Open reduction internal fixation
1. Principles
General considerations
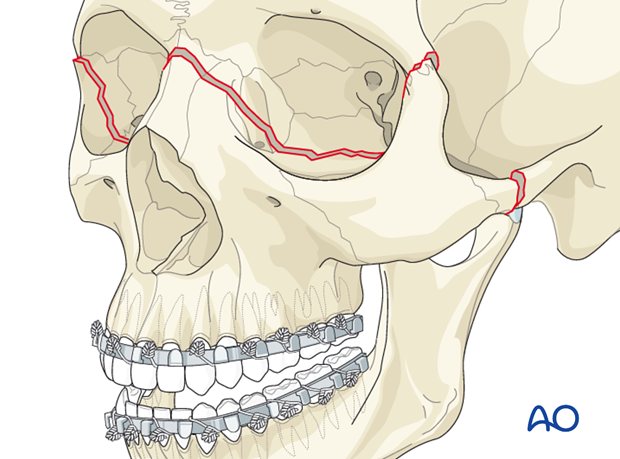
A Le Fort III fracture includes fracture of the nasofrontal junction, bilateral fractures through the area of the frontozygomatic suture, and probable fractures of the zygomatic arch. These fractures are also referred to as craniofacial dysjunction.
Considerations related to dental occlusion render nasotracheal intubation necessary. If that is not feasible, primary submental/submandibular intubation should be considered. Depending on the patient’s general condition, a tracheostomy might also be considered.
The aim of successful reconstruction of midface fractures is reestablishing the midfacial buttresses. These pillars can serve an even more important role in patients who lack dentition (partial or completely edentulous patients).
A principle in all Le Fort fractures is to reestablish the premorbid dental occlusion. Portions of the pterygoid plates and associated musculature are still attached to the posterior portion of the maxilla, so passive mobilization of the fracture can be difficult. Without passive mobilization, Class III tendency occurs often in the postoperative period. The reason for this is that when patients are placed into MMF during the surgery, the soft-tissue tension from the attached musculature distalizes the mandibular condyles in the glenoid fossae. When the MMF is removed, the condyles re-seat themselves into their normal position, bringing the mandibular dentition forward, creating a Class III malocclusion. In order to properly achieve a passive position of the maxilla, the maxilla requires strong mobilization forces using various instrumentation: Rowe’s disimpaction forceps, “Stromeyer” hook, Tessier retromaxillary mobilizers, etc.
The goal is to achieve an anatomical correct repositioning by means of 3-D reconstruction. If available, dental cast, stereolithographic models, and/or premorbid photographs may be useful guides for treatment.
As a general principle, all fractures should be exposed and reduced before plating.
Choice of implant
It is difficult to give absolute guidelines as to the strength of the plates to be used at the three key points of fixation for a Le Fort III fracture. There is considerable variability as to how unstable or comminuted the fractures may be. Furthermore, the majority of Le Fort III fractures are also associated with a plethora of other midface fractures. This has further impact on deciding the size and strength of the plate to be used. Finally, in many cases of Le Fort III fractures with other panfacial trauma, many surgeons may choose to leave the patient in MMF for a period of time postoperatively. This has a further impact in deciding whether a larger or smaller plate is adequate.
Older texts often recommended using a larger compression plate at the zygomaticofrontal suture. The soft-tissue coverage over this area is very thin, and patients are likely to complain if the plate is palpable. Furthermore, compression plating at this location is not necessary.
Generally, a smaller straight plate is adequate at the zygomaticofrontal area. A variety of different plates may be used at the nasofrontal area. Options include one or two straight plates, or various configurations of Y- or X-plates.
Click here for a description of implant options.
Orbital involvement
A Le Fort III fracture involves fractures of the internal orbit. If significant, these orbital fractures may be treated in the same way as other orbital fractures in this location. Click here for further details on the reconstruction of combined medial wall and orbital floor fractures.
