ORIF, wire
1. Introduction
Principles
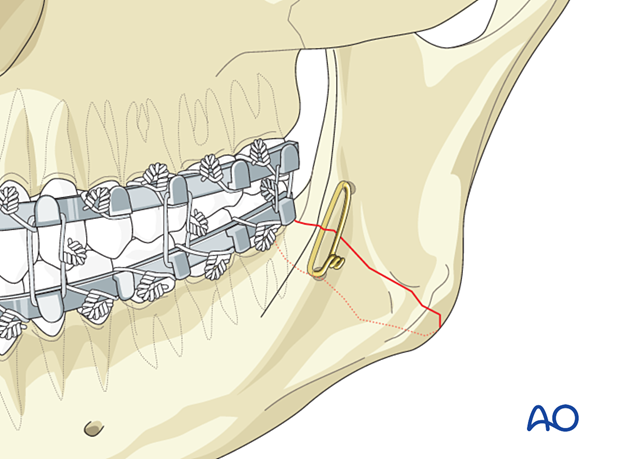
The intraosseous wire must be placed to resist the superior and clockwise rotation of the proximal fragment. Therefore, it is prudent to place the hole through the proximal fragment superiorly to the distal fragment hole.
The intraosseous wire does not need to engage both buccal and lingual cortices on each side of the fracture. It is only necessary to engage the buccal cortices with the wire.
Because this is a nonrigid technique, 5–6 weeks of MMF must be applied after surgery.
Special considerations
The following special considerations may need to be considered:
2. Patient preparation
This procedure is typically performed with the patient placed in a supine position.
3. Approach
For this procedure, the transoral approach to the angle is typically used.
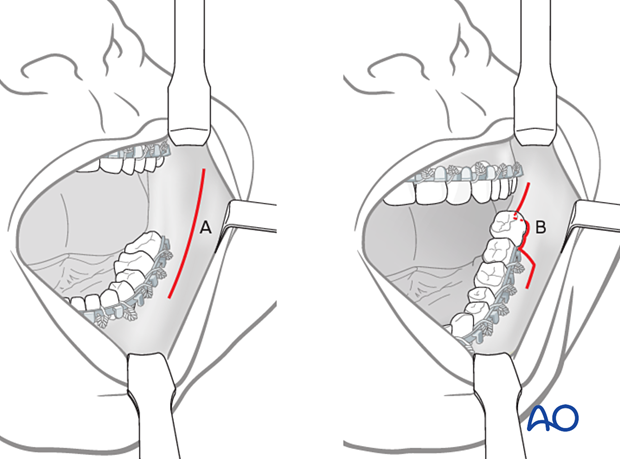
Depending on whether or not a third molar is to be extracted, there are two surgical approaches.
When there is no third molar present, or where one is present but is to be left in place, a purely vestibular incision approximately 5 mm away from the attached gingiva is made (A).
When an erupted the third molar is removed, the incision must incorporate the attached gingiva around the tooth's buccal side (B, the combination of vestibular and envelope incisions).
4. Fixation
Exposure of fracture
The fracture should be exposed, and any extractions determined necessary to be performed. Open reduction in dentate patients usually begins with fixation of the occlusion. However, MMF is not desirable when using intraosseous wire fixation until the wire is to be tightened. It is easier to drill the holes in the bone and pass the wire while the patient’s jaws are open.
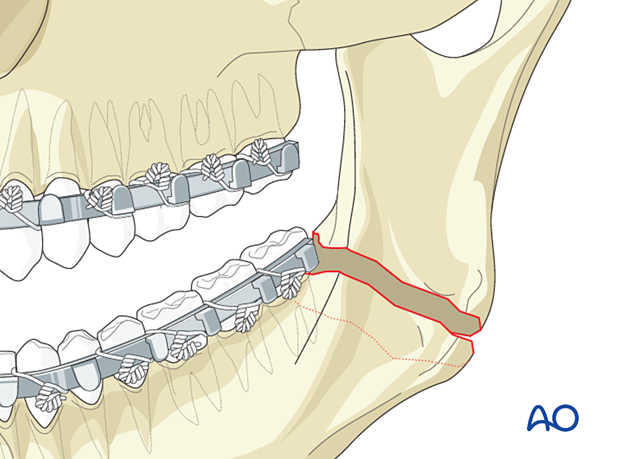
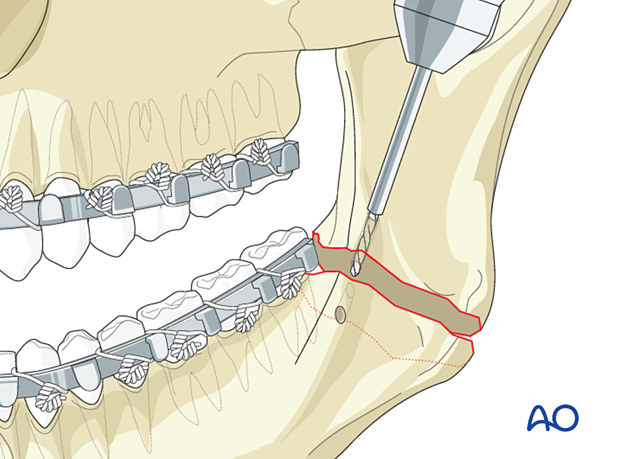
Drill holes
A 1.5 mm hole is drilled through the buccal cortex of the distal fragment. A second hole, located more superiorly, is drilled through the buccal cortex of the proximal fragment.
