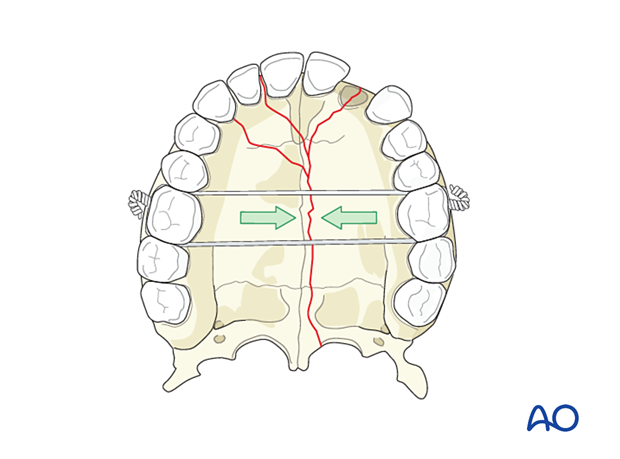
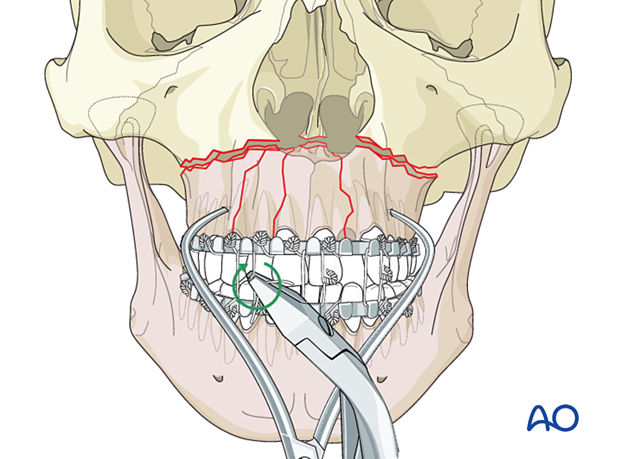
The reduction might be facilitated by placing a transpalatal wire to span the molars and compress the arch to eliminate the splaying and aid in the reduction of the fracture.
Apply MMF
Erich arch bars are applied, and the occlusion is checked. The occlusion is then secured by maxillomandibular fixation (MMF). Click here for a detailed description of the MMF technique.
4. Fixation
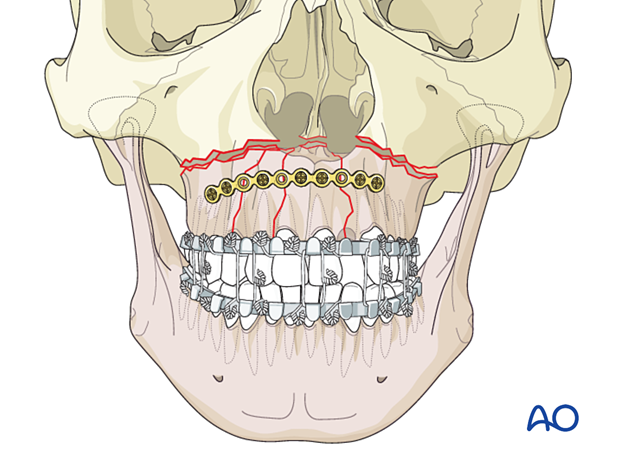
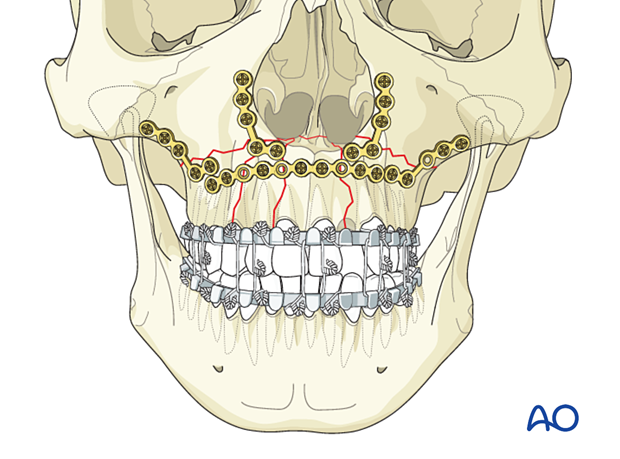
With multiple alveolar fractures, it may be necessary to place a longer bridging plate horizontally on the facial surface of the maxilla. An additional plate may be used on the palatal surface.
