Posterior short segment fixation with pedicle screws
1. Introduction
Preliminary remarks
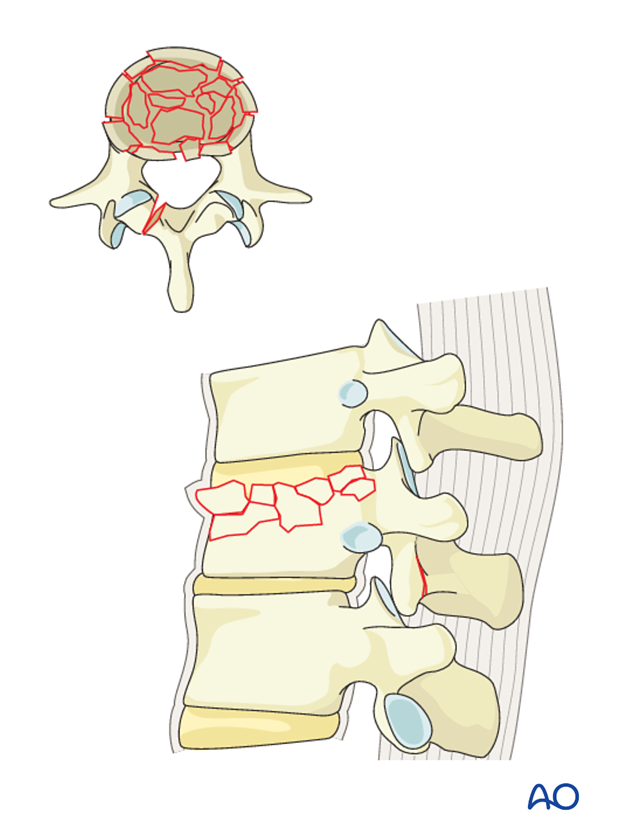
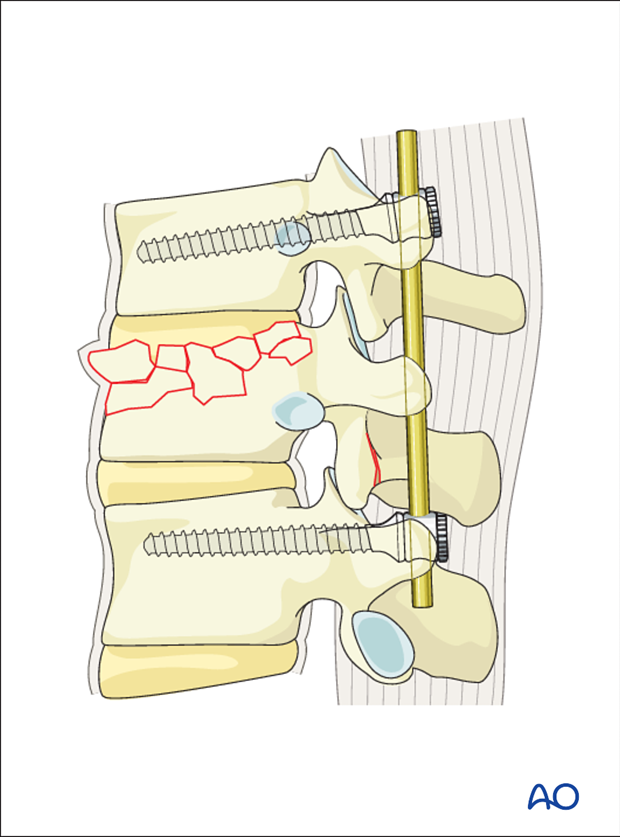
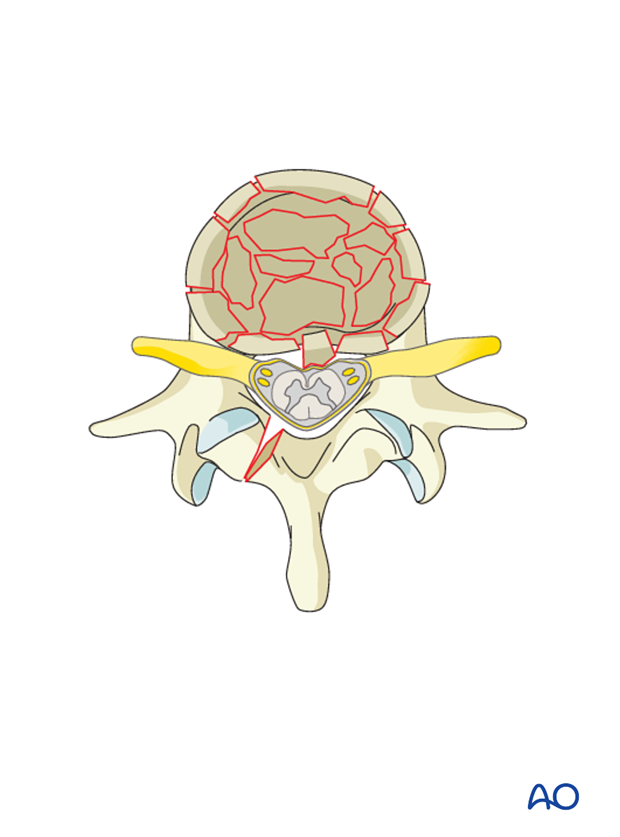
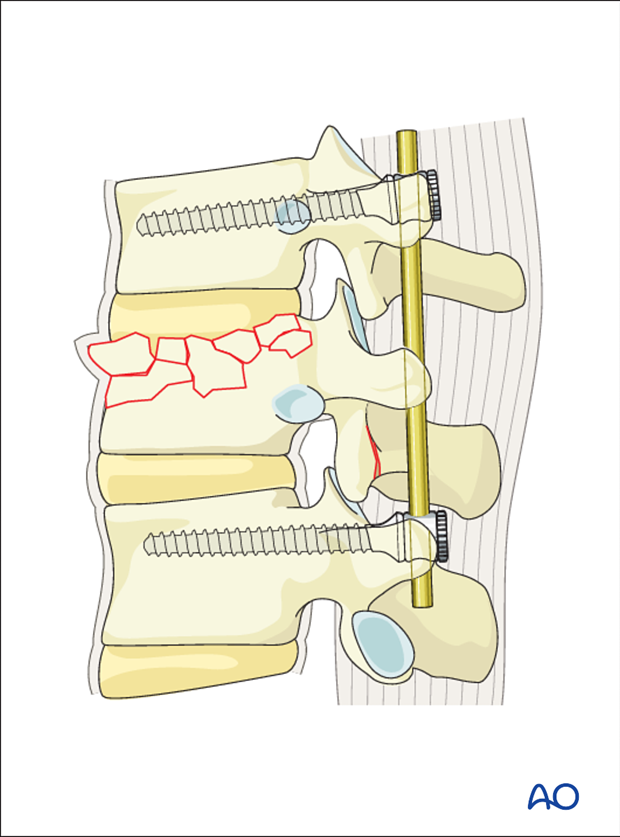
A3 injuries are compression injuries of the vertebral body involving only one endplate and associated with a fracture of the posterior wall of the vertebral body. Due to axial compression forces, vertical fracture of the lamina can be present and does not indicate a tension band failure.
Decompression
In cases where neurological deficit is observed and compression of the spinal canal is assumed, decompression has to be performed. It should be understood that this is a step that can also result in deterioration of neurology unless very meticulously performed.
Decompression can be performed anteriorly or posteriorly. Posteriorly, decompression can be indirect or direct. Indirect decompression may be tried before performing direct decompression. Please refer to Decompression techniques for a detailed discussion of indications for posterior decompression techniques.
Repair of dural laceration
More details on repair of dural laceration can be found here.