The holes need to be made a minimum of 5 mm from the fracture line.
The holes can be drilled with a drill inserted through the oral cavity, or a Steinmann pin can be inserted transcutaneously to drill the holes.
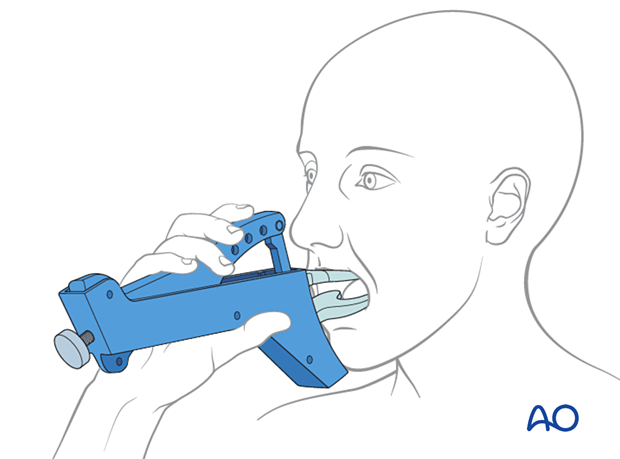
If needed, transbuccal instrumentation can be used to drill the holes.
If the terminal molar is extracted as part of the procedure, the holes enter the socket. If no tooth is extracted, the holes enter the medullary space and exit into the fracture.
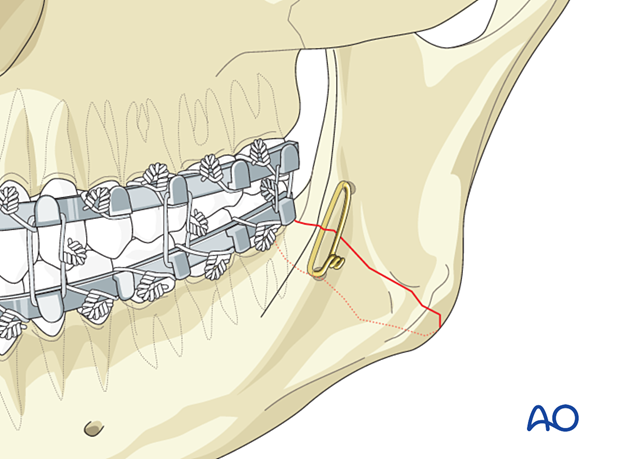
Applying internal wire fixation
A 0.5 mm wire (24 gauge) is passed through the holes and preliminarily twisted together. Before final tightening of the wire, the patient must be placed into occlusion and secured with MMF. The intraosseous wire is then tightened, cut, and bent down to the bone.