Teaching video
AO Teaching video on fixation of a complex midface fracture
2. Choice of approach
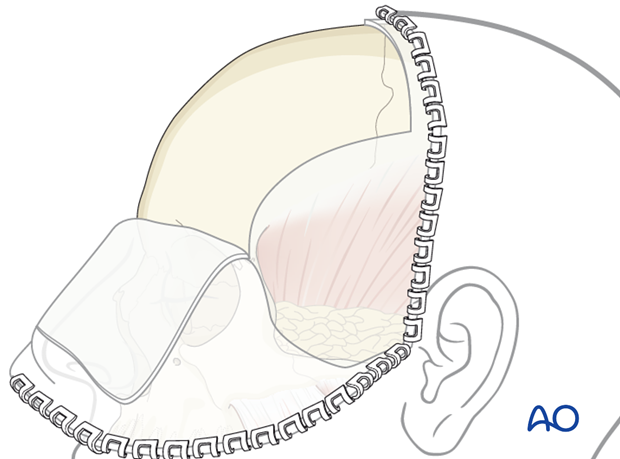
All of these fractures can be approached by coronal incision. A second option includes a combination of bilateral upper-eyelid incisions to treat the fracture at the frontozygomatic suture, combined with a glabellar incision to approach the nasofrontal area if the surgeon is confident regarding the reduction and chooses not to plate the zygomatic arch fractures.
A third option is to include a combination of upper-eyelid incisions, combined with a glabellar incision, combined with a preauricular approach to plate the zygomatic arch. This combination also avoids performing a coronal incision.
A glabellar incision may be particularly desirable in an elderly patient who commonly has frown lines in the area of the glabella, or in a patient who wears glasses, where the frame of the glasses may help to cover up the glabellar incision.
If present, existing lacerations may also be used. The ethmoidal approach is not recommend.
3. Reduction
Arch bars and mobilization
First, arch bars are secured to the dentition. Click here for a detailed description of mandibulomaxillary fixation.
After exposure of the fracture segments by adequate approaches, the fractures have to be mobilized to enable reduction and fixation.
Reduction instruments - Use of Rowe disimpaction forceps
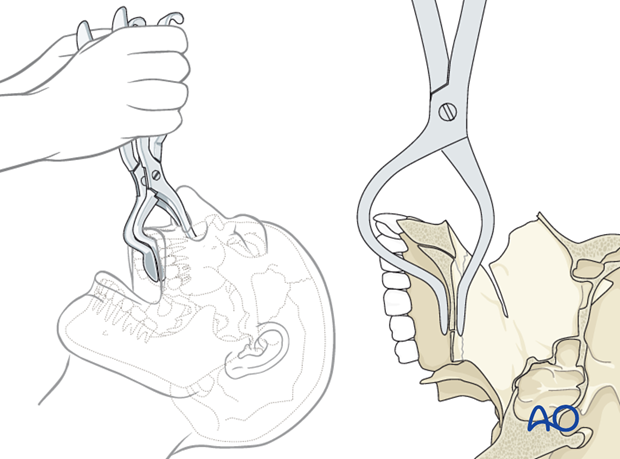
The Rowe disimpaction forces are side specific. They allow precise 3-D movement of fracture fragments of the centrally impacted midface or maxilla.
Note: Special attention has to be given to the patient’s individual fracture pattern so that the use of these instruments does not result in significant shearing at the skull base or orbit. Otherwise, severe complications such as blindness can occur.
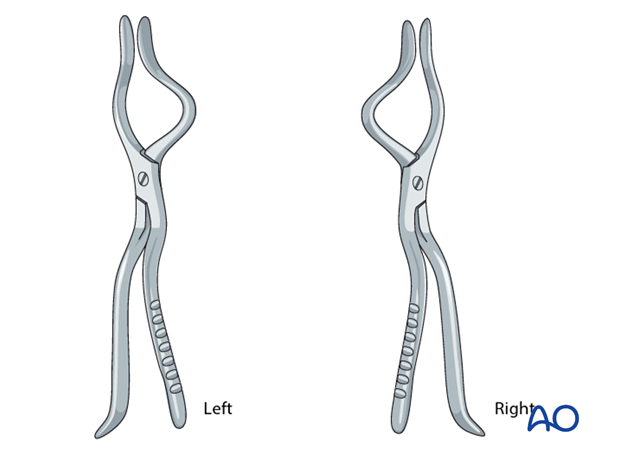
Special attention has to be paid regarding the correct placement of the Rowe disimpaction forceps so that the upper anterior dentition is not harmed.
The maxillary fracture is completely mobilized and an attempt should be made to make the fragment as passive as possible. This may require an up-down and side-to-side movement of the forceps.
Reduction instruments - Use of bone hooks
According to regional preferences and various schools of teaching, different bone hooks are used for fracture reduction in the lateral midfacial area.
