Open reduction internal fixation
1. Principles
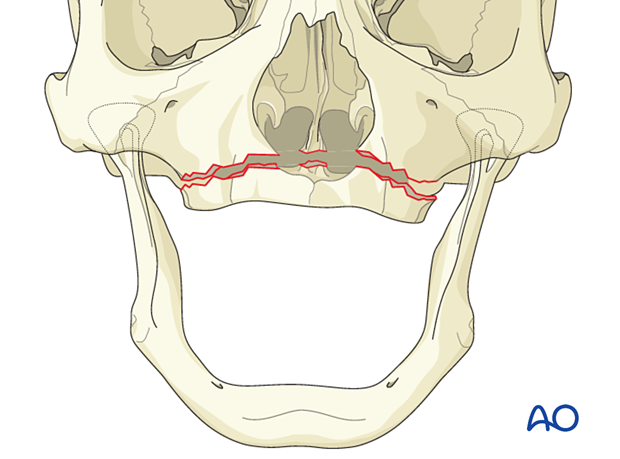
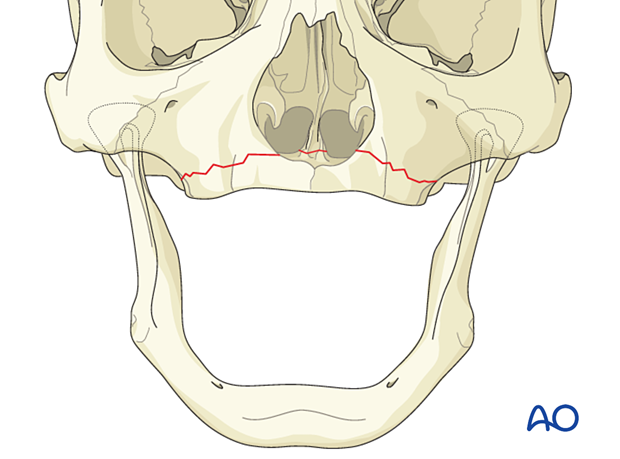
Edentulous Le Fort I fractures are rare. If they occur, the fracture is usually linear.
It is not possible to establish a definite occlusal relationship.
These fractures are typically treated by using bone plates after osseous reduction.
Significant displacement of an edentulous maxilla occurs into the nose and may encroach on the nasal airway. The maxillary ridge disappears into the nose making denture retention challenging.
More information regarding the choice of implants can be found here.
Teaching video
AO Teaching video on fixation of a complex midface fracture
2. Approach
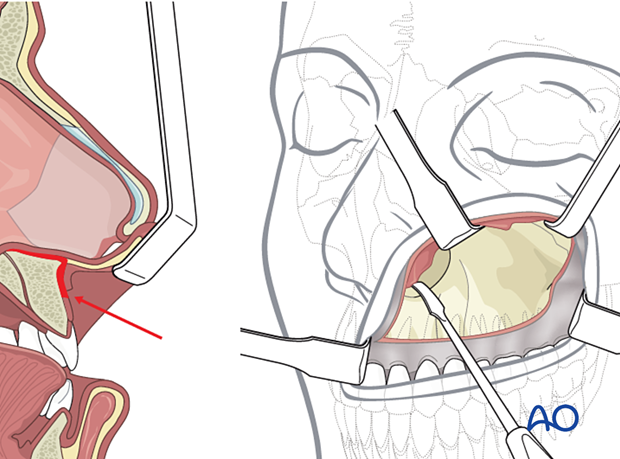
For this procedure, standard approaches to the maxilla are used. However, if present, lacerations can be used to access the fracture site for direct fracture management. The presence of significant intraoral lacerations may require rethinking and redesigning the incision in order to avoid devascularization of the bone or compromise of the soft tissue.
3. Reduction
Fracture reduction
In the case of a displaced maxillary complex, the fracture must be reduced first. This can be done manually by osteotomy or assisted by the use of reduction forceps. Frequently osteotomy is preferred to complete the fracture.
Reduction instruments
Rowe disimpaction forcepsThe Rowe disimpaction forceps are side-specific. They allow the application of significant amounts of force to disimpact and reposition the maxilla and midface.