More information on CMF implants can be found here.
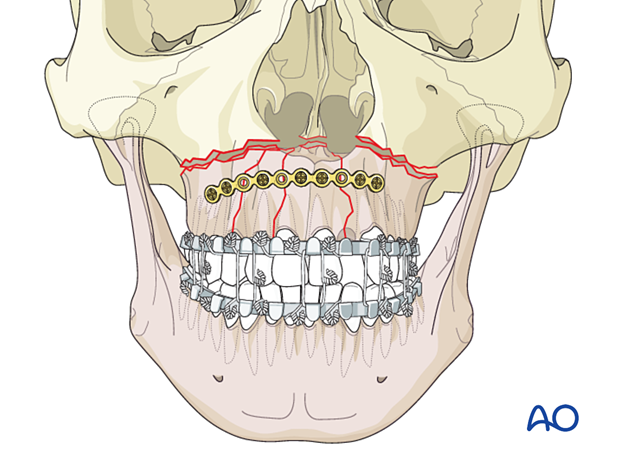
Plate application
Fixation should be considered in two planes. The first plane is the palate, which should be fixed with internal or transmucosal plates. The second plane is the facial aspect of the alveolar segment, where a plate is placed, avoiding injury to the tooth roots.
It may be desirable to plate the palate first while a perfect reduction of the previously splayed palate is visualized.
More information on CMF implants can be found here.
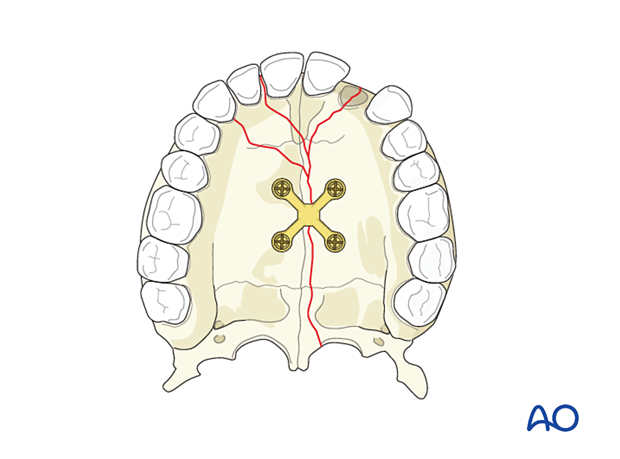
This illustration shows a straight plate placed on the bone or the mucosa with transmucosal screws.
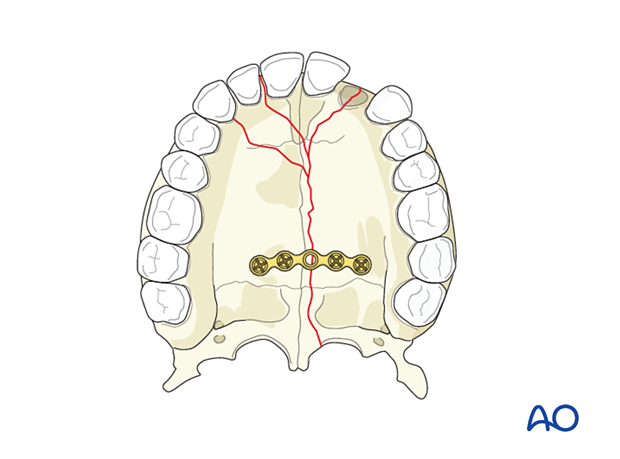
When possible, the use of an X plate provides good separate anterior and posterior fixation of the palatal fracture, as illustrated.
While placing the second plate on the anterior alveolar fracture, consider the position of additional plates to fix the Le Fort I fracture.
Care must be taken to avoid tooth roots.
Addressing the Le Fort I fracture
The Le Fort I fracture needs to be addressed after the palatal unit has been repaired. Please refer to the section on Le Fort fractures for further details.
