Open reduction internal fixation
1. Principles
Because NOE type I represents a noncomminuted fracture, the goal should be to achieve a good anatomical reduction of the frontal process of the maxilla and the piriform rim.
The fracture then requires internal fixation to maintain its proper position. This could include:
- 1-point fixation in the case of green-stick fractures at the frontal process of the maxilla
- 2-point fixation with lateral displacement of the fragment
- 3-point fixation if additional fixation at the infraorbital rim is required
Ideally, at least 2 points of fixation should be used to avoid changes in the position of the fragment.
The proper repositioning of the fragment and the medial canthal tendon is crucial to the final result.
Great care should be taken when placing plates anterior to the medial canthal ligament, as these may be visible through the thin overlying skin.
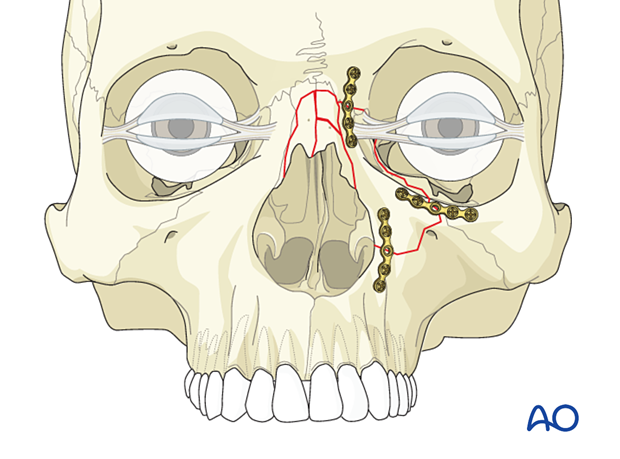
Nasal bone involvement
If the nasal bones are also fractured, they should be reduced.
2. Selection of approach
The most common access for reduction of NOE type I fractures includes the extended glabellar and the maxillary vestibular approaches. Existing lacerations can also be used. The lower eyelid transcutaneous or lower eyelid transconjunctival approaches may be used in cases of associated zygomatic fractures. For isolated unilateral NOE type I fractures, a coronal approach is usually not necessary.
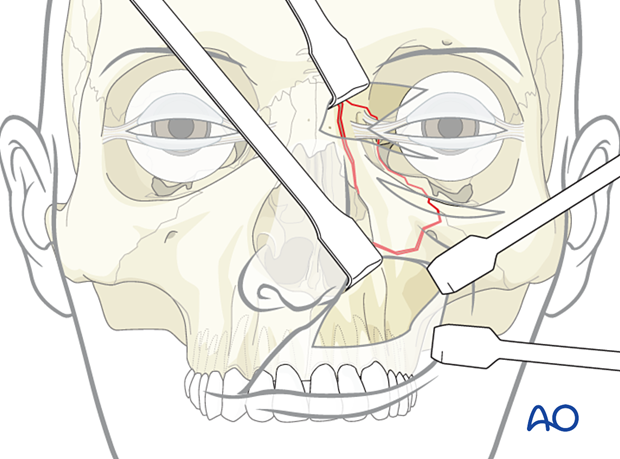
3. Reduction
NOE type I fractures are usually not difficult to reduce because they are not comminuted.
While visualizing the reduction of the bone fragment through one surgical approach, the surgeon must continually recheck the reduction through the other surgical approach(es) and digital palpation.
4. Fixation
General considerations
Displaced NOE type I fractures require internal fixation to maintain proper position. This could include 1-, 2-, or 3-point fixation.
NOE type I fractures that are hinged at the frontomaxillary suture (green stick), repositioning of the frontal process of the maxilla by rotating the infraorbital segment nasally may only require one point exposure and fixation at the piriform aperture via a maxillary vestibular incision.