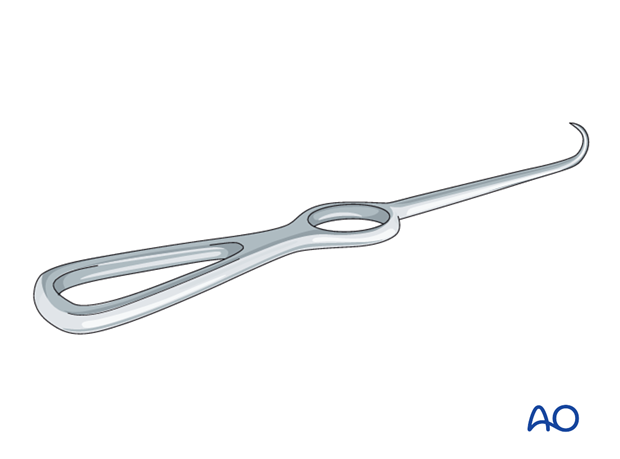
Reduction hook (Stromeyer hook)
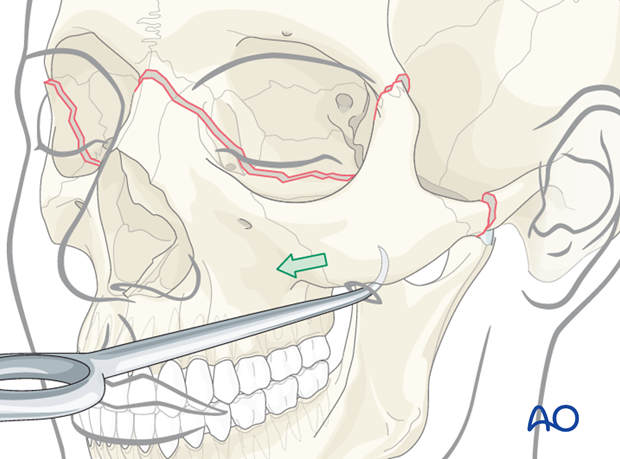
The Stromeyer hook (Georg Friederich Louis Stromeyer, Hannover, Germany, 1804-1876) is very versatile for transoral and transcutaneous reduction of lateral midfacial fractures. Its main indication is to reduce zygoma or zygomatic arch fractures.
In selected cases the Stromeyer hook can also be used for manipulating the Le Fort complex by hooking the tip of the instrument inside the piriform aperture and pulling downwards and anteriorly. This technique is called downfracture procedure in Le Fort osteotomies.
For zygoma reduction the tip of the Stromeyer hook is inserted transcutaneously. The curvature of the Stromeyer is held between the index finger and the thumb. The tip of the hook is then inserted about 4 cm below the lateral canthus either directly through the skin or following a limited stab incision.
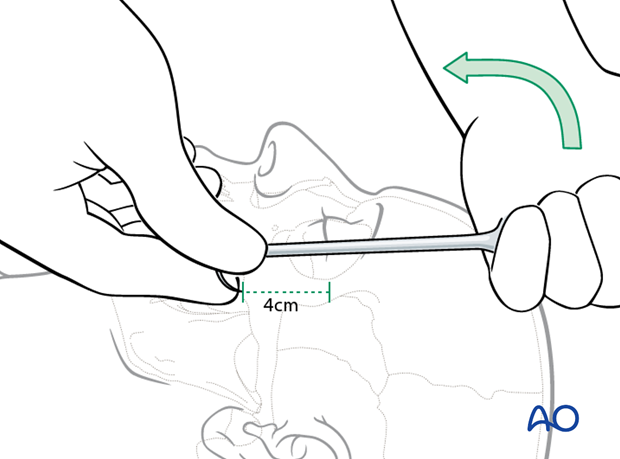
After controlled positioning of the instrument, the hook is placed below the fracture segment and reduction can be obtained by pulling in the necessary vector. Care has to be taken so that the direction of pull on the hook is not changed, causing dislocation of the hook which could result in injury to the orbit or soft tissues.