5. Severely damaged or comminuted tooth-bone units
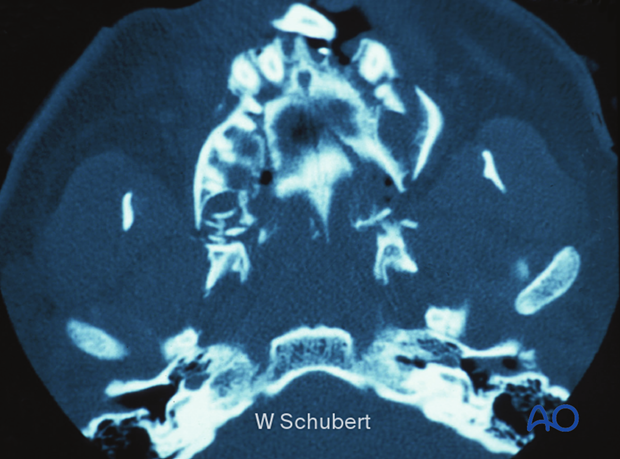
In this patient, the tooth-bone units are severely damaged or comminuted. The use of a palatal splint alone may not be adequate. An open technique with a horseshoe degloving palatal incision will allow successful fixation with multiple plates for these comminuted fragments.
6. Aftercare
Postoperative positioning
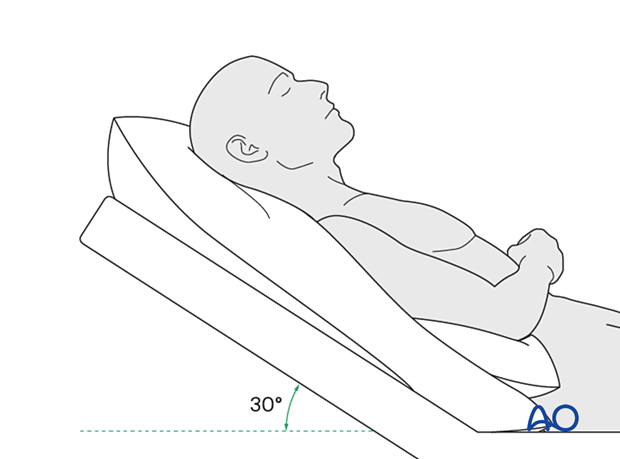
Keeping the patient’s head in an upright position both preoperatively and postoperatively may significantly reduce periorbital edema and pain.
Medication
The following medications may be used:
- Analgesia as necessary (no aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs) for seven days)
- In case of an open wound or exposed bone antibiotic coverage is indicated
- Regular perioral and oral wound care should include disinfectant mouth rinse, lip care, etc.
Postoperative imaging
Postoperative imaging should be performed within the first days after surgery. 3D imaging (CT, cone beam) is recommended to assess complex fracture reductions.
In fractures involving the alveolar area, orthopantomograms (OPG) are helpful.
Diet
Diet depends on the fracture pattern.
A soft (non-chew) diet can be taken as tolerated until there has been adequate healing (usually 4–6 weeks).
Patients in MMF will remain on a liquid diet until the MMF is released.
Clinical follow-up
Clinical follow-up depends on the complexity of the surgery and whether the patient has any postoperative problems.
Issues to consider with palatal fractures and alveolar ridge fractures include:
- Problems with dentition and dental sensation
- Problems with occlusion
- Problems with the temporomandibular joint (TMJ), such as reduced range of motion and pain
MMF
The need for and duration of MMF are very much dependent on:
- Fracture morphology
- Type and stability of fixation (including palatal splints)
- Dentition
- Coexistence of mandibular fractures
- Premorbid occlusion
Oral hygiene
Patients with arch bars, intraoral incisions, or wounds must be instructed about appropriate oral hygiene procedures. The presence of arch bars or elastics makes oral hygiene more complicated. A soft toothbrush (dipped in warm water to make it softer) should be used to clean the teeth and arch bars. Elastics are removed during oral hygiene procedures. Disinfectant mouth rinses (Chlorhexidine) should be prescribed and used at least three times a day to help sanitize the mouth.
For larger debris, a 1:1 mixture of hydrogen peroxide/Chlorhexidine can be used. The effervescent action of the hydrogen peroxide helps remove debris. A jet irrigator, (eg, Waterpik) is a handy tool to help remove debris from the wires. If used, care should be taken not to directly point the jet stream over intraoral incisions, which may lead to wound dehiscence.