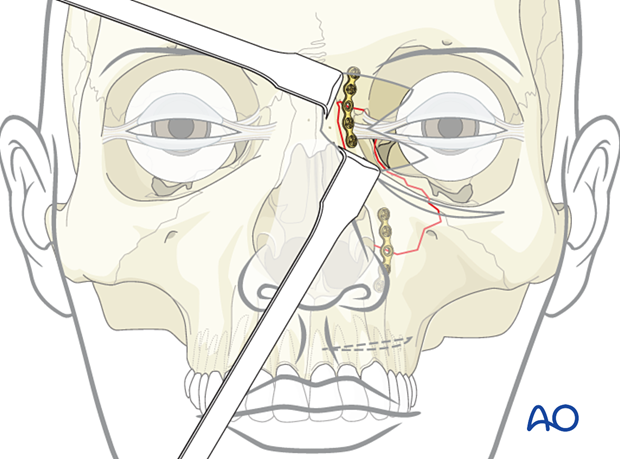
NOE type I fractures that require fixation at the frontomaxillary/frontonasal junction may require an extended glabellar approach or a transconjunctival approach with medial extension for fixation at this fracture site.
For isolated unilateral NOE type I fractures, a coronal approach is usually not necessary.
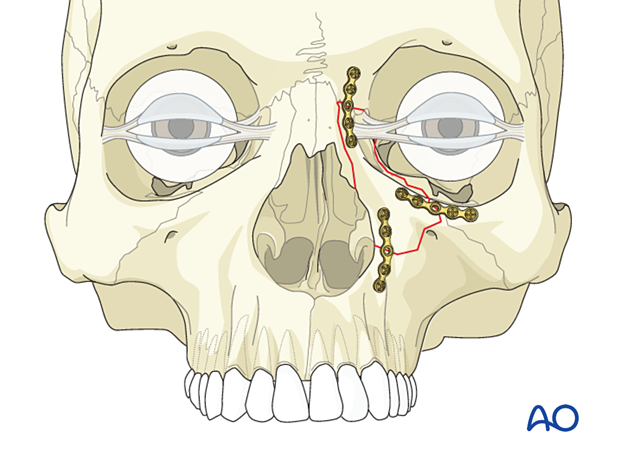
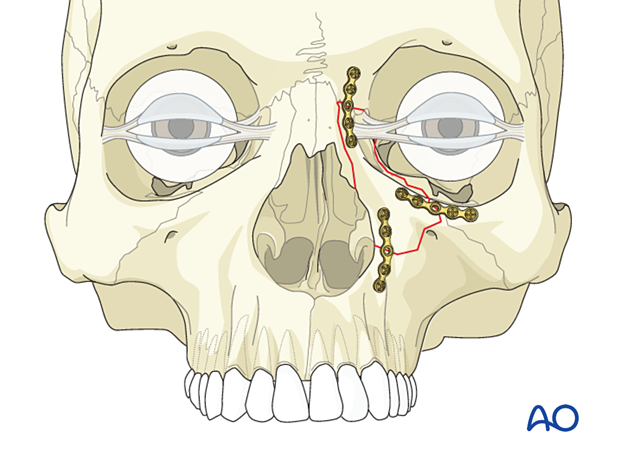
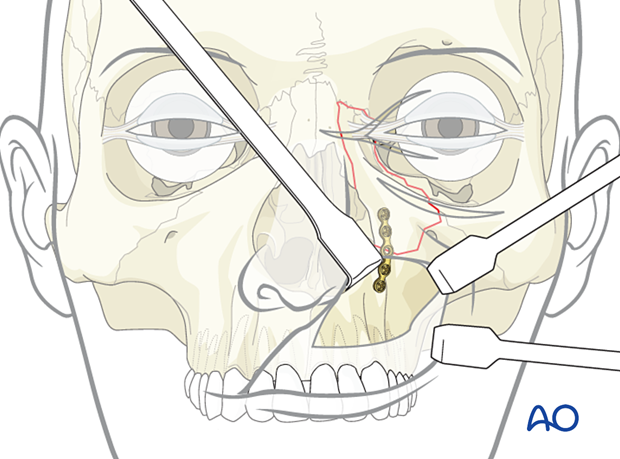
Placement of first plate
The first plate is generally placed inferiorly, along the piriform aperture, reducing and fixating the fractured fragment to the maxillary alveolus. This is performed through a vestibular incision.
In many cases, the bone fragment may be incompletely fractured (superiorly “hinged”). A 1-point fixation at the level of the piriform rim is often sufficient.
A right-angled clamp placed below the fractured segment in the piriform aperture can be used to lift it upwards to achieve a reduction. Alternatively, a “joystick” instrument (screw and forceps) can aid in the reduction of the fragment.