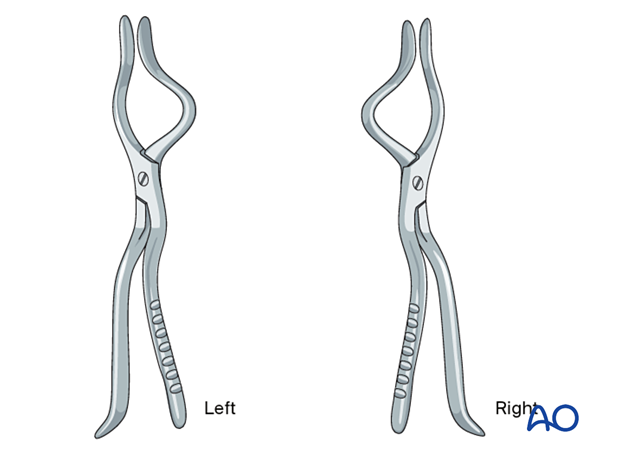
It should be noted that in cases of incomplete fracture many surgeons prefer to complete the fracture at the Le Fort I osteotomy level as a safer maneuver than using Rowe forceps for forced disimpaction.
If Rowe forceps are utilized, special attention must be paid to the correct placement of the forceps so that the upper anterior dentition is not harmed.
The maxillary fracture must be completely mobilized to allow for free repositioning.
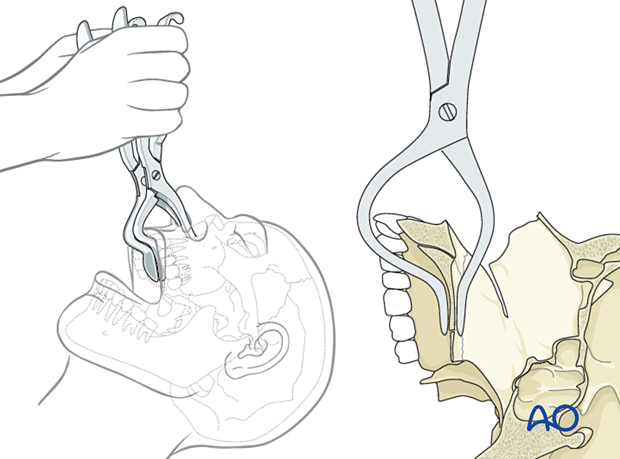
According to regional preferences and various schools of teaching, different bone hooks may be used for fracture mobilization and reduction. In general, they are all inferior to completion of the fracture with a Le Fort I osteotomy.
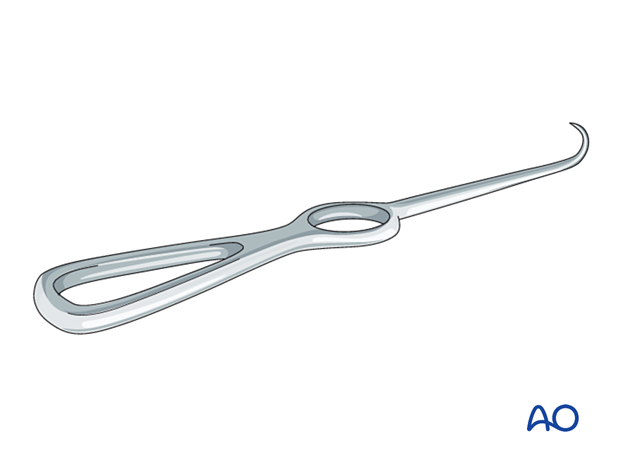
The Stromeyer hook is very versatile for the transoral reduction of Le Fort fractures.
In selected cases, the Stromeyer hook can also be used to manipulate the Le Fort complex by hooking the tip of the instrument inside the piriform aperture and pulling it downwards and forwards. This technique is sometimes referred to as the “downfracture procedure” in Le Fort osteotomies.
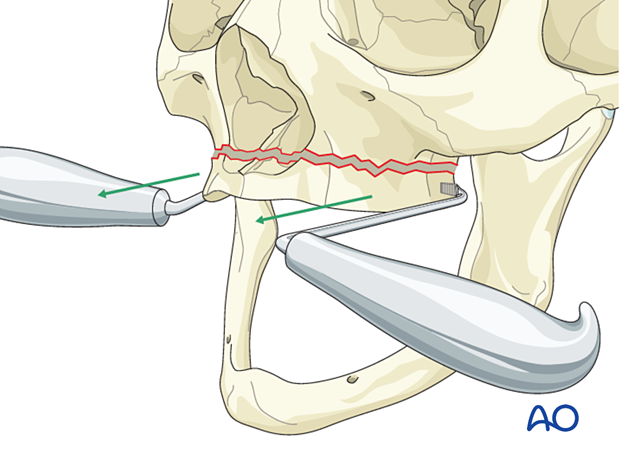
The Tessier retromaxillary mobilizers are placed behind the maxillary tuberosities to help mobilize a posteriorly displaced and impacted maxilla, facilitating passive repositioning and a normal occlusion. The repositioned maxilla must be passive to ensure that it remains in the correct position.