2. Patient preparation and approach
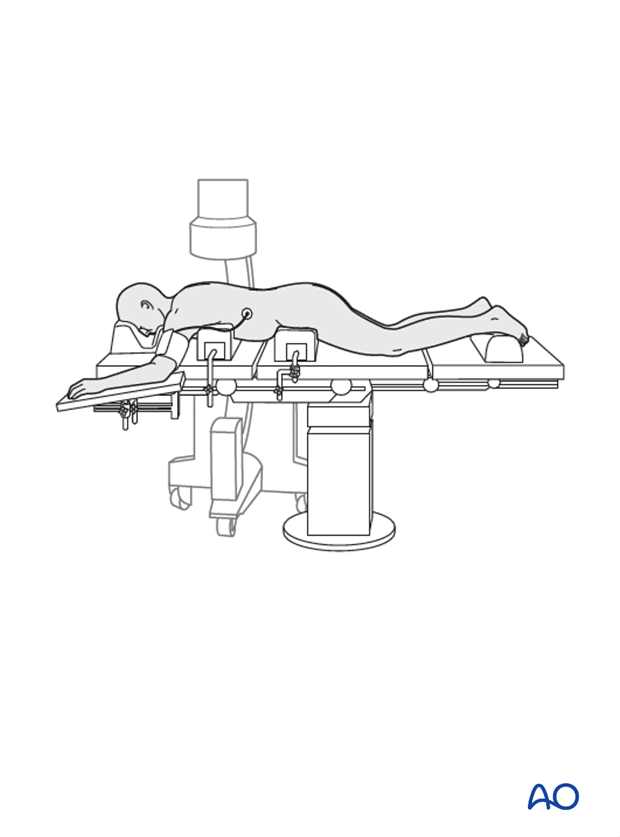
The posterior open approach to the midline is used together with the appropriate patient preparation.
3. Closed reduction
Primary reduction is performed by positioning of the patient onto a frame to create lordosis.
4. Reduction with pedicle screws
Preliminary remarks
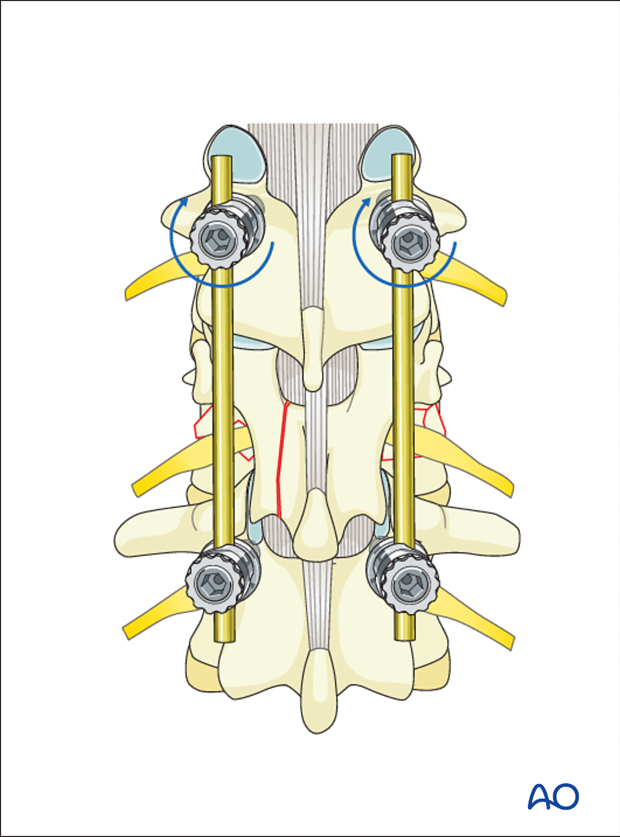
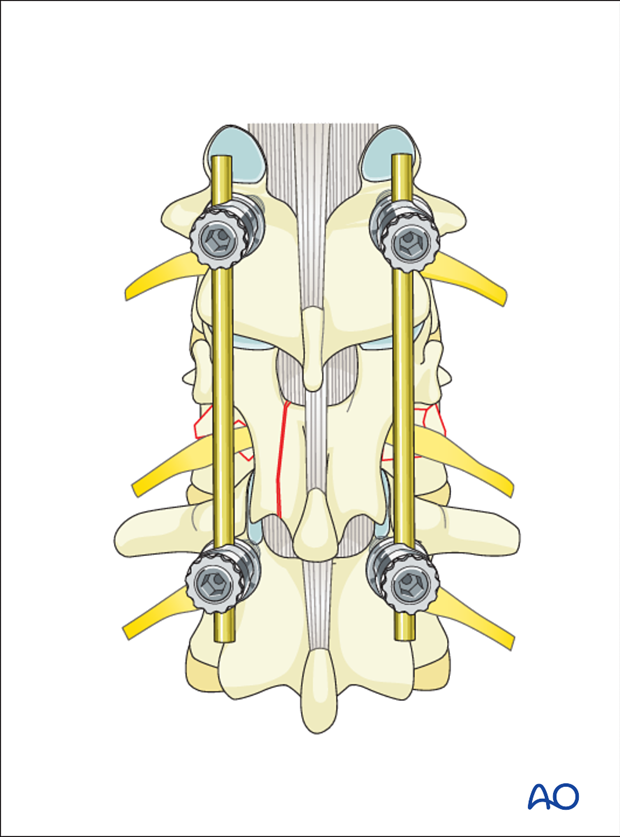