Placement of a second plate
If 2-point fixation is required, the second plate is placed at the frontonasal suture. A low-profile plate and screws should be used to ensure that the hardware is not visible under the thin skin.
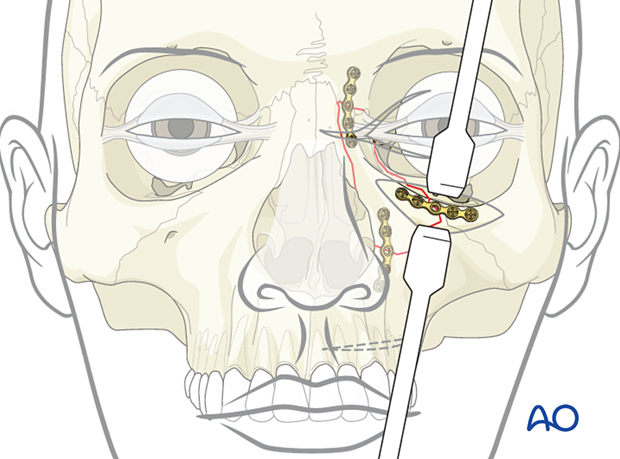
Placement of third plate (if necessary)
A third plate may be necessary on the orbital rim. In some cases, exploration and possible reconstruction of the medial wall and floor of the orbit may be necessary.
5. Soft tissues
Splinting
Adhesive strips are placed over the skin of the nasal dorsum, and the nasal bones are splinted using an external splint that conforms to the patient’s nose. If the nasal bones are comminuted or loose, they should be supported with an intranasal packing, which should be placed before placing the external splint.
If this technique is chosen, extreme caution is recommended. Patients will commonly have significant postoperative edema in this area; surgical incisions and lacerations can be present. If the splints are placed too tight, the patient is at risk of having skin necrosis in the medial canthal area.
This technique may be more relevant with the increased complexity of the NOE fractures. It may not be as applicable with a simple type I fracture with minimal degloving of the soft tissues from the bone in the medial canthal area. It may be more beneficial in type II and type III fractures where there has been more comminution associated with a greater need for degloving the soft tissues to achieve adequate reduction and fixation.
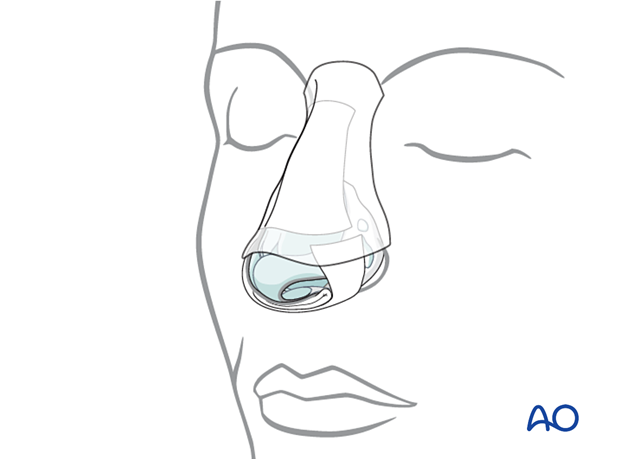
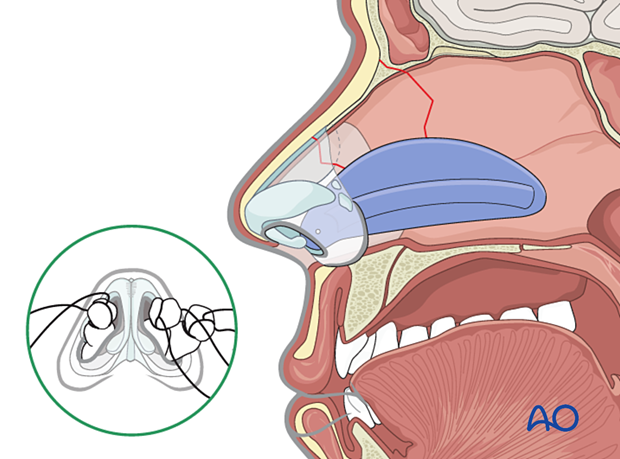
Nasal septum: Doyle splint
The nasal septum can be stabilized with splints (Doyle) or packs.