Reduction instruments - Use of threaded reduction tool
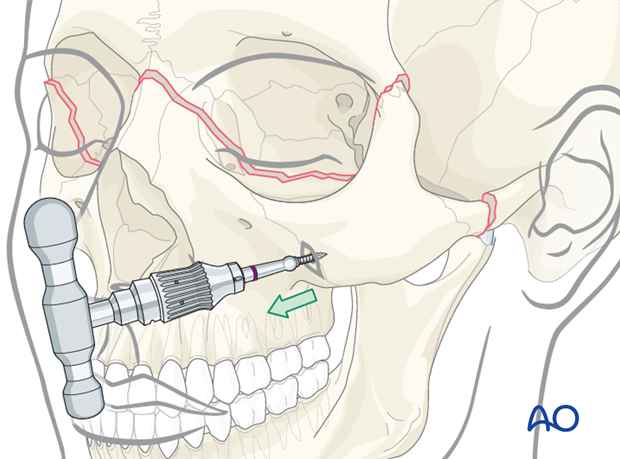
The threaded reduction tool (Carroll-Girard technique) might be helpful to 3-D position the midface.
The tip of the tool is self-drilling which generally requires no predrilling, but support of the mobile fragment is required to withstand the force resulting from the insertion of the instrument.
The T-handle allows excellent manipulation of a solid bony structure like the zygoma, in a Le Fort III fracture. Insertion of the threaded reduction tool is usually done after limited stab incision.
4. Fixation
General considerations
According to the quality and stability of the reduction, the final decision is made regarding the number of plates and screws, and the design of the plates.
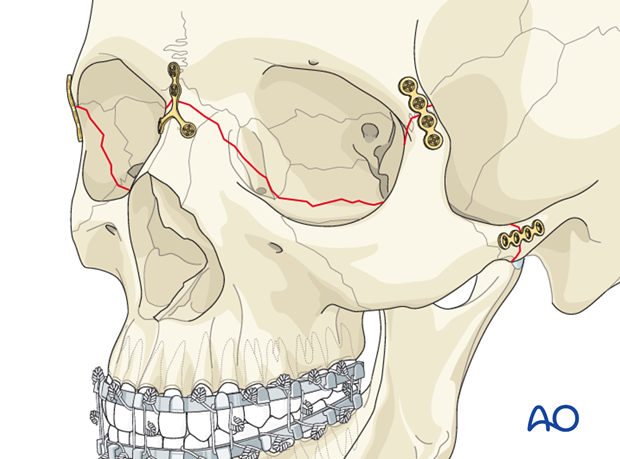
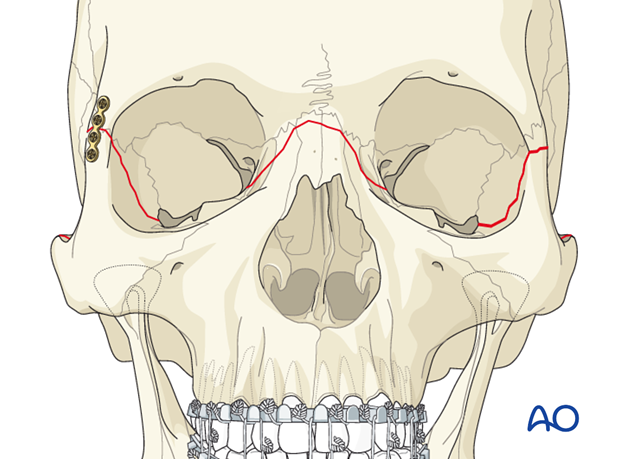
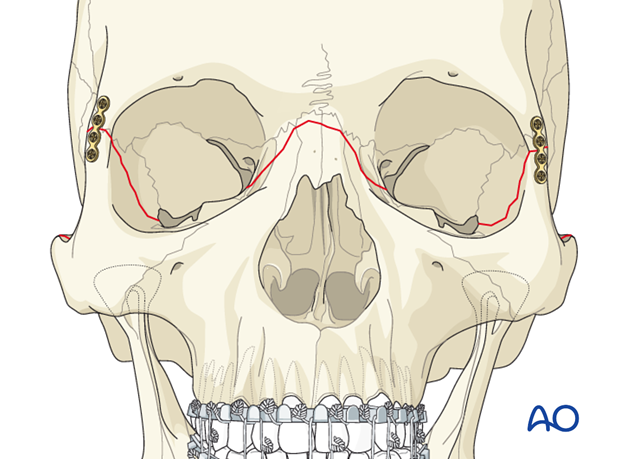
Generally, for Le Fort III fractures, plate fixation is applied to the fractures at the zygomatic arch, the frontozygomatic area, and the nasofrontal junction.