Due to the fact that bilateral instrumentation is necessary in all cases, all steps described below are repeated on the opposite side, unless described otherwise.
Pedicle screw insertion
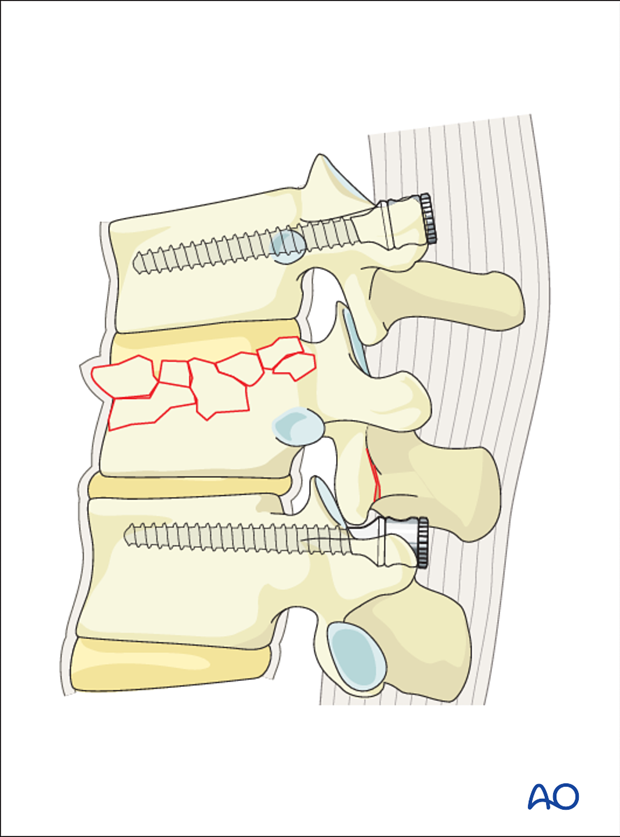
Most A3 fractures can be managed by posterior short segment fixation with pedicle screws alone.
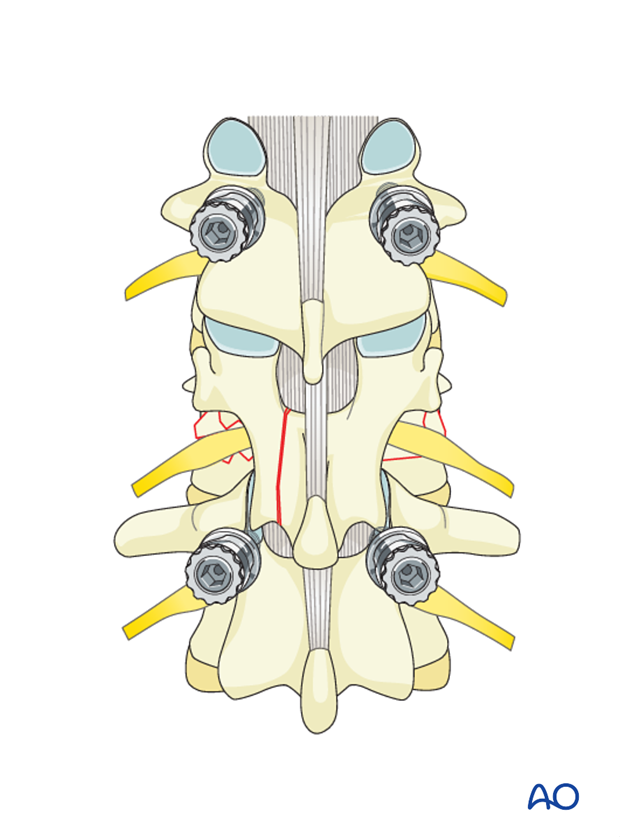
Pedicle screws are inserted into the vertebrae cephalad and caudal to the fracture level on both sides. Mono- or polyaxial, top- or side loading screws can be used in any combination.