The Doyle splints are made from silicone and are placed on either side of the septum, secured by one or multiple sutures. They are designed to prevent the formation of a septal hematoma, splint septal cartilage, and maintain an open airway.
Removal of packs and splints
Packs used for control of acute bleeding can be removed after 24 hours.
Any packs supporting the nasal bones must be left in place for 5–7 days and as long as the external splint is in place.
The patient should be prescribed antibiotic treatment for as long as the nasal packs are in place.
6. Aftercare
Evaluation of the patient’s vision
Patient vision is evaluated on awakening from anesthesia and then at regular intervals until hospital discharge.
A swinging flashlight test may serve to confirm pupillary response to light in the unconscious or non-cooperative patient; alternatively, an electrophysiological examination must be performed but this is dependent on the appropriate equipment (VEP).
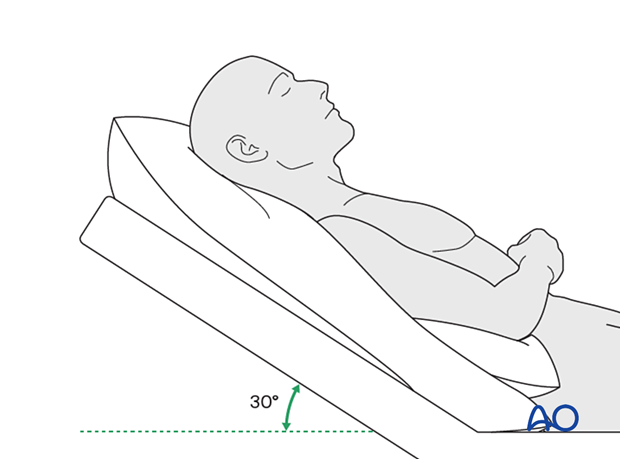
Postoperative positioning
Keeping the patient’s head in a raised position both preoperatively and postoperatively may significantly reduce edema and pain.
Nose blowing
Nose blowing should be avoided for at least ten days following fracture repair to prevent orbital emphysema.
Medication
The use of the following perioperative medication is controversial. There is little evidence to make solid recommendations for postoperative care.
- No aspirin for seven days (use of nonsteroidal anti-inflammatory drugs (NSAIDs)is controversial)
- Analgesia as necessary
- Antibiotics (Many surgeons use perioperative antibiotics.) There is no clear advantage of any antibiotic, and the recommended duration of treatment is debatable.
- A nasal decongestant may be helpful for symptomatic improvement in some patients.
- Steroids, in cases of severe orbital trauma, may help with postoperative edema. Some surgeons have noted increased complications with perioperative steroids.
- Ophthalmic ointment should follow local and approved protocol. This is not generally required in the case of periorbital edema. Some surgeons prefer it. Some ointments have been found to cause significant conjunctival irritation.
Postoperative imaging
Postoperative imaging must be performed during the first days after surgery. 3D imaging (CT, cone beam) is recommended to assess complex fracture reductions. An exception may be made for centers capable of intraoperative imaging.
Wound care
Ice packs are effective in the short term to minimize edema.
Remove the sutures from the skin after approximately five days if non-resorbable sutures have been used.
Avoid sun exposure and tanning to skin incisions for several months.
Diet
Diet depends on the fracture pattern and the patient’s condition, but there are usually no limitations.
Clinical follow-up
Clinical follow-up depends on the complexity of the surgery and whether the patient has any postoperative problems.In all patients with NOE trauma, all the following should be periodically assessed:
- Globe position
- Double vision
- Other vision problems
- Nasal airway status
Other issues to consider are:
- Facial deformity (including asymmetry and pseudo-telecanthus)
- Sensory nerve compromise
- Problems of scar formation
- Anosmia
- Epiphora and dacryocystitis
Implant removal
Generally, implant removal is not necessary except in the event of infection or exposure.
Special considerations
Travel in pressurized aircraft is permitted 4–6 weeks postoperatively. Mild pain on descent may be noticed. However, flying in a non-pressurized plane should be avoided for a minimum of 6 weeks.
No scuba diving should be permitted for at least 12 weeks. Additionally, the patient should be warned of potential long-term risks.