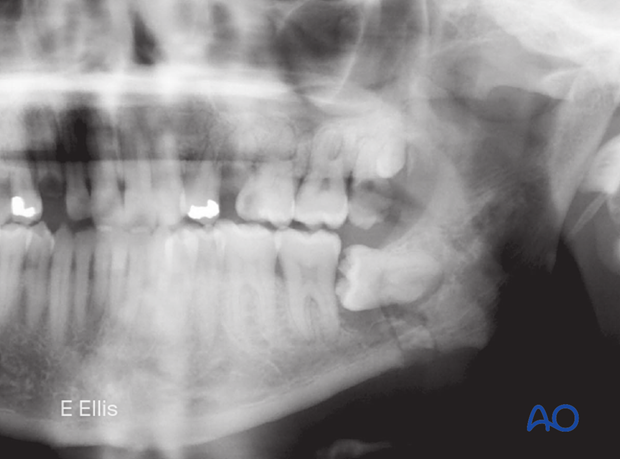
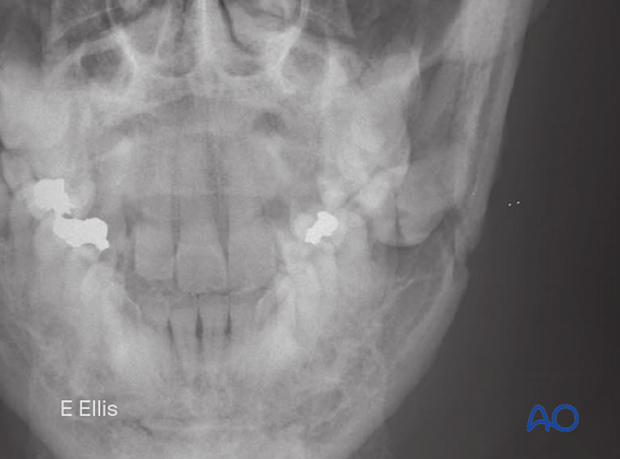
Panoramic and PA x-rays show a left simple angle fracture associated with an impacted third molar.
The standard care for this type of fracture is the use of internal fixation hardware (plates and screws). When plates and screws are not available, wire fixation may be considered.
This case will illustrate the use of a wire in the open reduction and fixation of an angle fracture.
PA view of the same case.
Because it is anticipated that the second molar might be removed in addition to the third molar, the soft-tissue incision is made as demonstrated.
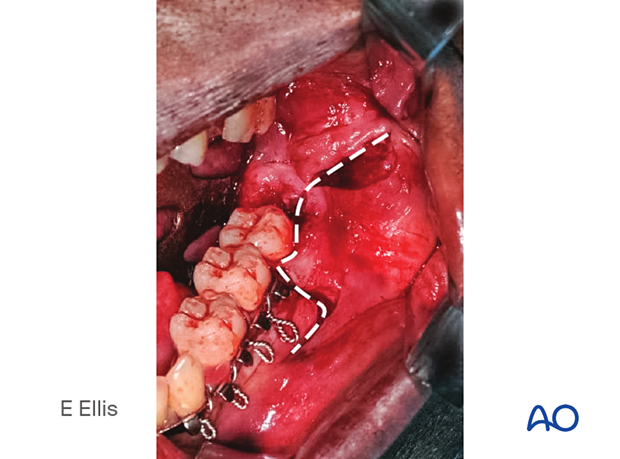
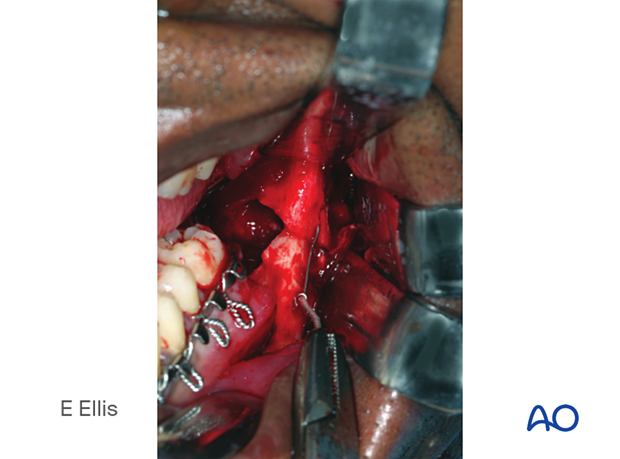
Subperiosteal dissection exposes the fracture and the impacted third molar.
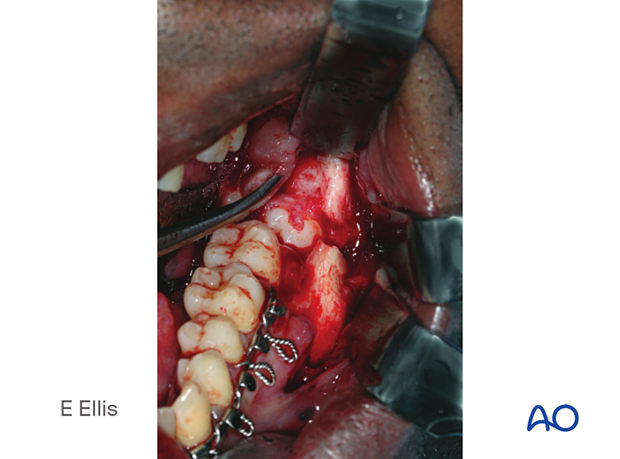
The impacted third molar is being removed because it interfered with fracture reduction.