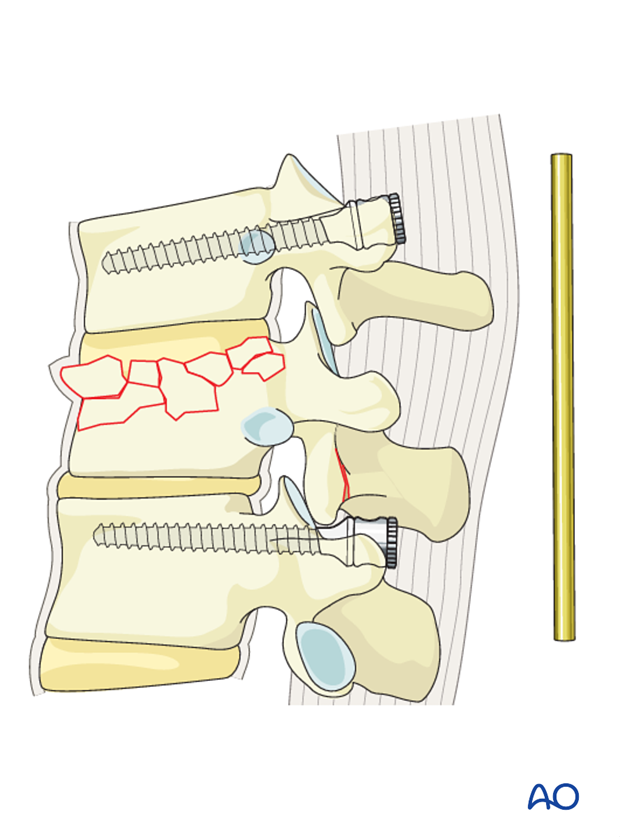
Rod contouring
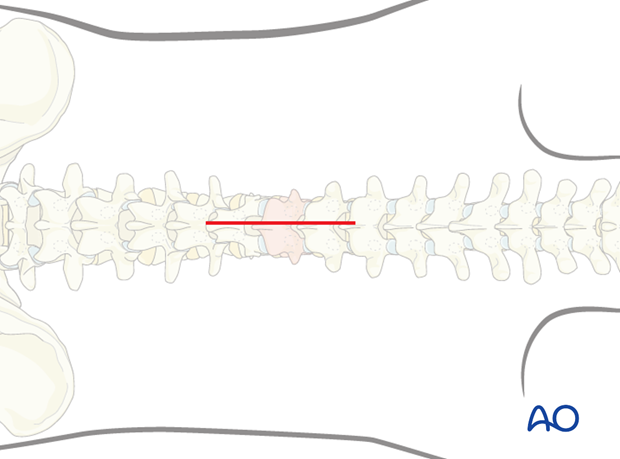
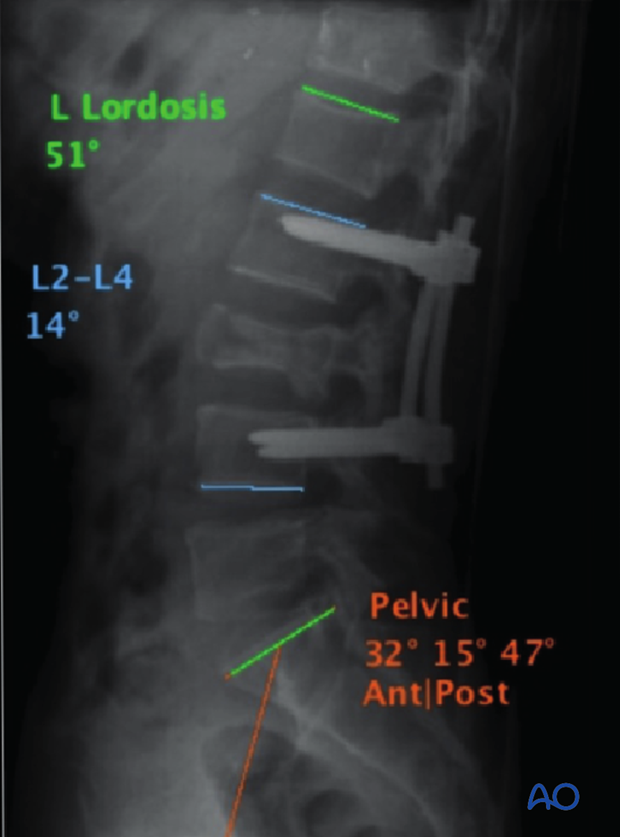
The contouring of the rod depends on the site of the fracture following the natural curvature of the spine. A rod contoured in mild kyphosis is chosen for fractures from T1-T10. A straight or a slightly lordotic rod is chosen for fractures from T11-L1 as illustrated, and a rod contoured to lordosis is chosen for lumbar fractures.
Rod insertion
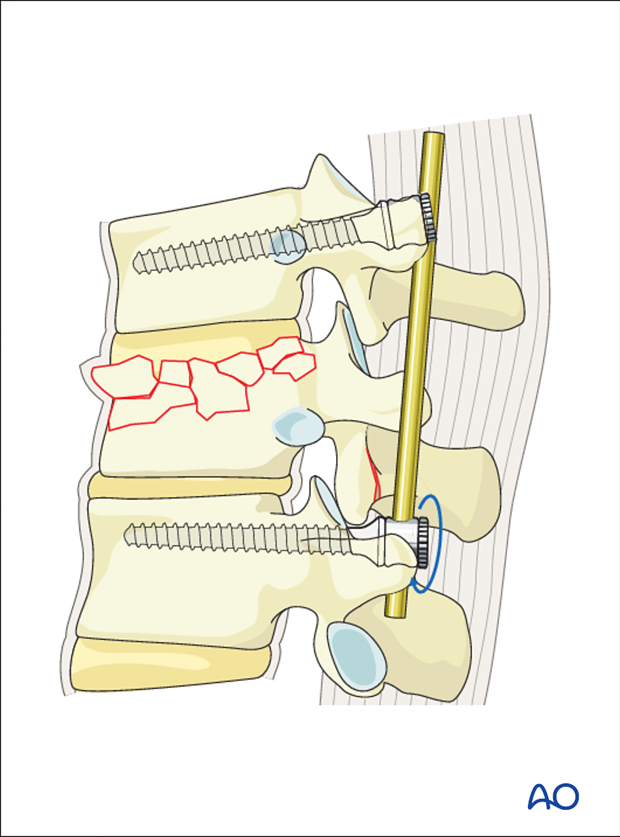
The rods are introduced to the distal screw heads on both sides and tightened.
The rod is then inserted into the proximal screw heads without tightening.
Decompression
If it is decided to perform an indirect decompression, this is done at this stage. If indirect decompression proves to be insufficient, a direct decompression eg, posterior or transpedicular decompression are undertaken. Refer to the Posterior Decompression techniques for detailed instructions. ( Posterior Decompression)
Distraction (ligamentotaxis)
With the help of a distractor, the proximal screws are distracted along the rod. This is done on both sides simultaneously.