Fixation usually starts at the most reliably reduced buttress, always considering any fracture line in all three dimensions. If reduction is satisfactory, the first plate can be fixed by filling an adequate number of screws into the plate holes. Due to the specific patient injury patterns, provisional fixation with a limited number of screws may be indicated (in special cases, even temporary wire fixation might be considered). Final fixation must include two screws per fracture side.
The remaining buttresses are similarly addressed.
Complete reduction and fixation of the Le Fort fractures should take place before addressing the internal orbital wall fractures.
If there are any significant orbital fractures that require fixation or plating, these are performed after complete reduction and stabilization of the Le Fort III fracture.
First plate
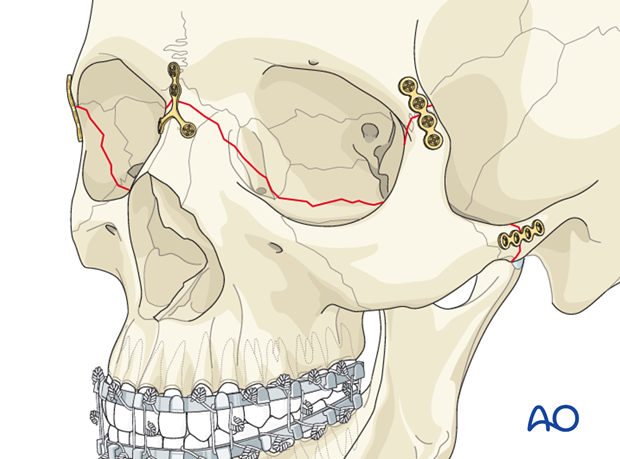
In the case shown, the first plate is applied to the right lateral orbital buttress. According to the fracture morphology, a plate of appropriate profile, shape, and length is selected and contoured using bending pliers.
The plate is positioned with appropriate instruments (eg, forceps, plate holders, gauze packer). The first hole is drilled (a drill bit with a stop may be used) next to the fracture line in the frontal process of the zygoma and a screw is inserted.
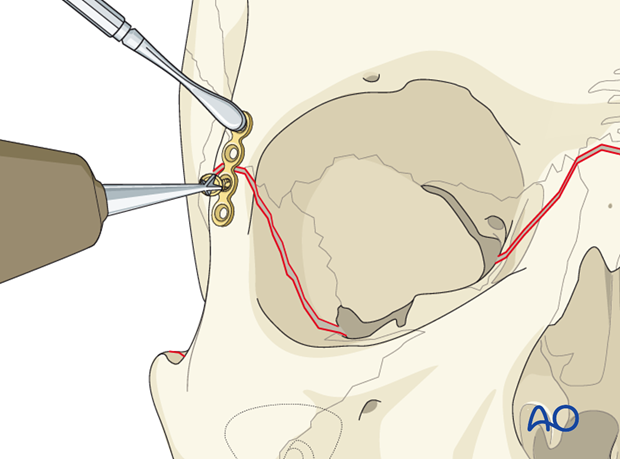
Second screw in first plate
After drilling, the second screw is inserted next to the fracture line on the opposite side of the fracture.
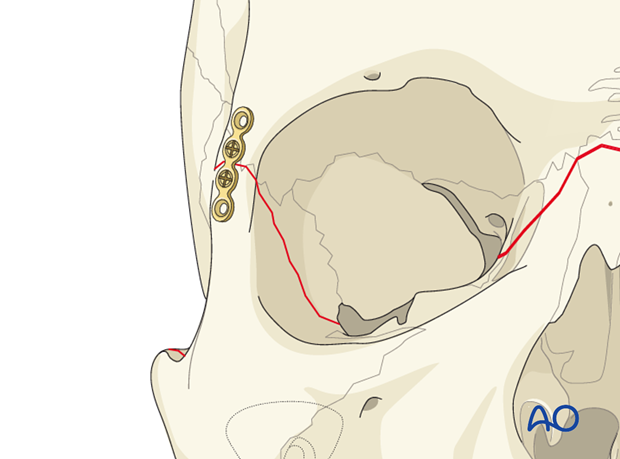
Insertion of remaining screws
If reduction is satisfactory at the other fracture lines, the remaining screws are inserted (at least two screws per fracture fragment).
Alternatively, these two screws can be inserted after all other plates have been applied.
Contralateral frontozygomatic buttress
In the illustrated case the contralateral frontozygomatic buttress is fixed in the same manner.