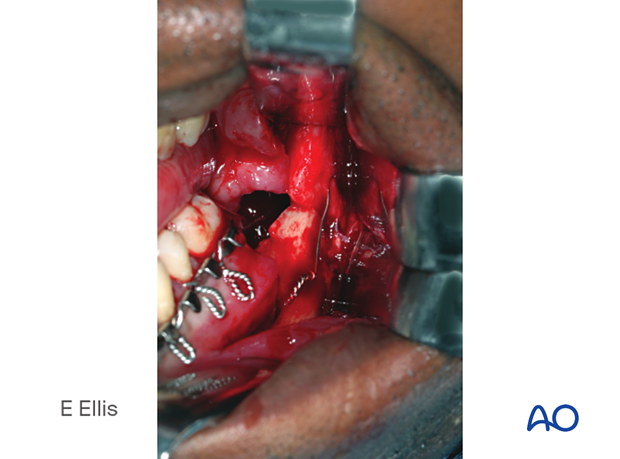
The second molar is also removed because there is a large bony defect along the posterior root.

After making two holes, the wire is then passed from the extraction site out the hole in the proximal fragment.
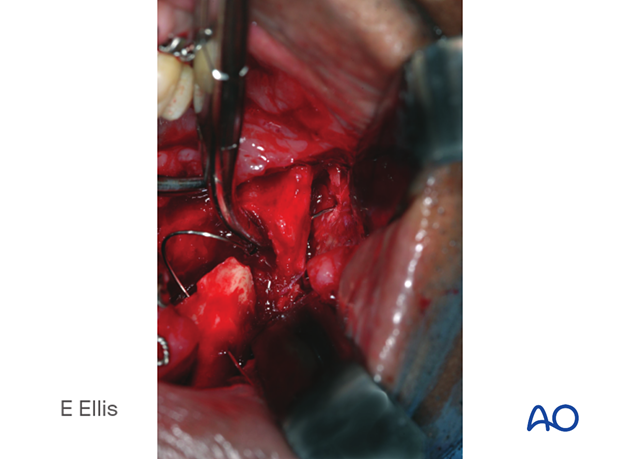
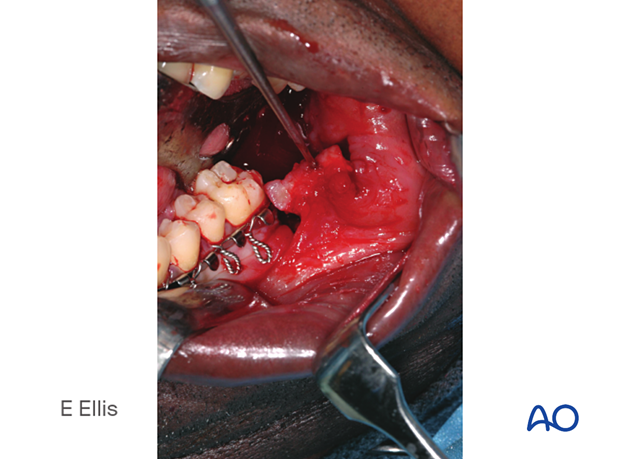
The wire is then preliminarily tightened. Before final tightening, the patient should be placed into MMF.
The wire has been tightened, cut, and bent down to lay against the bone
The flap is undermined with scissors to facilitate closure over the second molar extraction site.

Note that the flap has now been mobilized.
The flap has been closed over the extraction sites.
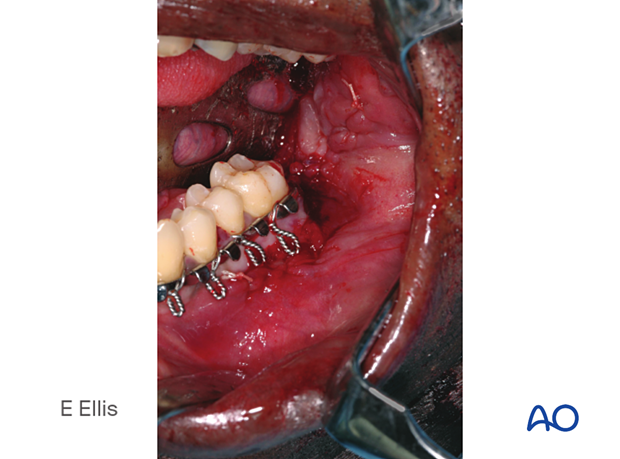
MMF is secured and left in position for 5–6 weeks. Note this patient’s preexisting malocclusion.