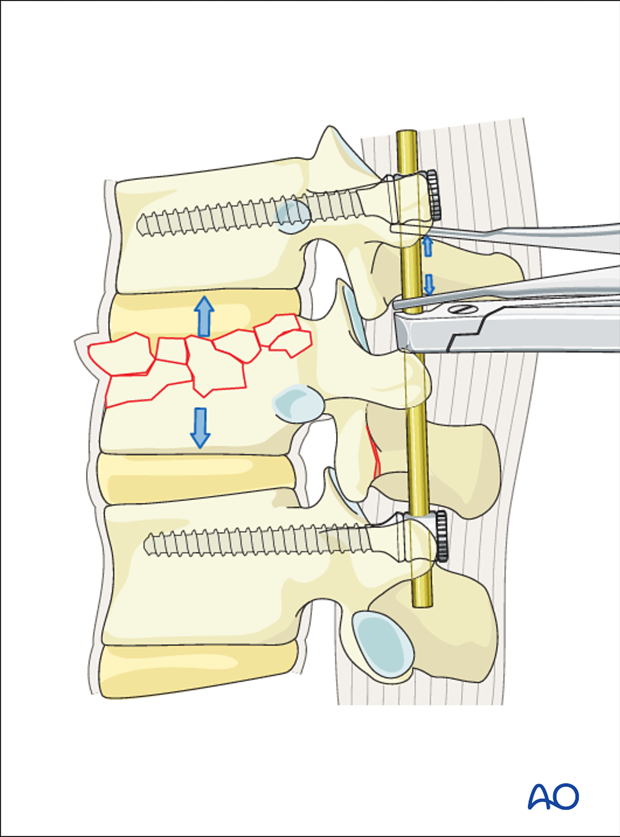
The screw heads are tightened with the inner nuts to secure the reduction achieved.
The final construct is shown from a lateral view.
5. Fusion
Decision
Although fusion was routinely performed for all spinal fractures, its indications are now being restricted to fractures that are highly unstable.
Nonfusion fixations can be performed for A3, A4, and B1 type injuries. Fusion is routinely performed for A2, B2, B3 and all C injuries as they are unstable injuries with extensive soft tissue and ligamentous disruption.
Nonfusion
For nonfusion surgeries, the facet joint capsule is preserved during the entire procedure.
The screws can be removed after 9 months once the fracture has healed.
6. Intraoperative imaging
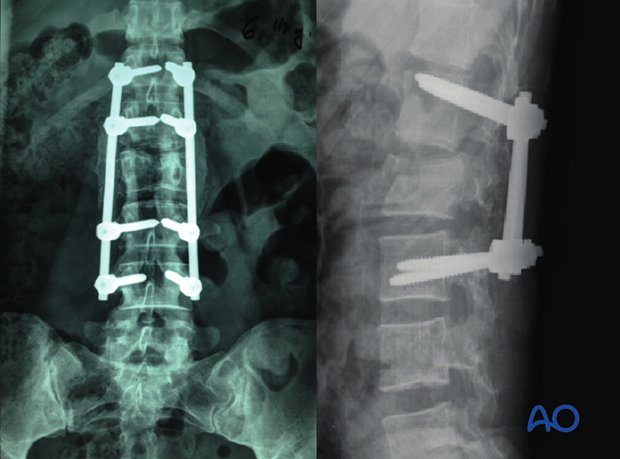
Prior to wound closure, intraoperative imaging is performed to check the adequacy of reduction, position, and length of screws and the overall coronal and sagittal spinal alignment.
7. Aftercare for posterior procedures
Patients are made to sit up in the bed on the first day after surgery. Bracing is optional. Patients with intact neurological status are made to stand and walk on the second day after surgery. Patients can be discharged when medically stable or sent to a rehabilitation center if further care is necessary. This depends on the comfort levels and presence of other associated injuries.
Patients are generally followed with periodical x-rays at 6 weeks, 3 months, 6 months, and 1 year. Normally, 5-10 degrees of loss of kyphosis can be observed within the first 6 months, which does not affect the functional outcomes. For nonfusion surgeries, the implants can be removed once fusion is confirmed.