Additional plates (if required)
For isolated Le Fort III fractures, bilateral frontozygomatic fixation may be sufficient; more commonly, additional points of fixation are needed.
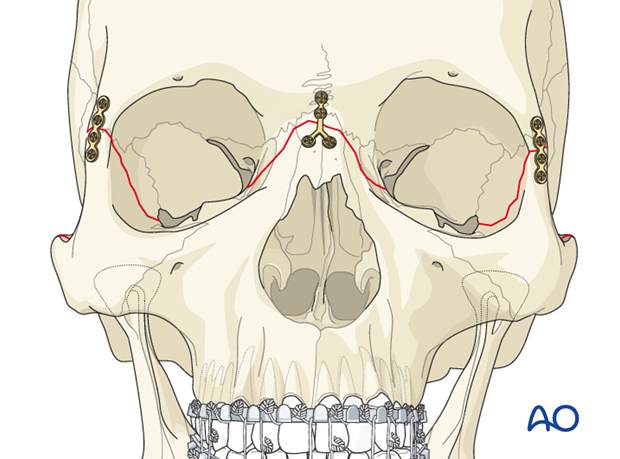
Nasofrontal plate(s)
Depending on the fracture pattern, one or two appropriate plates are applied. In this illustrated case, an inverted Y-plate is used for further reduction and stability at the nasofrontal fracture.
Zygomatic arch plate
If stability of the specific patient’s fracture morphology requires additional fixation, plates can be applied to the zygomatic arches in order to reestablish these sagittal buttresses.
Plate fixation normally uses straight plates. As with other fractures, at least two screws should be placed on each side of the fracture line, when possible. The number, length, and size of screws vary according to patient anatomy.
In case of a fracture of the zygomatic arch near the temporal bone, screw fixation (position screw or lag screw) may be considered. Care has to be taken to choose the correct implant dimension and length so that the neighboring structures are not harmed. The use of drill bits with a drill stop should be considered in this area.
Click here for further details – see “Options to consider for arch reconstruction”.
Check occlusion
After internal fixation has been completed, MMF is released and the occlusion checked.
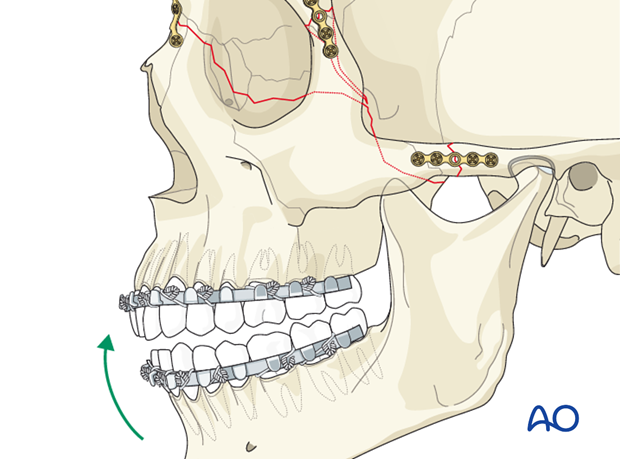
Pitfall: malocclusion
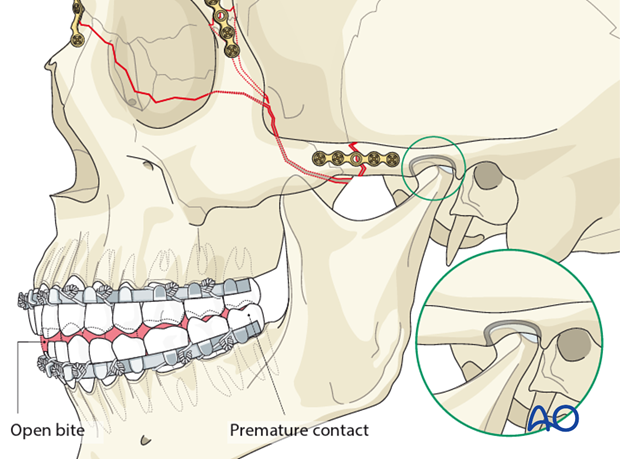
If an open bite and/or Class III tendency occurs when checking the occlusion, one or both mandibular condyles were malposed in posterior and/or inferior direction. In such cases, it is necessary to remove the bone plates, reapply MMF, and passively reposition the maxillomandibular complex again, assuring the condyles are properly seated. Bone plates are again applied and the occlusion verified.