Postoperative panoramic and PA x-rays show the reduction of the fracture, position of the intraosseous wire, and MMF.
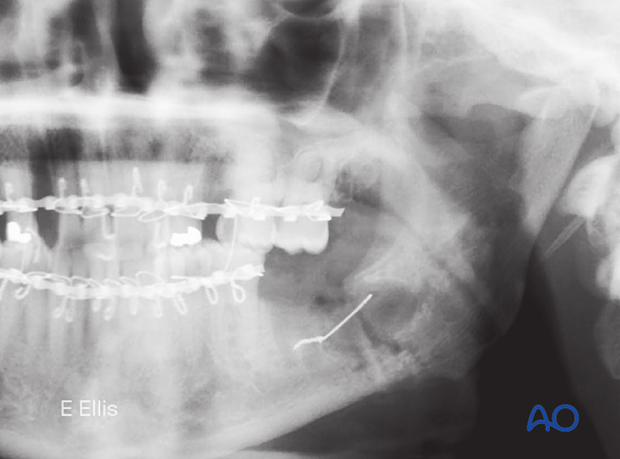
PA view of the same case.

5. Aftercare following ORIF of mandibular symphysis, body, angle, and ramus fractures
Use of jaw bra
If significant degloving of the soft tissues of the mandible has occurred, there may be a consideration for using a jaw bra or similar support dressing.
Arch bars
If arch bars or MMF screws are used intraoperatively, they are usually removed at the conclusion of surgery if proper fracture reduction and fixation have been achieved. Arch bars may be maintained postoperatively if functional therapy is required or if required as part of the fixation.
X-Rays
Postoperative x-rays are taken within the first days after surgery. In an uneventful course, follow-up x-rays are taken after 4–6 weeks.
Follow up
The patient is examined approximately 1 week postoperatively and periodically thereafter to assess the stability of the occlusion and to check for infection of the surgical wound. During each visit, the surgeon must evaluate the patient's ability to perform adequate oral hygiene and wound care and provide additional instructions if necessary. Many patients need to be seen regularly for replacement of their intermaxillary elastics and to encourage range of motion in their TMJ in the later course of the treatment.
Follow-up appointments are at the discretion of the surgeon and depend on the stability of the occlusion on the first visit. If a malocclusion is noted and treatable with training elastics, weekly appointments are recommended.
The patient should be warned to continue routine follow up with their dentist. Fractures near the dental roots can often result in delayed loss of tooth viability, requiring periapical films and additional dental procedures.
Malocclusion
If a malocclusion is detected, the surgeon must ascertain its etiology (with appropriate imaging technique). If the malocclusion is secondary to surgical edema or muscle splinting, training elastics may be beneficial. The lightest elastics as possible are used for guidance, because active motion of the mandible is desirable. Patients should be shown how to place and remove the elastics using a hand mirror.
If the malocclusion is secondary to a bony problem due to inadequate reduction or hardware failure or displacement, elastic training will be of no benefit. The patient must return to the operating room for revision surgery.
Basic postoperative instructions
DietDepending upon the stability of the internal fixation, the diet can vary between liquid and semi-liquid to “as tolerated”, at the discretion of the surgeon. Any elastics are removed during eating.
Patients having only extraoral approaches are not compromised in their routine oral hygiene measures and should continue with their daily schedule.
Patients with intraoral wounds must be instructed in appropriate oral hygiene procedures. The presence of the arch-bars and any elastics makes this a more difficult procedure than normal. A soft toothbrush (dipping in warm water makes it softer) should be used to clean the surfaces of the teeth and arch-bars. Any elastics are removed for oral hygiene procedures. Chlorhexidine oral rinses should be prescribed and used at least three times each day to help sanitize the mouth. Chlorohexidine may cause staining of the teeth and should not be used longer than necessary. For larger debris, a 1:1 mixture of hydrogen peroxide (0.25%)/chlorhexidine (0.12%) can be used. The bubbling action of the hydrogen peroxide helps remove debris. A water flosser, providing a water jet, is a very useful tool to help remove debris from the wires. If a this is used, care should be taken not to direct the jet stream directly over intraoral incisions as this may lead to wound dehiscence.
Physiotherapy can be prescribed at the first visit and opening and excursive exercises begun as soon as possible. Goals should be set, and, typically, 40 mm of maximum interincisal jaw opening should be attained by 4 weeks postoperatively. If the patient cannot fully open his mouth, additional passive physical therapy may be required such as Therabite® or tongue-blade training.