Confirm proper reduction
Confirm proper reduction by assessing bone alignment at the piriform aperture (nasomaxillary buttress) and the zygomaticomaxillary buttress.
4. Fixation
Plating
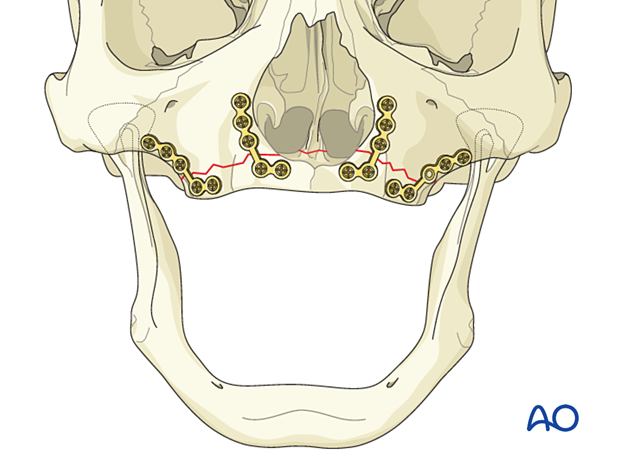
Two plates are often not enough to prevent rotation and displacement of the maxilla which rotates around the single side point of fixation.
Four L-plates are shown in the illustration.
Posttraumatic care
Hardware removal may be required in the future to facilitate the wearing of a removable denture or the placement of dental implants.
5. Aftercare
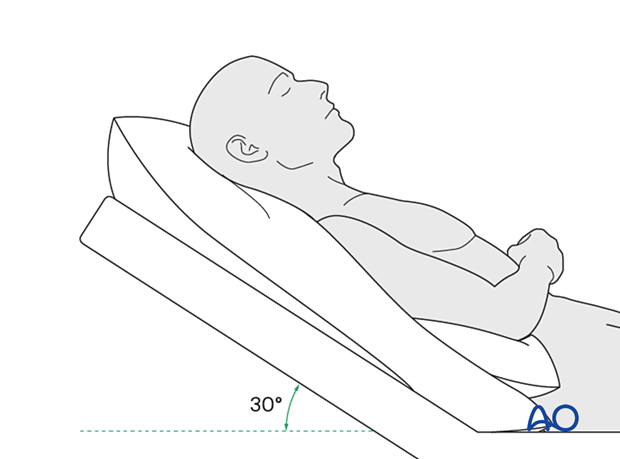
Postoperative positioning
Keeping the patient’s head in an upright position both preoperatively and postoperatively may significantly reduce periorbital edema and pain.
Medication
The following medications may be used:
- Analgesia as necessary (no aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs) for seven days)
- In case of an open wound or exposed bone antibiotic coverage is indicated
- Regular perioral and oral wound care should include disinfectant mouth rinse, lip care, etc.
Postoperative imaging
Postoperative imaging may be considered if further confirmation of alignment is desired. 2D and 3D imaging (CT, cone beam) are recommended to assess complex fracture reductions. An exception may be made for centers capable of intraoperative imaging.
In fractures involving the alveolar area, orthopantomograms (OPG) are helpful.
Diet
Diet depends on the fracture pattern.
A soft (non-chew) diet can be taken as tolerated until there has been adequate healing (usually 4–6 weeks).
Patients in MMF will remain on a liquid diet until the MMF is released.
Clinical follow-up
Clinical follow-up depends on the complexity of the surgery and whether the patient has any postoperative problems.
Issues to consider with palatal fractures and alveolar ridge fractures include:
- Problems with dentition and dental sensation
- Problems with occlusion
- Problems with the temporomandibular joint (TMJ), such as reduced range of motion and pain
MMF
The need for and duration of MMF are very much dependent on:
- Fracture morphology
- Type and stability of fixation (including palatal splints)
- Dentition
- Coexistence of mandibular fractures
- Premorbid occlusion
Oral hygiene
Patients with arch bars, intraoral incisions, or wounds must be instructed about appropriate oral hygiene procedures. The presence of arch bars or elastics makes oral hygiene more complicated. A soft toothbrush (dipped in warm water to make it softer) should be used to clean the teeth and arch bars. Elastics are removed during oral hygiene procedures. Disinfectant mouth rinses (Chlorhexidine) should be prescribed and used at least three times a day to help sanitize the mouth.
For larger debris, a 1:1 mixture of hydrogen peroxide/Chlorhexidine can be used. The effervescent action of the hydrogen peroxide helps remove debris. A jet irrigator, (eg, Waterpik) is a handy tool to help remove debris from the wires. If used, care should be taken not to directly point the jet stream over intraoral incisions, which may lead to wound dehiscence.