The reason for a malocclusion may be the fact that the condylar heads were not positioned correctly in their respective glenoid fossae when securing MMF (as illustrated).
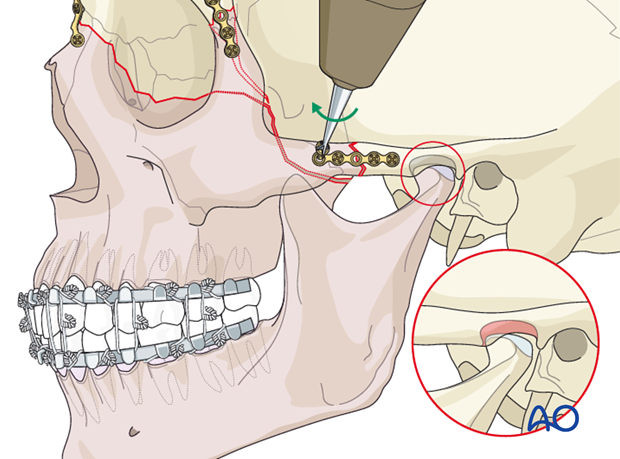
Illustration showing the subsequent malocclusion.
5. Aftercare following open reduction and internal fixation of Le Fort II and Le Fort III fractures
Evaluation of the patients vision is performed as soon as they are awakened from anesthesia and then at regular intervals until they are discharged from the hospital.
A swinging flashlight test may serve in the unconscious and/or noncooperative patient; alternatively electrophysiological examination has to be performed but is dependent on the appropriate equipment (VEP).
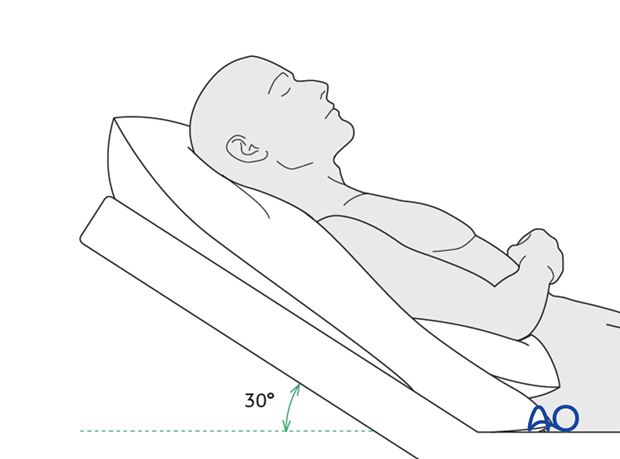
Postoperative positioning
Keeping the patient’s head in an upright position both preoperatively and postoperatively may significantly improve periorbital edema and pain.
Nose-blowing
To prevent orbital emphysema, nose-blowing should be avoided for at least 10 days following orbital fracture repair.
Medication
The use of the following perioperative medication is controversial. There is little evidence to make strong recommendations for postoperative care.
- No aspirin or nonsteroidal antiinflammatory drugs (NSAIDs) for 7 days
- Analgesia as necessary
- Antibiotics (many surgeons use perioperative antibiotics. There is no clear advantage of any one antibiotic, and the recommended duration of treatment is debatable.)
- Nasal decongestant may be helpful for symptomatic improvement in some patients.
- Steroids, in cases of severe orbital trauma, may help with postoperative edema. Some surgeons have noted increased complications with perioperative steroids.
- Ophthalmic ointment should follow local and approved protocol. This is not generally required in case of periorbital edema. Some surgeons prefer it. Some ointments have been found to cause significant conjunctival irritation.
- Regular perioral and oral wound care has to include disinfectant mouth rinse, lip care, etc.
Ophthalmological examination
Postoperative examination by an ophthalmologist may be requested. The following signs and symptoms are usually evaluated:
- Vision (except for alveolar ridge fracture, palatal fracture)
- Extraocular motion (motility) (except alveolar ridge fracture, palatal fracture)
- Diplopia (except Le Fort I, alveolar ridge fracture, palatal fracture)
- Globe position (except Le Fort I, alveolar ridge fracture, palatal fracture)
- Perimetric examination (except Le Fort I, alveolar ridge fracture, palatal fracture)
- Lid position
- If the patient complains of epiphora (tear overflow), the lacrimal duct must be checked.
Note: In case of postoperative double vision, ophthalmological assessment has to clarify the cause. Use of prism foils on existing glasses may be helpful as an early aid.
Postoperative imaging
Postoperative imaging has to be performed within the first days after surgery. 3-D imaging (CT, cone beam) is recommended to assess complex fracture reductions. An exception may be made for centers capable of intraoperative imaging.
Especially in fractures involving the alveolar area, orthopantomograms (OPG) are helpful.
Wound care
Remove sutures from skin after approximately 5 days if nonresorbable sutures have been used.
Apply ice packs (may be effective in a short term to minimize edema).
Avoid sun exposure and tanning to skin incisions for several months.
Diet
Diet depends on the fracture pattern.
Soft diet can be taken as tolerated until there has been adequate healing of the maxillary vestibular incision.
Intranasal feeding may be considered in cases with oral bone exposure and soft-tissue defects.
Patients in MMF will remain on a liquid diet until such time the MMF is released.
Clinical follow-up
Clinical follow-up depends on the complexity of the surgery, and whether the patient has any postoperative problems.
With patients having fracture patterns including periorbital trauma, issues to consider are the following:
- Globe position
- Double vision
- Other vision problems
Other issues to consider are:
- Facial deformity (incl. asymmetry)
- Sensory nerve compromise
- Problems of scar formation
Issues to consider with Le Fort fractures, palatal fractures and alveolar ridge fractures include:
- Problems of dentition and dental sensation
- Problems of occlusion
- Problems of the temporomandibular joint (TMJ), (lack of range of motion, pain)
Eye movement exercises
Following orbital fractures, eye movement exercises should be considered.
Implant removal
Implant removal is rarely required. It is possible that this may be requested by patients if the implant becomes palpable or visible. In some countries it will be more commonly requested. There have been cases where patients have complained of cold sensitivity in areas of plate placement. It is controversial whether this cold sensitivity is a result of the plate, a result of nerve injury from the original trauma, or from nerve injury due to trauma of the surgery. Issues of cold sensitivity generally improve or resolve with time without removal of the hardware.
Generally, orbital implant removal is not necessary except in the event of infection or exposure. Readmission might be indicated if long term stability of the orbital volume has not been maintained.
MMF
The duration and/or use of MMF is controversial and highly dependent on the particular patient and complexity of the trauma. In some cases where long-term MMF may be recommended, the surgeon may choose to leave the patient out of MMF immediately postoperatively because of concerns of edema, postoperative sedation, and airway. In these cases the surgeon may choose to place the patient in MMF after these concerns have been resolved.
The need and duration of MMF is very much dependent on:
- Fracture morphology
- Type and stability of fixation (including palatal splints)
- Dentition
- Coexistence of mandibular fractures
- Premorbid occlusion
Oral hygiene
Patients with arch bars and/or intraoral incisions and/or wounds must be instructed in appropriate oral hygiene procedures. The presence of the arch bars or elastics makes this a more difficult procedure. A soft toothbrush (dipped in warm water to make it softer) should be used to clean the surfaces of the teeth and arch bars. Elastics are removed for oral hygiene procedures. Chlorhexidine oral rinses should be prescribed and used at least 3 times a day to help sanitize the mouth.
For larger debris, a 1:1 mixture of hydrogen peroxide/chlorhexidine can be used. The bubbling action of the hydrogen peroxide helps remove debris. A Waterpik® is a very useful tool to help remove debris from the wires. If a Waterpik is used, care should be taken not to direct the jet stream directly over intraoral incisions as this may lead to wound dehiscence.
Follow-up
The patient needs to be examined and reassessed regularly and often. Additionally, ophthalmological, ENT, and neurological/neurosurgical examination may be necessary. If any clinical signs for meningitis or mental disturbances develop, professional help has to be sought. A regular follow-up CT scan is recommended 3-6 months after the trauma to assure proper pneumatization of the sinuses (particularly, mucocele formation has to be ruled out), sealing of the skull base and stability of fragment position.
Note: Posttrauma meningitis can occur even decades following trauma.
Special considerations for orbital fractures
Travel in commercial airlines is permitted following orbital fractures. Commercial airlines pressurize their cabins. Mild pain on descent may be noticed. However, flying in military aircraft should be avoided for a minimum of six weeks.
No scuba diving should be permitted for at least six weeks.












